J Korean Med Sci.
2022 May;37(19):e153. 10.3346/jkms.2022.37.e153.
The Impact of the Amendment of the Health Insurance Coverage for F-18 Fluorodeoxyglucose Positron Emission Tomography on the Healthcare Behaviors for Breast Cancer: An Interrupted Time Series Analysis of the Korean National Data From 2013 to 2018
- Affiliations
-
- 1Department of Nuclear Medicine, Chungbuk National University Hospital, Cheongju, Korea
- 2Department of Research and Analysis, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 3Department of Health Administration and Management, College of Medical Science, Soonchunhyang University, Asan, Korea
- 4Healthcare Review and Assessment Committee, Health Insurance Review and Assessment Service, Wonju, Korea
- 5Quality Assessment Department, Health Insurance Review and Assessment Service, Wonju, Korea
- 6Quality Assessment Administration Department, Health Insurance Review and Assessment Service, Wonju, Korea
- 7Department of Internal Medicine, University of Nevada Las Vegas School of Medicine, Las Vegas, NV, USA
- 8Division of Breast and Endocrine Surgery, Department of Surgery, Korea University Ansan Hospital, Ansan, Korea
- 9Department of Nuclear Medicine, Seoul National University College of Medicine, Seoul, Korea
- 10Cancer Research Institute, Seoul National University, Seoul, Korea
- 11Bio-MAX Institute, Seoul National University, Seoul, Korea
- 12Department of Thoracic and Cardiovascular Surgery, Korea University Ansan Hospital, Ansan, Korea
- KMID: 2529771
- DOI: http://doi.org/10.3346/jkms.2022.37.e153
Abstract
- Background
F-18 Fluorodeoxyglucose positron emission tomography (F-18 FDG PET), which can cover the body from the skull base to the thigh in one scan, is beneficial for evaluating distant metastasis. F-18 FDG PET has interested policymakers because of its relatively high cost. This study investigated the effect of the F-18 FDG PET reimbursement criteria amendment on healthcare behavior in breast cancer using an interrupted time series (ITS) analysis.
Methods
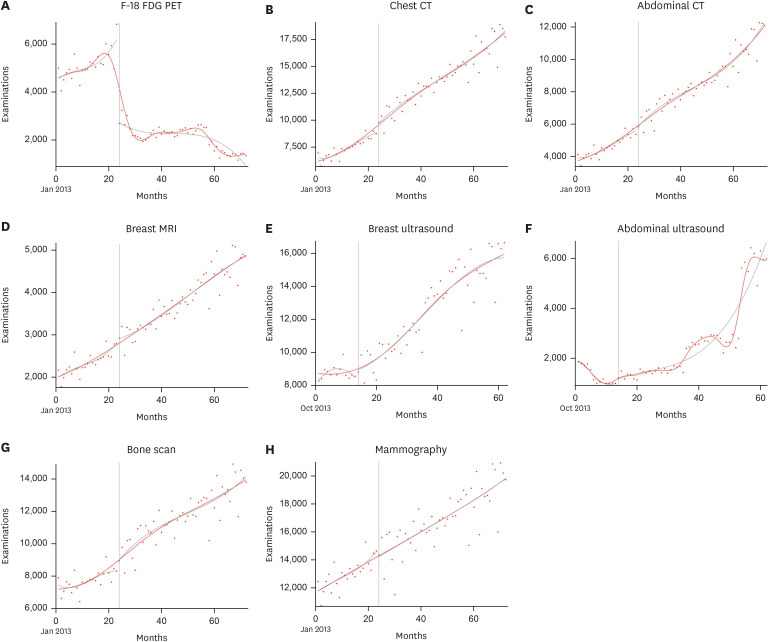
We retrospectively analyzed the inpatient and outpatient data from Korea’s Health Insurance Review and Assessment Service (HIRA) from January 1, 2013 to December 31, 2018. ITS analysis was performed for the number of each medical imaging modality and the total medical imaging cost of the breast cancer patients.
Results
The annual number of breast cancer patients has been increasing steadily since 2013. The trend of F-18 FDG PET increased before the reimbursement criteria was amended, but intensely decreased immediately thereafter. The chest and abdomen computed tomography scans showed a statistically significant increase immediately after the amendment and kept steadily increasing. A change in the total medical imaging cost for the breast cancer patient claimed every month showed an increasing trend before the amendment (β = 5,475, standard error [SE] = 1,992, P = 0.008) and rapid change immediately after (β = −103,317, SE = 16,152, P < 0.001). However, there was no significant change in the total medical imaging cost at the long-term follow-up (β = −912, SE = 1,981, P = 0.647).
Conclusion
Restriction of health insurance coverage for cancer may affect healthcare behaviors. To compensate for it, the policymakers must consider this and anticipate the impact following implementation.
Keyword
Figure
Reference
-
1. Eubank WB, Mankoff DA. Evolving role of positron emission tomography in breast cancer imaging. Semin Nucl Med. 2005; 35(2):84–99. PMID: 15765372.2. Han S, Choi JY. Impact of 18F-FDG PET, PET/CT, and PET/MRI on staging and management as an initial staging modality in breast cancer: a systematic review and meta-analysis. Clin Nucl Med. 2021; 46(4):271–282. PMID: 33651022.3. Ulaner GA. PET/CT for patients with breast cancer: where Is the clinical impact? AJR Am J Roentgenol. 2019; 213(2):254–265. PMID: 31063423.4. Kim L, Kim JA, Kim S. A guide for the utilization of health insurance review and assessment service national patient samples. Epidemiol Health. 2014; 36:e2014008. PMID: 25078381.5. Mahamat A, MacKenzie FM, Brooker K, Monnet DL, Daures JP, Gould IM. Impact of infection control interventions and antibiotic use on hospital MRSA: a multivariate interrupted time-series analysis. Int J Antimicrob Agents. 2007; 30(2):169–176. PMID: 17560085.6. Young JM, Stacey I, Dobbins TA, Dunlop S, Dessaix AL, Currow DC. Association between tobacco plain packaging and Quitline calls: a population-based, interrupted time-series analysis. Med J Aust. 2014; 200(1):29–32. PMID: 24438415.7. Alshamsan R, Lee JT, Majeed A, Netuveli G, Millett C. Effect of a UK pay-for-performance program on ethnic disparities in diabetes outcomes: interrupted time series analysis. Ann Fam Med. 2012; 10(3):228–234. PMID: 22585887.8. Kim J, Han J, Chun BC. Trends of internet search volumes for major depressive disorder symptoms during the COVID-19 pandemic in Korea: an interrupted time-series analysis. J Korean Med Sci. 2022; 37(14):e108. PMID: 35411728.9. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017; 46(1):348–355. PMID: 27283160.10. Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974; 9(3):208–220. PMID: 4436074.11. Card D, Dobkin C, Maestas N. The impact of nearly universal insurance coverage on health care utilization: evidence from Medicare. Am Econ Rev. 2008; 98(5):2242–2258. PMID: 19079738.12. Kim SJ, Han KT, Park EC, Park S, Kim TH. Copayment policy effects on healthcare spending and utilization by Korean lung cancer patients at end of life: a retrospective cohort design 2003-2012. Asian Pac J Cancer Prev. 2014; 15(13):5265–5270. PMID: 25040986.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Whole Body Positron Emission Tomography/Computed Tomography
- Unexpected Second Primary Malignancies Detected by F-18 FDG PET/CT During Follow-up for Primary Malignancy: Two Case Reports
- Improving Causal Inference in Observational Studies: Interrupted Time Series Design
- National Statistics of Endoscopic Submucosal Dissection for Early Gastric Cancer in Korea
- Random Synchronous Malignancy in Male Breast: A Case Report