Endocrinol Metab.
2022 Apr;37(2):281-289. 10.3803/EnM.2021.1333.
Graves’ Disease and the Risk of End-Stage Renal Disease: A Korean Population-Based Study
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea
- 2Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea
- 3Supportive Care Center/Department of Family Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Clinical Research Design & Evaluation, Samsung Advanced Institute for Health Sciences & Technology, Sungkyunkwan University, Seoul, Korea
- 5Division of Nephrology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 6Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2529220
- DOI: http://doi.org/10.3803/EnM.2021.1333
Abstract
- Background
Hyperthyroidism is associated with an increased glomerular filtration rate (GFR) in the hyperdynamic state, which is reversible after restoring euthyroidism. However, long-term follow-up of renal dysfunction in patients with hyperthyroidism has not been performed.
Methods
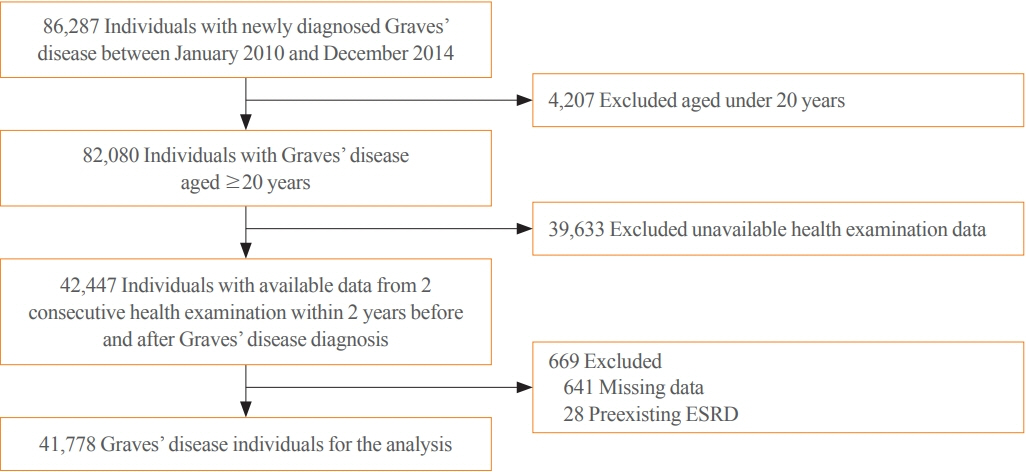
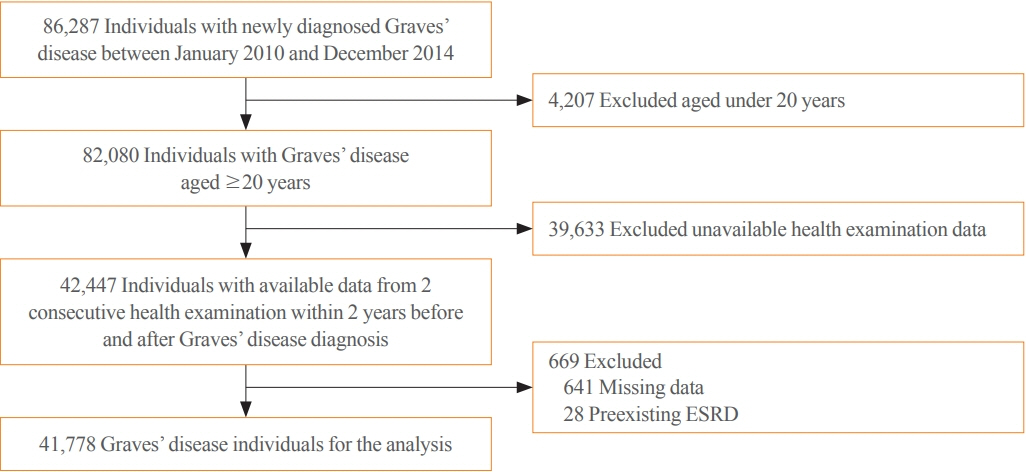
This was a retrospective cohort study using the Korean National Health Insurance database and biannual health checkup data. We included 41,778 Graves’ disease (GD) patients and 41,778 healthy controls, matched by age and sex. The incidences of end-stage renal disease (ESRD) were calculated in GD patients and controls. The cumulative dose and duration of antithyroid drugs (ATDs) were calculated for each patient and categorized into the highest, middle, and lowest tertiles.
Results
Among 41,778 GD patients, 55 ESRD cases occurred during 268,552 person-years of follow-up. Relative to the controls, regardless of smoking, drinking, or comorbidities, including chronic kidney disease, GD patients had a 47% lower risk of developing ESRD (hazard ratio [HR], 0.53; 95% confidence interval [CI], 0.37 to 0.76). In particular, GD patients with a higher baseline GFR (≥90 mL/min/1.73 m2; HR, 0.33; 95% CI, 0.11 to 0.99), longer treatment duration (>33 months; HR, 0.31; 95% CI, 0.17 to 0.58) or higher cumulative dose (>16,463 mg; HR, 0.29; 95% CI, 0.15 to 0.57) of ATDs had a significantly reduced risk of ESRD.
Conclusion
This was the first epidemiological study on the effect of GD on ESRD, and we demonstrated that GD population had a reduced risk for developing ESRD.
Figure
Cited by 1 articles
-
Effect of Hyperthyroidism on Preventing Renal Insufficiency
Tae Yong Kim
Endocrinol Metab. 2022;37(2):220-220. doi: 10.3803/EnM.2022.201.
Reference
-
1. Kaptein EM, Quion-Verde H, Massry SG. Hemodynamic effects of thyroid hormone. Contrib Nephrol. 1984; 41:151–9.
Article2. Kaptein EM, Feinstein EI, Massry SG. Thyroid hormone metabolism in renal diseases. Contrib Nephrol. 1982; 33:122–35.3. Katz AI, Emmanouel DS, Lindheimer MD. Thyroid hormone and the kidney. Nephron. 1975; 15(3-5):223–49.
Article4. Mariani LH, Berns JS. The renal manifestations of thyroid disease. J Am Soc Nephrol. 2012; 23:22–6.
Article5. Montenegro J, Gonzalez O, Saracho R, Aguirre R, Gonzalez O, Martinez I. Changes in renal function in primary hypothyroidism. Am J Kidney Dis. 1996; 27:195–8.
Article6. Cho YY, Kim SK, Jung JH, Hahm JR, Kim TH, Chung JH, et al. Long-term outcomes of renal function after radioactive iodine therapy for thyroid cancer according to preparation method: thyroid hormone withdrawal vs. recombinant human thyrotropin. Endocrine. 2019; 64:293–8.
Article7. Karanikas G, Schutz M, Szabo M, Becherer A, Wiesner K, Dudczak R, et al. Isotopic renal function studies in severe hypothyroidism and after thyroid hormone replacement therapy. Am J Nephrol. 2004; 24:41–5.
Article8. den Hollander JG, Wulkan RW, Mantel MJ, Berghout A. Correlation between severity of thyroid dysfunction and renal function. Clin Endocrinol (Oxf). 2005; 62:423–7.
Article9. Sonmez E, Bulur O, Ertugrul DT, Sahin K, Beyan E, Dal K. Hyperthyroidism influences renal function. Endocrine. 2019; 65:144–8.
Article10. Kimmel M, Braun N, Alscher MD. Influence of thyroid function on different kidney function tests. Kidney Blood Press Res. 2012; 35:9–17.
Article11. Kwon H, Jung JH, Han KD, Park YG, Cho JH, Lee DY, et al. Prevalence and annual incidence of thyroid disease in Korea from 2006 to 2015: a nationwide population-based cohort study. Endocrinol Metab (Seoul). 2018; 33:260–7.
Article12. Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002; 87:489–99.13. Shin DW, Cho B, Guallar E. Korean National Health Insurance Database. JAMA Intern Med. 2016; 176:138.
Article14. Seo GH, Kim SW, Chung JH. Incidence & prevalence of hyperthyroidism and preference for therapeutic modalities in Korea. J Korean Thyroid Assoc. 2013; 6:56–63.
Article15. Kim MK, Han K, Koh ES, Kim HS, Kwon HS, Park YM, et al. Variability in total cholesterol is associated with the risk of end-stage renal disease: a nationwide population-based study. Arterioscler Thromb Vasc Biol. 2017; 37:1963–70.16. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999; 130:461–70.
Article17. Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016; 26:1343–421.
Article18. Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017; 27:315–89.
Article19. Li X, Misik AJ, Rieder CV, Solaro RJ, Lowen A, Fliegel L. Thyroid hormone receptor alpha 1 regulates expression of the Na+/H+ exchanger (NHE1). J Biol Chem. 2002; 277:28656–62.20. Santos Ornellas D, Grozovsky R, Goldenberg RC, Carvalho DP, Fong P, Guggino WB, et al. Thyroid hormone modulates ClC-2 chloride channel gene expression in rat renal proximal tubules. J Endocrinol. 2003; 178:503–11.
Article21. Razvi S, Jabbar A, Pingitore A, Danzi S, Biondi B, Klein I, et al. Thyroid hormones and cardiovascular function and diseases. J Am Coll Cardiol. 2018; 71:1781–96.
Article22. Vargas F, Moreno JM, Rodriguez-Gomez I, Wangensteen R, Osuna A, Alvarez-Guerra M, et al. Vascular and renal function in experimental thyroid disorders. Eur J Endocrinol. 2006; 154:197–212.
Article23. Iseki K, Ikemiya Y, Fukiyama K. Risk factors of end-stage renal disease and serum creatinine in a community-based mass screening. Kidney Int. 1997; 51:850–4.
Article24. Huang B, Zhang Y, Wang L, Wu Q, Li T, Zhang J, et al. Phospholipase A2 receptor autoantibodies as a novel serological biomarker for autoimmune thyroid disease associated nephropathy. Front Immunol. 2020; 11:837.
Article25. Moon JH, Yi KH. The diagnosis and management of hyperthyroidism in Korea: consensus report of the Korean Thyroid Association. Endocrinol Metab (Seoul). 2013; 28:275–9.
Article26. Nystrom HF, Jansson S, Berg G. Incidence rate and clinical features of hyperthyroidism in a long-term iodine sufficient area of Sweden (Gothenburg) 2003-2005. Clin Endocrinol (Oxf). 2013; 78:768–76.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Therapeutic Consideration for the Elderly Patients with End Stage Renal Disease
- Risk factors for peptic ulcer disease in patients with end-stage renal disease receiving dialysis
- Anemia and nutrition in end stage renal disease patient
- Cardiovascular disease in end-stage renal disease
- The Coexistence of Fibromuscular Dysplasia of the Renal Artery and Graves’ Disease in an Adolescent: A Case Report