Ann Hepatobiliary Pancreat Surg.
2022 May;26(2):125-132. 10.14701/ahbps.21-127.
Can the presence of KRAS mutations guide the type of liver resection during simultaneous resection of colorectal liver metastasis?
- Affiliations
-
- 1Department of Surgery, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 2Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2530090
- DOI: http://doi.org/10.14701/ahbps.21-127
Abstract
- Backgrounds/Aims
It is generally accepted that non-anatomical resection (NAR) in colorectal liver metastasis (CRLM) has comparable safety and efficacy compared to anatomical resection (AR); however, there are reports that AR may have better outcomes in KRAS mutated CRLM. This study aimed to determine the effects of KRAS mutations and surgical techniques on survival outcomes in CRLM patients.
Methods
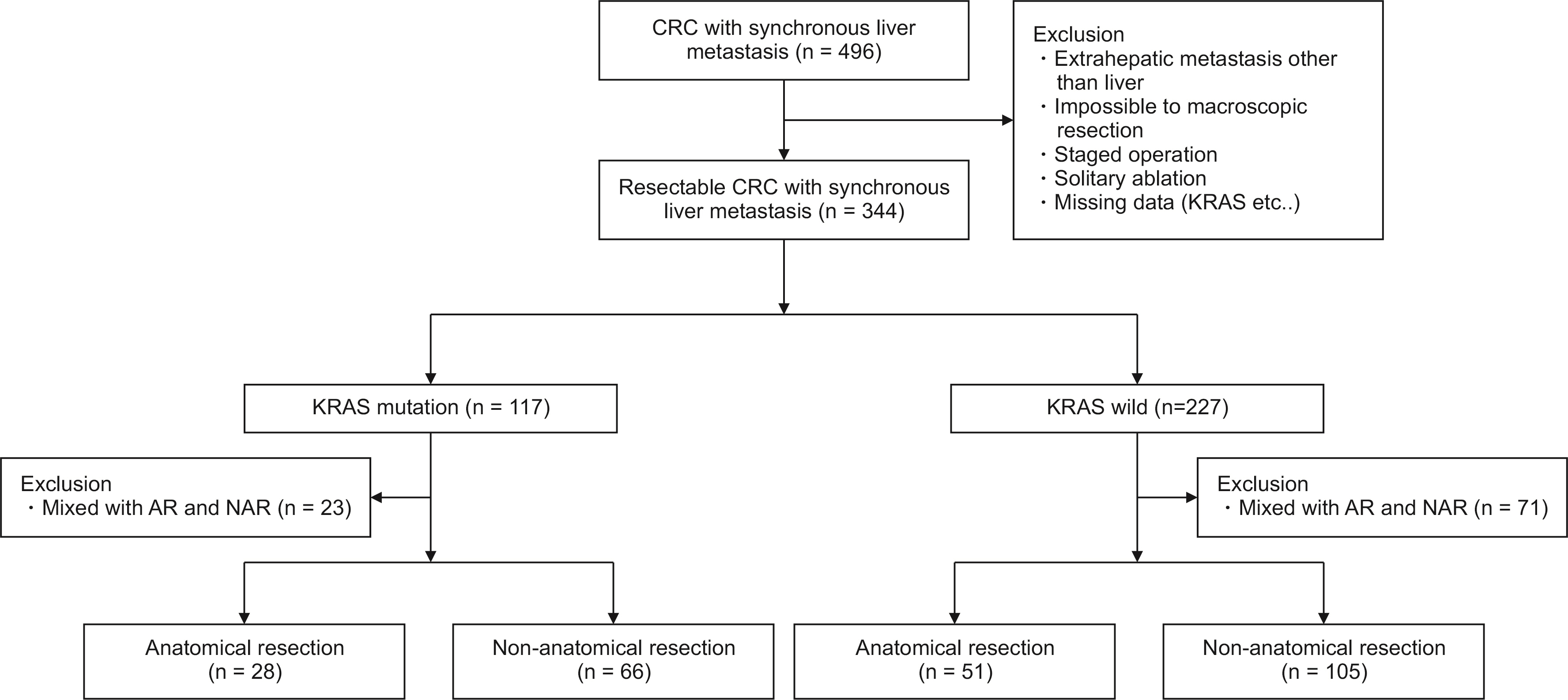
Two hundred fifty patients who underwent hepatic resection of CRLM with known KRAS mutational status between 2007 and 2018 were analyzed. A total of 94 KRAS mutated CRLM and 156 KRAS wild-type CRLM were subdivided by surgical approach and compared for short- and long-term outcomes.
Results
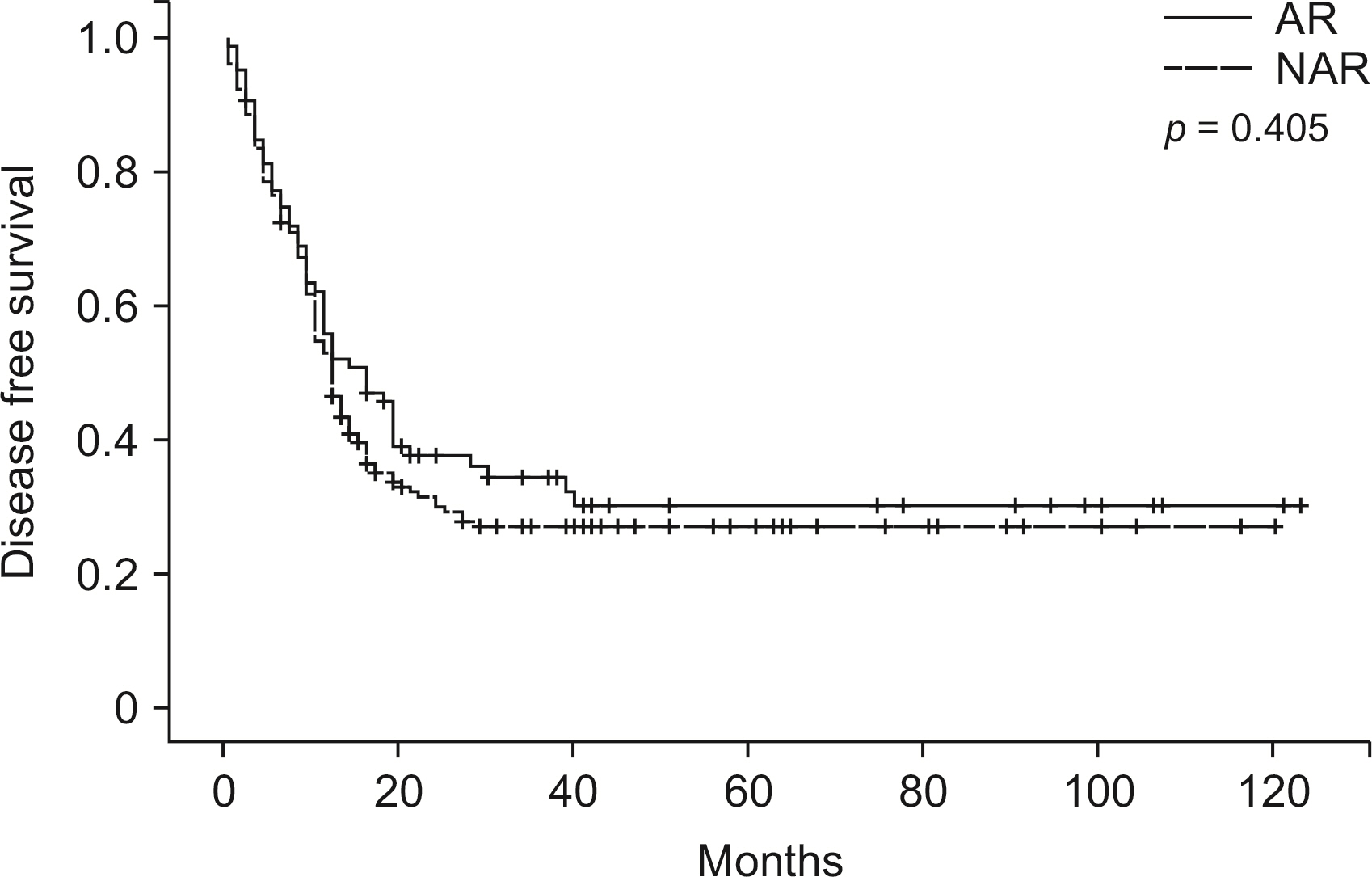
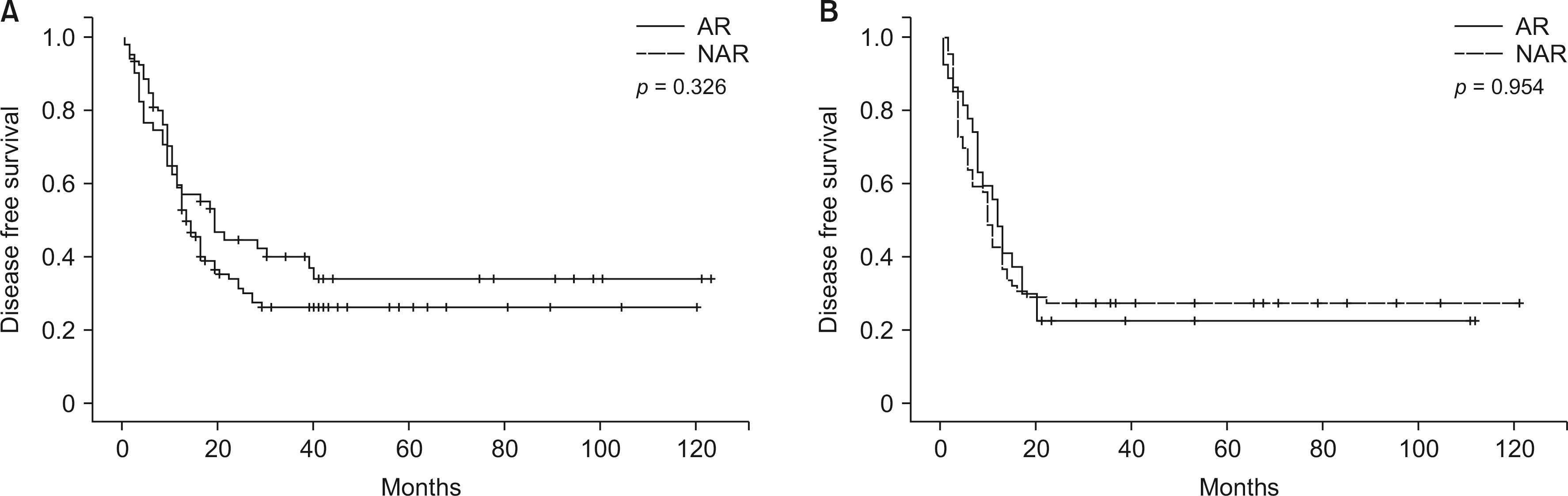
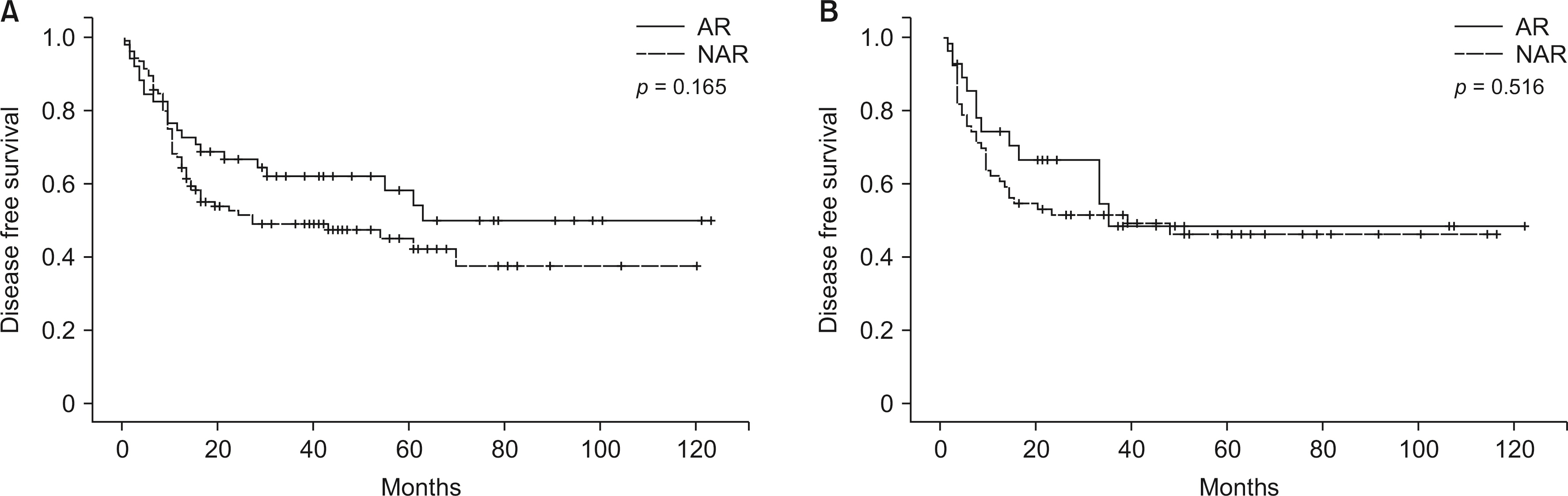
In both KRAS wild-type and mutated type, there was no difference in estimated blood loss, postoperative complications, and 30-day mortality. There was no difference in disease-free survival (DFS) between AR and NAR in both groups (p = 0.326, p = 0.954, respectively). Finally, there was no difference in intrahepatic DFS between AR and NAR groups in both the KRAS groups (p = 0.165, p = 0.516, respectively).
Conclusions
The presence of KRAS mutation may not be a significant factor when deciding the approach in simultaneous resection of CRLM.
Keyword
Figure
Cited by 1 articles
-
Primary tumor sidedness is not prognostic factor in resectable colorectal cancer liver metastasis: a retrospective observational cohort study
Sung Jun Jo, Jongman Kim, Jung Kyong Shin, Jinsoo Rhu, Jung Wook Huh, Gyu-seong Choi, Jae-Won Joh
Ann Surg Treat Res. 2024;107(5):264-273. doi: 10.4174/astr.2024.107.5.264.
Reference
-
1. Engstrand J, Nilsson H, Strömberg C, Jonas E, Freedman J. 2018; Colorectal cancer liver metastases - a population-based study on incidence, management and survival. BMC Cancer. 18:78. DOI: 10.1186/s12885-017-3925-x. PMID: 29334918. PMCID: PMC5769309.
Article2. Tsilimigras DI, Ntanasis-Stathopoulos I, Bagante F, Moris D, Cloyd J, Spartalis E, et al. 2018; Clinical significance and prognostic relevance of KRAS, BRAF, PI3K and TP53 genetic mutation analysis for resectable and unresectable colorectal liver metastases: a systematic review of the current evidence. Surg Oncol. 27:280–288. DOI: 10.1016/j.suronc.2018.05.012. PMID: 29937183.
Article3. Shindoh J, Nishioka Y, Yoshioka R, Sugawara T, Sakamoto Y, Hasegawa K, et al. 2016; KRAS mutation status predicts site-specific recurrence and survival after resection of colorectal liver metastases irrespective of location of the primary lesion. Ann Surg Oncol. 23:1890–1896. DOI: 10.1245/s10434-016-5087-5. PMID: 26786089.
Article4. Vauthey JN, Zimmitti G, Kopetz SE, Shindoh J, Chen SS, Andreou A, et al. 2013; RAS mutation status predicts survival and patterns of recurrence in patients undergoing hepatectomy for colorectal liver metastases. Ann Surg. 258:619–626. discussion 626–627. DOI: 10.1097/SLA.0b013e3182a5025a. PMID: 24018645. PMCID: PMC3856211.
Article5. Margonis GA, Sasaki K, Andreatos N, Kim Y, Merath K, Wagner D, et al. 2017; KRAS mutation status dictates optimal surgical margin width in patients undergoing resection of colorectal liver metastases. Ann Surg Oncol. 24:264–271. DOI: 10.1245/s10434-016-5609-1. PMID: 27696170.
Article6. Brudvik KW, Mise Y, Chung MH, Chun YS, Kopetz SE, Passot G, et al. 2016; RAS mutation predicts positive resection margins and narrower resection margins in patients undergoing resection of colorectal liver metastases. Ann Surg Oncol. 23:2635–2643. DOI: 10.1245/s10434-016-5187-2. PMID: 27016292. PMCID: PMC5527830.
Article7. Moris D, Ronnekleiv-Kelly S, Rahnemai-Azar AA, Felekouras E, Dillhoff M, Schmidt C, et al. 2017; Parenchymal-sparing versus anatomic liver resection for colorectal liver metastases: a systematic review. J Gastrointest Surg. 21:1076–1085. DOI: 10.1007/s11605-017-3397-y. PMID: 28364212.
Article8. Mise Y, Aloia TA, Brudvik KW, Schwarz L, Vauthey JN, Conrad C. 2016; Parenchymal-sparing hepatectomy in colorectal liver metastasis improves salvageability and survival. Ann Surg. 263:146–152. DOI: 10.1097/SLA.0000000000001194. PMID: 25775068.
Article9. Kokudo N, Tada K, Seki M, Ohta H, Azekura K, Ueno M, et al. 2001; Anatomical major resection versus nonanatomical limited resection for liver metastases from colorectal carcinoma. Am J Surg. 181:153–159. DOI: 10.1016/S0002-9610(00)00560-2. PMID: 11425058.
Article10. Lalmahomed ZS, Ayez N, van der Pool AE, Verheij J, IJzermans JN, Verhoef C. 2011; Anatomical versus nonanatomical resection of colorectal liver metastases: is there a difference in surgical and oncological outcome? World J Surg. 35:656–661. DOI: 10.1007/s00268-010-0890-9. PMID: 21161655. PMCID: PMC3032901.
Article11. Sarpel U, Bonavia AS, Grucela A, Roayaie S, Schwartz ME, Labow DM. 2009; Does anatomic versus nonanatomic resection affect recurrence and survival in patients undergoing surgery for colorectal liver metastasis? Ann Surg Oncol. 16:379–384. DOI: 10.1245/s10434-008-0218-2. PMID: 19020941.
Article12. DeMatteo RP, Palese C, Jarnagin WR, Sun RL, Blumgart LH, Fong Y. 2000; Anatomic segmental hepatic resection is superior to wedge resection as an oncologic operation for colorectal liver metastases. J Gastrointest Surg. 4:178–184. DOI: 10.1016/S1091-255X(00)80054-2. PMID: 10675241.
Article13. Margonis GA, Buettner S, Andreatos N, Sasaki K, Ijzermans JNM, van Vugt JLA, et al. 2017; Anatomical resections improve disease-free survival in patients with KRAS-mutated colorectal liver metastases. Ann Surg. 266:641–649. DOI: 10.1097/SLA.0000000000002367. PMID: 28657938.
Article14. Kye BH, Lee SH, Jeong WK, Yu CS, Park IJ, Kim HR, et al. 2019; Which strategy is better for resectable synchronous liver metastasis from colorectal cancer, simultaneous surgery, or staged surgery? Multicenter retrospective analysis. Ann Surg Treat Res. 97:184–193. DOI: 10.4174/astr.2019.97.4.184. PMID: 31620392. PMCID: PMC6779956.
Article15. Abelson JS, Michelassi F, Sun T, Mao J, Milsom J, Samstein B, et al. 2017; Simultaneous resection for synchronous colorectal liver metastasis: the new standard of care? J Gastrointest Surg. 21:975–982. DOI: 10.1007/s11605-017-3422-1. PMID: 28411351.
Article16. Boudjema K, Locher C, Sabbagh C, Ortega-Deballon P, Heyd B, Bachellier P, et al. 2021; Simultaneous versus delayed resection for initially resectable synchronous colorectal cancer liver metastases: a prospective, open-label, randomized, controlled trial. Ann Surg. 273:49–56. DOI: 10.1097/SLA.0000000000003848. PMID: 32209911.
Article17. Majno P, Mentha G, Toso C, Morel P, Peitgen HO, Fasel JH. 2014; Anatomy of the liver: an outline with three levels of complexity--a further step towards tailored territorial liver resections. J Hepatol. 60:654–662. DOI: 10.1016/j.jhep.2013.10.026. PMID: 24211738.
Article18. Kaibori M, Kon M, Kitawaki T, Kawaura T, Hasegawa K, Kokudo N, et al. 2017; Comparison of anatomic and non-anatomic hepatic resection for hepatocellular carcinoma. J Hepatobiliary Pancreat Sci. 24:616–626. DOI: 10.1002/jhbp.502. PMID: 28887834.
Article19. Navarro J, Rho SY, Kang I, Choi GH, Min BS. 2019; Robotic simultaneous resection for colorectal liver metastasis: feasibility for all types of liver resection. Langenbecks Arch Surg. 404:895–908. DOI: 10.1007/s00423-019-01833-7. PMID: 31797029.
Article20. Choi SH, Choi GH, Han DH, Choi JS. 2015; Laparoscopic liver resection using a rubber band retraction technique: usefulness and perioperative outcome in 100 consecutive cases. Surg Endosc. 29:387–397. DOI: 10.1007/s00464-014-3680-x. PMID: 24986021.
Article21. Gavriilidis P, Sutcliffe RP, Hodson J, Marudanayagam R, Isaac J, Azoulay D, et al. 2018; Simultaneous versus delayed hepatectomy for synchronous colorectal liver metastases: a systematic review and meta-analysis. HPB (Oxford). 20:11–19. DOI: 10.1016/j.hpb.2017.08.008. PMID: 28888775.
Article22. Torzilli G, Viganò L, Gatti A, Costa G, Cimino M, Procopio F, et al. 2017; Twelve-year experience of "radical but conservative" liver surgery for colorectal metastases: impact on surgical practice and oncologic efficacy. HPB (Oxford). 19:775–784. DOI: 10.1016/j.hpb.2017.05.006. PMID: 28625391.
Article23. Margonis GA, Buettner S, Andreatos N, Wagner D, Sasaki K, Barbon C, et al. 2019; Prognostic factors change over time after hepatectomy for colorectal liver metastases: a multi-institutional, international analysis of 1099 patients. Ann Surg. 269:1129–1137. DOI: 10.1097/SLA.0000000000002664. PMID: 31082912.
Article24. Tomlinson JS, Jarnagin WR, DeMatteo RP, Fong Y, Kornprat P, Gonen M, et al. 2007; Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol. 25:4575–4580. DOI: 10.1200/JCO.2007.11.0833. PMID: 17925551.
Article25. Yin Z, Liu C, Chen Y, Bai Y, Shang C, Yin R, et al. 2013; Timing of hepatectomy in resectable synchronous colorectal liver metastases (SCRLM): simultaneous or delayed? Hepatology. 57:2346–2357. DOI: 10.1002/hep.26283. PMID: 23359206.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Simultaneous Laparoscopy-Assisted Resection for Colorectal Cancer and Metastases
- Resection of Colorectal Liver Metastases
- Liver Metastases in Colorectal Cancer
- Treatment of Liver Metastases
- Simultaneous resection of synchronous colorectal liver metastasis: Feasibility and development of a prediction model