J Rhinol.
2022 Mar;29(1):52-55. 10.18787/jr.2021.00381.
A Case of Oculomotor Nerve Paralysis Caused by Cavernous Sinus Metastasis of Tonsil Cancer
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, School of Medicine, Sungkyunkwan University, Seoul, Republic of Korea
- KMID: 2528321
- DOI: http://doi.org/10.18787/jr.2021.00381
Abstract
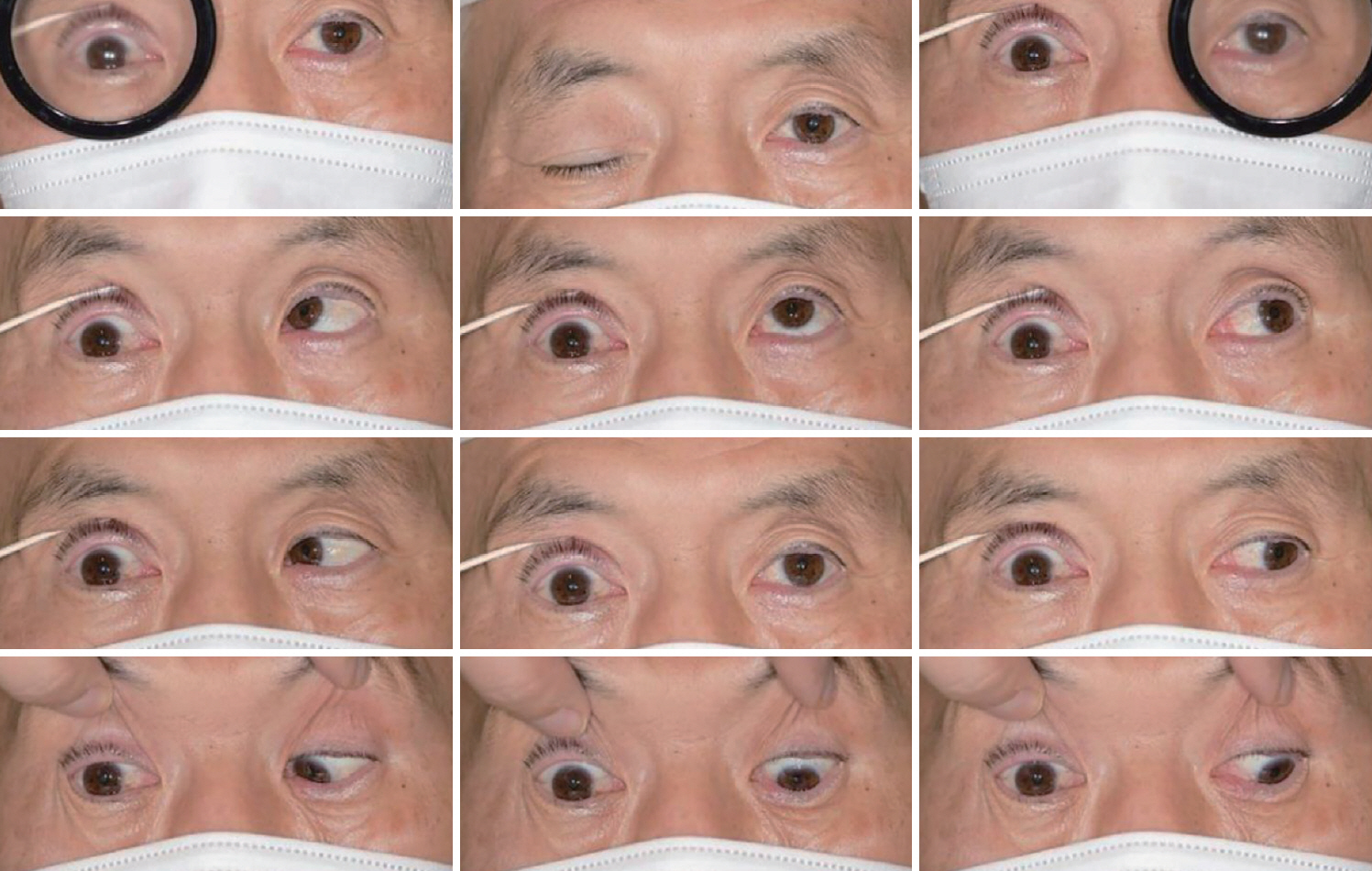
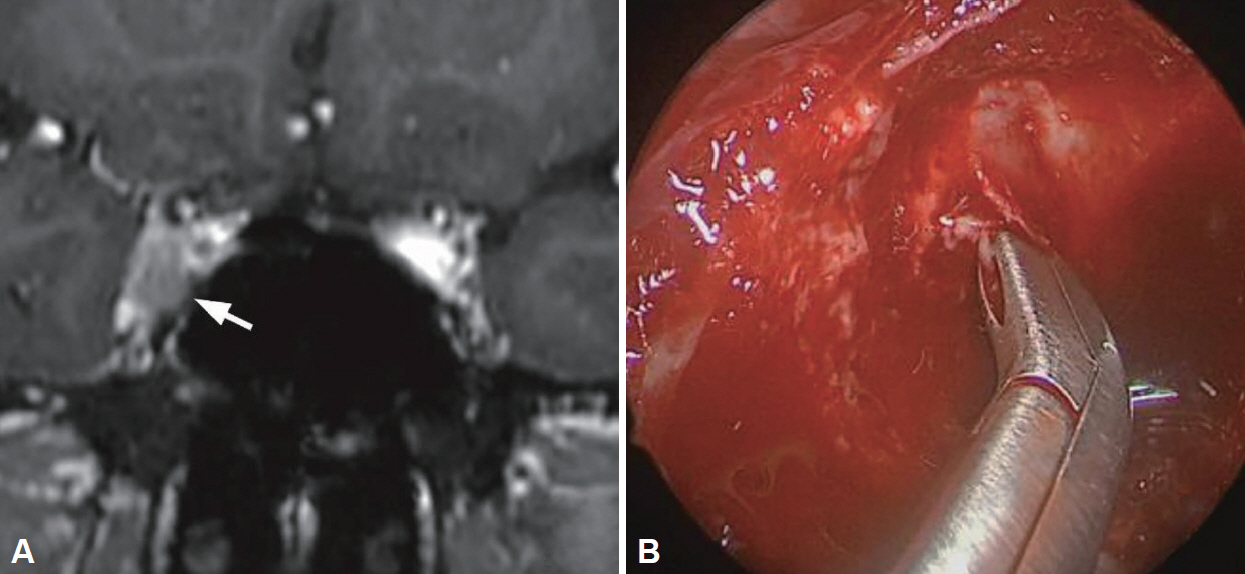
- Oropharyngeal squamous cell carcinoma (OSCC) with metastasis to the cavernous sinus (CS) is uncommon, and only a few cases have been described in the literature. The highest age-adjusted incidence rate for OSCC including the tonsil in males occurs in South Asians, and more cases should be reported to establish earlier identification and treatment. We report a case of OSCC in a 59-year-old male who underwent prompt endoscopic biopsy and early palliative radiation therapy to allow complete recovery of cranial nerve palsies to improve his quality of life, despite having a poor prognosis. Furthermore, this report emphasizes his dramatic resolution of symptoms after radiation therapy, highlighting the importance of rapid recognition and proper management.
Keyword
Figure
Reference
-
1. Johnson-Obaseki S, McDonald JT, Corsten M, Rourke R. Head and neck cancer in Canada: trends 1992 to 2007. Otolaryngol Head Neck Surg. 2012; 147(1):74–8.2. Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010; 363(1):24–35.
Article3. Glastonbury CM. Head and neck squamous cell cancer: approach to staging and surveillance. In : Hodler J, Kubik-Huch RA, von Schulthess GK, editors. Diseases of the brain, head and neck, spine 2020-2023: diagnostic Imaging. 1st ed. Cham (CH): Springer International Publishing;2020. p. 215–22.4. Huang SH, Perez-Ordonez B, Liu FF, Waldron J, Ringash J, Irish J, et al. Atypical clinical behavior of p16-confirmed HPV-related oropharyngeal squamous cell carcinoma treated with radical radiotherapy. Int J Radiat Oncol Biol Phys. 2012; 82(1):276–83.
Article5. Marchese-Ragona R, Maria Ferraro S, Marioni G, Staffieri C, Manara R, Restivo DA, et al. Abducent nerve paralysis: first clinical sign of clivus metastasis from tonsillar carcinoma. Acta Otolaryngol. 2008; 128(6):713–6.
Article6. González García R, Sastre Pérez J, Naval Gías L, Rodríguez Campo FJ, Díaz González FJ. Cavernous sinus metastasis from oropharyngeal squamous cell carcinoma. Med Oral Patol Oral Cir Bucal. 2007; 12(2):E166–70.7. Forner D, Wilke D, Rigby MH, Croul S, Mishra A, Massoud E, et al. Cavernous sinus involvement in human papillomavirus associated oropharyngeal squamous cell carcinoma: case report of an atypical site of distant metastasis. J Otolaryngol Head Neck Surg. 2018; 47(1):32.
Article8. Dellaretti M, Almeida JC, Martins WCDS, Faria MP. Percutaneous biopsy of lesions in the cavernous sinus: a systematic review. World Neurosurg. 2017; 108:1–5.
Article9. Bly RA, Ramakrishna R, Ferreira M, Moe KS. Lateral transorbital neuroendoscopic approach to the lateral cavernous sinus. J Neurol Surg B Skull Base. 2014; 75(1):11–7.10. Liu HS, Di X. Endoscopic endonasal surgery for biopsy of cavernous sinus lesions. Minim Invasive Neurosurg. 2009; 52(2):69–73.
Article11. Rosenfeld DJ, Berenholz L, Glasgold M, Rao V, Spiegel J. Malignant neoplasms of the sphenoid sinus. Trans Pa Acad Ophthalmol Otolaryngol. 1987; 39(1):618–21.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolated Oculomotor Nerve Palsy Caused by Cavernous Sinus Dural Arteriovenous Fistula: Case Report
- Oculomotor and Abducens Nerve Palsy Complicated by Cavernous Sinus Thrombophlebitis Resulting from Acute Sinusitis
- Cavernous Angioma of the Oculomotor Nerve
- Isolated Oculomotor Nerve Palsy due to Non-Hodgkin's Lymphoma Demonstrated by Serial MRI
- Isolated Sphenoid Sinus Mucocele Presenting as Third Nerve Palsy