Intest Res.
2022 Apr;20(2):184-191. 10.5217/ir.2020.00104.
Addition of computed tomography chest increases the diagnosis rate in patients with suspected intestinal tuberculosis
- Affiliations
-
- 1Department of Gastroenterology and Human Nutrition, All India Institute of Medical Sciences, New Delhi, India
- 2Department of Radiodiagnosis, All India Institute of Medical Sciences, New Delhi, India
- 3Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
- 4Department of Pulmonary Medicine, All India Institute of Medical Sciences, New Delhi, India
- KMID: 2529564
- DOI: http://doi.org/10.5217/ir.2020.00104
Abstract
- Background/Aims
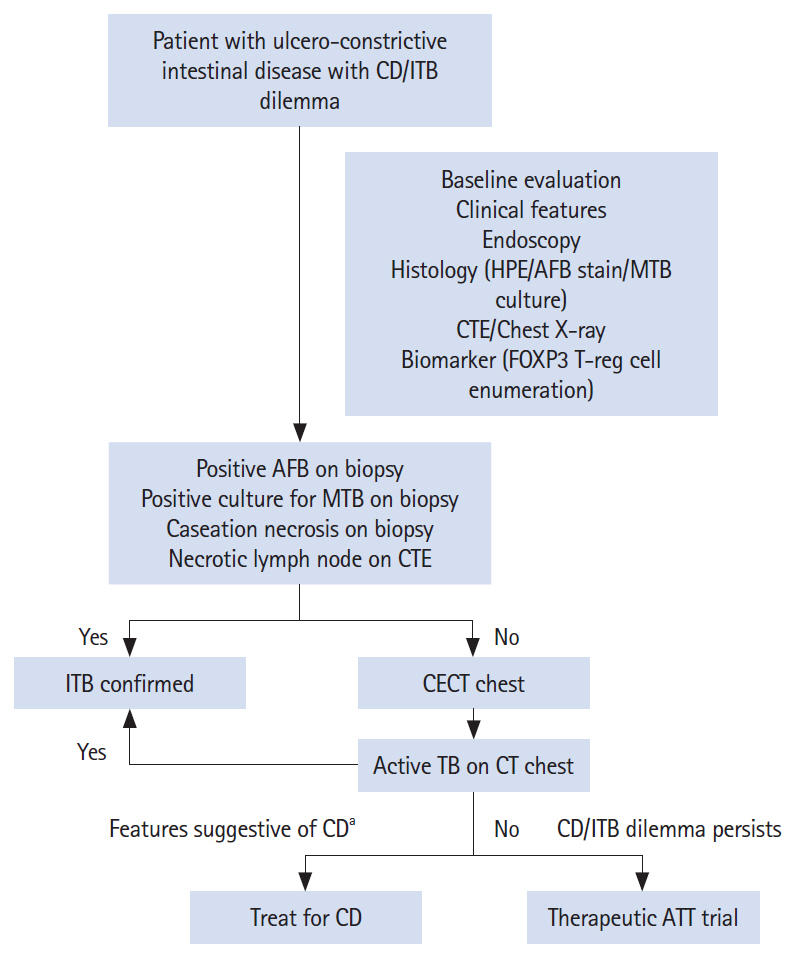
Intestinal tuberculosis (ITB) is difficult to diagnose due to poor sensitivity of definitive diagnostic tests. ITB may be associated with concomitant pulmonary tuberculosis (PTB) which may remain undetected on chest X-ray. We assessed the role of contrast enhanced computed tomography (CECT) chest in detecting the prevalence of active PTB, and increasing the diagnostic yield in patients with suspected ITB.
Methods
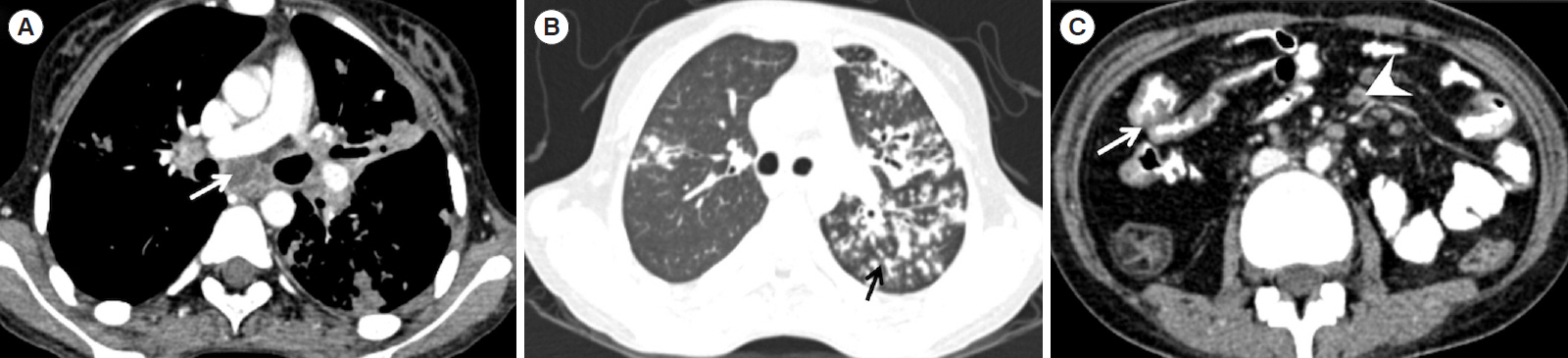
Consecutive treatment naïve patients with suspected ITB (n=200) who underwent CECT chest (n=88) and had follow-up duration>1 year were recruited in this retrospective study (February 2016 to October 2018). ITB was diagnosed in the presence of caseating granuloma, positive acid fast stain or culture for Mycobacterium tuberculosis on biopsy, presence of necrotic lymph nodes (LNs) on CT enterography or positive response to anti-tubercular therapy. Evidence of active tuberculosis on CECT-chest was defined as presence of centrilobular nodules with or without consolidation/miliary nodules/thick-walled cavity/enlarged necrotic mediastinal LNs.
Results
Sixty-five of eighty-eight patients (mean age, 33.8±12.8 years; 47.7% of females) were finally diagnosed as ITB (4-caseating granuloma on biopsy, 12-necrotic LNs on CT enterography, 1-both, and 48-response to anti-tubercular therapy) and 23 were diagnosed as Crohn’s disease. Findings of active TB on CECT chest with or without necrotic abdominal LNs were demonstrated in 5 and 20 patients, respectively. No patient with Crohn’s disease had necrotic abdominal LNs or active PTB. Addition of CECT chest in the diagnostic algorithm improved the sensitivity of ITB diagnosis from 26.2% to 56.9%.
Conclusions
Addition of CECT chest significantly improves the sensitivity for definite diagnosis in a patient with suspected ITB.
Figure
Reference
-
1. Logan VS. Anorectal tuberculosis. Proc R Soc Med. 1969; 62:1227–1230.2. Singh P, Ananthakrishnan A, Ahuja V. Pivot to Asia: inflammatory bowel disease burden. Intest Res. 2017; 15:138–141.
Article3. Pratap Mouli V, Munot K, Ananthakrishnan A, et al. Endoscopic and clinical responses to anti-tubercular therapy can differentiate intestinal tuberculosis from Crohn’s disease. Aliment Pharmacol Ther. 2017; 45:27–36.
Article4. Gupta A, Pratap Mouli V, Mohta S, et al. Antitubercular therapy given to differentiate Crohn’s disease from intestinal tuberculosis predisposes to stricture formation. J Crohns Colitis. 2020; 14:1611–1618.
Article5. Sharma MP, Bhatia V. Abdominal tuberculosis. Indian J Med Res. 2004; 120:305–315.6. Raniga S, Parikh N, Arora A, Vaghani M, Vora PA, Vaidya V. Is HRCT reliable in determining disease activity in pulmonary tuberculosis? Indian J Radiol Imaging. 2006; 16:221–228.
Article7. Alkabab YM, Enani MA, Indarkiri NY, Heysell SK. Performance of computed tomography versus chest radiography in patients with pulmonary tuberculosis with and without diabetes at a tertiary hospital in Riyadh, Saudi Arabia. Infect Drug Resist. 2018; 11:37–43.
Article8. Nachiappan AC, Rahbar K, Shi X, et al. Pulmonary tuberculosis: role of radiology in diagnosis and management. Radiographics. 2017; 37:52–72.
Article9. Paustian F. Tuberculosis of the intestine. In : Haubrich WS, Schaffner F, Berk JE, editors. Bockus gastroenterology. 5th ed. Philadelphia: Saunders;1995. p. 3304.10. Sharma SK, Mohan A. Extrapulmonary tuberculosis. Indian J Med Res. 2004; 120:316–353.
Article11. Du J, Ma YY, Xiang H, Li YM. Confluent granulomas and ulcers lined by epithelioid histiocytes: new ideal method for differentiation of ITB and CD? A meta analysis. PLoS One. 2014; 9:e103303.
Article12. Kedia S, Sharma R, Sreenivas V, et al. Accuracy of computed tomographic features in differentiating intestinal tuberculosis from Crohn’s disease: a systematic review with meta-analysis. Intest Res. 2017; 15:149–159.
Article13. Tiwari V, Kedia S, Garg SK, et al. CD4+ CD25+ FOXP3+ T cell frequency in the peripheral blood is a biomarker that distinguishes intestinal tuberculosis from Crohn’s disease. PLoS One. 2018; 13:e0193433.
Article14. Rampal R, Kedia S, Wari MN, et al. Prospective validation of CD4+CD25+FOXP3+ T-regulatory cells as an immunological marker to differentiate intestinal tuberculosis from Crohn’s disease. Intest Res. 2021; 19:232–238.
Article15. Yadav DP, Madhusudhan KS, Kedia S, et al. Development and validation of visceral fat quantification as a surrogate marker for differentiation of Crohn’s disease and intestinal tuberculosis. J Gastroenterol Hepatol. 2017; 32:420–426.
Article16. Sharma SK, Ryan H, Khaparde S, et al. Index-TB guidelines: guidelines on extrapulmonary tuberculosis for India. Indian J Med Res. 2017; 145:448–463.17. Kedia S, Das P, Madhusudhan KS, et al. Differentiating Crohn’s disease from intestinal tuberculosis. World J Gastroenterol. 2019; 25:418–432.
Article18. Limsrivilai J, Shreiner AB, Pongpaibul A, et al. Meta-analytic bayesian model for differentiating intestinal tuberculosis from Crohn’s disease. Am J Gastroenterol. 2017; 112:415–427.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Acute Appendicitis due to Intestinal Stricture after Intestinal Tuberculosis Treatment
- AIDS Diagnosed in the Course of Managing Duodenal Fistula Caused by Tuberculosis: A Case Report
- Diagnosis of Pulmonary Tuberculosis: Recent Advances and Diagnostic Algorithms
- Intestinal Tuberculosis Mimicking Colon Cancer
- Extraintestinal Tuberculosis is Useful for Differential Diagnosis of Intestinal Tuberculosis