Intest Res.
2022 Apr;20(2):231-239. 10.5217/ir.2021.00056.
Efficacy and tolerability of hyperbaric oxygen therapy in small bowel stricturing Crohn’s disease: a pilot study
- Affiliations
-
- 1Department of Gastroenterology, All India Institute of Medical Sciences, New Delhi, India
- 2Department of Anesthesia, All India Institute of Medical Sciences, New Delhi, India
- 3Department of Plastic Surgery, All India Institute of Medical Sciences, New Delhi, India
- 4Department of Radiology, All India Institute of Medical Sciences, New Delhi, India
- KMID: 2529569
- DOI: http://doi.org/10.5217/ir.2021.00056
Abstract
- Background/Aims
Existing therapeutic options for complicated Crohn’s disease (CD) like biologics and surgery are limited by inadequate long-term efficacy, cost, and adverse effects. Tissue hypoxia is important in CD pathogenesis and may be ameliorated with hyperbaric oxygen therapy (HBOT). We assessed the efficacy and tolerability of HBOT in small bowel stricturing CD.
Methods
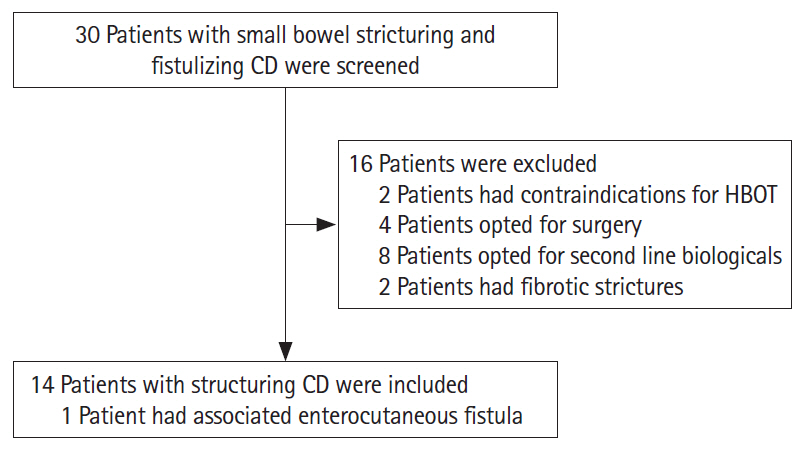
This pilot study included patients of small bowel stricturing CD (from April 2019 to January 2020) who underwent HBOT. These patients were refractory to conventional medical treatment or had multiple strictures not amenable to resection. Each session of HBOT was given for 60 minutes with a pressure of 1.5–2.5 atm. Clinical, biochemical responses and Short Inflammatory Bowel Disease (SIBD) questionnaire were evaluated at 2 and 6 months, and radiological response was evaluated at 6 months.
Results
Fourteen patients (mean age, 42.9±15.7 years; male, 50%) were subjected to 168 HBOT sessions. Thirteen patients (92.7%) had strictures and 1 patient had enterocutaneous fistula in addition. Median number of HBOT sessions was 11 (range, 3–20) which were administered over a median of 4 weeks. Most patients tolerated it well except 1 who had hemotympanum. At 2 and 6 months of follow-up, 64.2% of patients had a clinical response, 50% and 64.2% of patients had clinical remission respectively. Steroid-free clinical remission was seen in 8 (57%) of patients with radiological improvement in 50%. There was a significant improvement in SIBD scores at 2-month follow-up (59.4 vs. 44.5, P=0.03).
Conclusions
HBOT can be a safe and effective therapeutic option in patients with stricturing small bowel CD refractory to conventional medical treatment.
Figure
Reference
-
1. Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn’s disease. Lancet. 2017; 389:1741–1755.
Article2. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54.
Article3. Ng SC, Bernstein CN, Vatn MH, et al. Geographical variability and environmental risk factors in inflammatory bowel disease. Gut. 2013; 62:630–649.
Article4. Thia KT, Sandborn WJ, Harmsen WS, Zinsmeister AR, Loftus EV Jr. Risk factors associated with progression to intestinal complications of Crohn’s disease in a population-based cohort. Gastroenterology. 2010; 139:1147–1155.
Article5. Ma C, Moran GW, Benchimol EI, et al. Surgical rates for Crohn’s disease are decreasing: a population-based time trend analysis and validation study. Am J Gastroenterol. 2017; 112:1840–1848.
Article6. Fu YT, Hong T, Round A, Bressler B. Impact of medical therapy on patients with Crohn’s disease requiring surgical resection. World J Gastroenterol. 2014; 20:11808–11814.
Article7. Jeuring SF, van den Heuvel TR, Liu LY, et al. Improvements in the long-term outcome of Crohn’s disease over the past two decades and the relation to changes in medical management: results from the population-based IBDSL cohort. Am J Gastroenterol. 2017; 112:325–336.
Article8. Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn’s disease. Gastroenterology. 1990; 99:956–963.
Article9. Furuta GT, Turner JR, Taylor CT, et al. Hypoxia-inducible factor 1-dependent induction of intestinal trefoil factor protects barrier function during hypoxia. J Exp Med. 2001; 193:1027–1034.
Article10. Clambey ET, McNamee EN, Westrich JA, et al. Hypoxia-inducible factor-1 alpha-dependent induction of FoxP3 drives regulatory T-cell abundance and function during inflammatory hypoxia of the mucosa. Proc Natl Acad Sci U S A. 2012; 109:E2784–E2793.
Article11. Dulai PS, Gleeson MW, Taylor D, Holubar SD, Buckey JC, Siegel CA. Systematic review: the safety and efficacy of hyperbaric oxygen therapy for inflammatory bowel disease. Aliment Pharmacol Ther. 2014; 39:1266–1275.
Article12. Dulai PS, Buckey JC Jr, Raffals LE, et al. Hyperbaric oxygen therapy is well tolerated and effective for ulcerative colitis patients hospitalized for moderate-severe flares: a phase 2A pilot multi-center, randomized, double-blind, sham-controlled trial. Am J Gastroenterol. 2018; 113:1516–1523.
Article13. Fahad H, Dulai PS, Shen B, Kochhar GS. Hyperbaric oxygen therapy is effective in the treatment of inflammatory and fistulizing pouch complications. Clin Gastroenterol Hepatol. 2021; 19:1288–1291.
Article14. Irvine EJ, Zhou Q, Thompson AK. The Short Inflammatory Bowel Disease Questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn’s Relapse Prevention Trial. Am J Gastroenterol. 1996; 91:1571–1578.15. Van Assche G, Dignass A, Panes J, et al. The second European evidence-based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. J Crohns Colitis. 2010; 4:7–27.
Article16. Best WR, Becktel JM, Singleton JW, Kern F Jr. Development of a Crohn’s Disease Activity Index. National Cooperative Crohn’s Disease Study. Gastroenterology. 1976; 70:439–444.17. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753.
Article18. Rieder F, Bettenworth D, Ma C, et al. An expert consensus to standardise definitions, diagnosis and treatment targets for anti-fibrotic stricture therapies in Crohn’s disease. Aliment Pharmacol Ther. 2018; 48:347–357.
Article19. Feuerstein JD, Ho EY, Shmidt E, et al. AGA clinical practice guidelines on the medical management of moderate to severe luminal and perianal fistulizing Crohn’s disease. Gastroenterology. 2021; 160:2496–2508.20. Makanyanga JC, Pendsé D, Dikaios N, et al. Evaluation of Crohn’s disease activity: initial validation of a magnetic resonance enterography global score (MEGS) against faecal calprotectin. Eur Radiol. 2014; 24:277–287.
Article21. Hasan B, Yim Y, Ur Rashid M, et al. Hyperbaric oxygen therapy in chronic inflammatory conditions of the pouch. Inflamm Bowel Dis. 2021; 27:965–970.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of radiation-induced cystitis with hyperbaric oxygen
- A Basic Survey for Regional Capability of Hyperbaric Oxygen Therapy to Multiple Fire Victims
- Risk of surgery in patients with stricturing type of Crohn's disease at the initial diagnosis: a single center experience
- Early experience of hyperbaric oxygen therapy in radiation-induced cystitis
- Current status of endoscopic balloon dilation for Crohn's disease