Acute Crit Care.
2022 Feb;37(1):35-44. 10.4266/acc.2021.01193.
Brain-lung interaction: a vicious cycle in traumatic brain injury
- Affiliations
-
- 1Colombian Clinical Research Group in Neurocritical Care, University of Pamplona, Cúcuta, Colombia
- 2Colombian Clinical Research Group in Neurocritical Care, University of Cartagena, Cartagena, Colombia
- 3Latin American Council of Neurocritical Care (CLaNi), Cartagena, Colombia
- 4Global Neurosurgery Committee, World Federation of Neurosurgical Societies, Cartagena, Colombia
- 5Medical and Surgical Research Center, Cartagena, Colombia
- 6Department of Intensive Care, Hospital Maciel, Montevideo, Uruguay
- 7Department of Intensive Care, Regions Hospital, St. Paul, MN, USA
- KMID: 2527905
- DOI: http://doi.org/10.4266/acc.2021.01193
Abstract
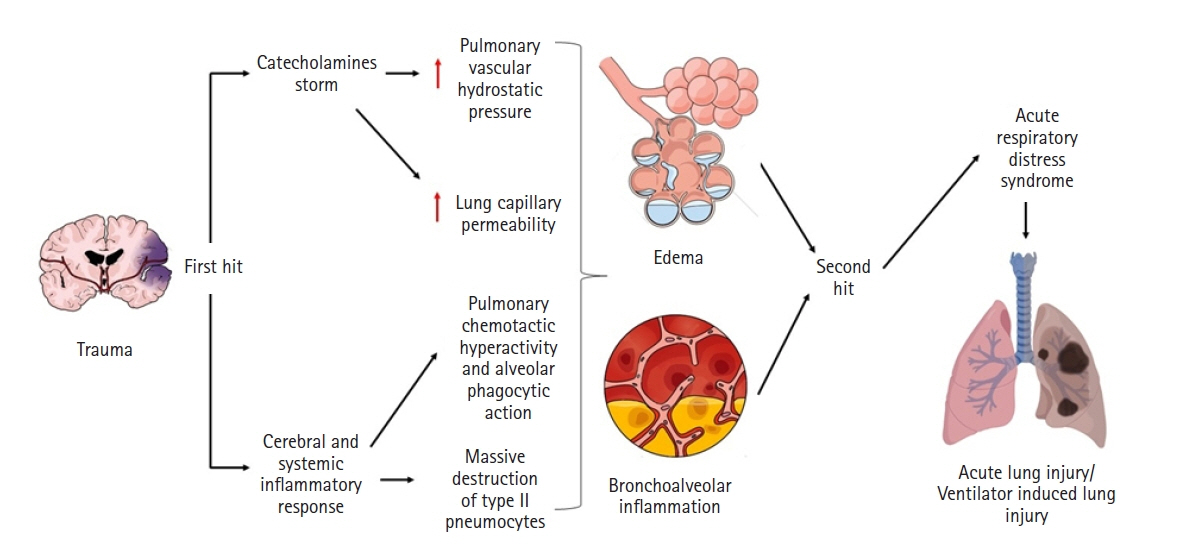
- The brain-lung interaction can seriously affect patients with traumatic brain injury, triggering a vicious cycle that worsens patient prognosis. Although the mechanisms of the interaction are not fully elucidated, several hypotheses, notably the “blast injury” theory or “double hit” model, have been proposed and constitute the basis of its development and progression. The brain and lungs strongly interact via complex pathways from the brain to the lungs but also from the lungs to the brain. The main pulmonary disorders that occur after brain injuries are neurogenic pulmonary edema, acute respiratory distress syndrome, and ventilator-associated pneumonia, and the principal brain disorders after lung injuries include brain hypoxia and intracranial hypertension. All of these conditions are key considerations for management therapies after traumatic brain injury and need exceptional case-by-case monitoring to avoid neurological or pulmonary complications. This review aims to describe the history, pathophysiology, risk factors, characteristics, and complications of brain-lung and lung-brain interactions and the impact of different old and recent modalities of treatment in the context of traumatic brain injury.
Keyword
Figure
Cited by 1 articles
-
The role of cardiac dysfunction and post-traumatic pulmonary embolism in brain-lung interactions following traumatic brain injury
Mabrouk Bahloul, Karama Bouchaala, Najeh Baccouche, Kamilia Chtara, Hedi Chelly, Mounir Bouaziz
Acute Crit Care. 2022;37(2):266-268. doi: 10.4266/acc.2022.00374.
Reference
-
1. Johnson WD, Griswold DP. Traumatic brain injury: a global challenge. Lancet Neurol. 2017; 16:949–50.
Article2. Okidi R, Ogwang DM, Okello TR, Ezati D, Kyegombe W, Nyeko D, et al. Factors affecting mortality after traumatic brain injury in a resource-poor setting. BJS Open. 2020; 4:320–5.
Article3. Lee K, Rincon F. Pulmonary complications in patients with severe brain injury. Crit Care Res Pract. 2012; 2012:207247.
Article4. Mrozek S, Constantin JM, Geeraerts T. Brain-lung crosstalk: implications for neurocritical care patients. World J Crit Care Med. 2015; 4:163–78.
Article5. Brown-Séquard CE. On the production of hemorrhage, anemia, edema and emphysema in the lungs by injuries to the base of the brain. Lancet. 1871; 97:6.
Article6. Simmons RL, Martin AM Jr, Heisterkamp CA 3rd, Ducker TB. Respiratory insufficiency in combat casualties. II. Pulmonary edema following head injury. Ann Surg. 1969; 170:39–44.7. Theodore J, Robin ED. Speculations on neurogenic pulmonary edema (NPE). Am Rev Respir Dis. 1976; 113:405–11.8. Brambrink AM, Dick WF. Neurogenic pulmonary edema: pathogenesis, clinical picture and therapy. Anaesthesist. 1997; 46:953–63.9. López-Aguilar J, Fernández-Gonzalo MS, Turon M, Quílez ME, Gómez-Simón V, Jódar MM, et al. Lung-brain interaction in the mechanically ventilated patient. Med Intensiva. 2013; 37:485–92.
Article10. Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet. 1967; 2:319–23.
Article11. Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis. 1988; 138:720–3.
Article12. Bratton SL, Davis RL. Acute lung injury in isolated traumatic brain injury. Neurosurgery. 1997; 40:707–12.
Article13. Holland MC, Mackersie RC, Morabito D, Campbell AR, Kivett VA, Patel R, et al. The development of acute lung injury is associated with worse neurologic outcome in patients with severe traumatic brain injury. J Trauma. 2003; 55:106–11.
Article14. Contant CF, Valadka AB, Gopinath SP, Hannay HJ, Robertson CS. Adult respiratory distress syndrome: a complication of induced hypertension after severe head injury. J Neurosurg. 2001; 95:560–8.
Article15. Rincon F, Ghosh S, Dey S, Maltenfort M, Vibbert M, Urtecho J, et al. Impact of acute lung injury and acute respiratory distress syndrome after traumatic brain injury in the United States. Neurosurgery. 2012; 71:795–803.
Article16. Dziedzic T, Slowik A, Szczudlik A. Nosocomial infections and immunity: lesson from brain-injured patients. Crit Care. 2004; 8:266–70.17. Piek J, Chesnut RM, Marshall LF, van Berkum-Clark M, Klauber MR, Blunt BA, et al. Extracranial complications of severe head injury. J Neurosurg. 1992; 77:901–7.
Article18. Woratyla SP, Morgan AS, Mackay L, Bernstein B, Barba C. Factors associated with early onset pneumonia in the severely brain-injured patient. Conn Med. 1995; 59:643–7.19. Fàbregas N, Torres A. Pulmonary infection in the brain injured patient. Minerva Anestesiol. 2002; 68:285–90.20. Ranieri VM, Suter PM, Tortorella C, De Tullio R, Dayer JM, Brienza A, et al. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA. 1999; 282:54–61.
Article21. Bronchard R, Albaladejo P, Brezac G, Geffroy A, Seince PF, Morris W, et al. Early onset pneumonia: risk factors and consequences in head trauma patients. Anesthesiology. 2004; 100:234–9.22. Koutsoukou A, Katsiari M, Orfanos SE, Kotanidou A, Daganou M, Kyriakopoulou M, et al. Respiratory mechanics in brain injury: a review. World J Crit Care Med. 2016; 5:65–73.
Article23. Gonzalvo R, Martí-Sistac O, Blanch L, López-Aguilar J. Bench-to-bedside review: brain-lung interaction in the critically ill. A pending issue revisited. Crit Care. 2007; 11:216.
Article24. Mascia L. Acute lung injury in patients with severe brain injury: a double hit model. Neurocrit Care. 2009; 11:417–26.
Article25. Al-Dhahir MA, Das JM, Sharma S. Neurogenic pulmonary edema [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 [cited 2021 Sep 31]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532984/.26. Kennedy JD, Hardin KA, Parikh P, Li CS, Seyal M. Pulmonary edema following generalized tonic clonic seizures is directly associated with seizure duration. Seizure. 2015; 27:19–24.
Article27. Raja HM, Herwadkar AV, Paroutoglou K, Lilleker JB. Neurogenic pulmonary oedema complicating a lateral medullary infarct. BMJ Case Rep. 2018; 2018:bcr2018225437.
Article28. Romero Osorio OM, Abaunza Camacho JF, Sandoval Briceño D, Lasalvia P, Narino Gonzalez D. Postictal neurogenic pulmonary edema: case report and brief literature review. Epilepsy Behav Case Rep. 2017; 9:49–50.
Article29. Šedý J, Kuneš J, Zicha J. Pathogenetic mechanisms of neurogenic pulmonary edema. J Neurotrauma. 2015; 32:1135–45.
Article30. Busl KM, Bleck TP. Neurogenic pulmonary edema. Crit Care Med. 2015; 43:1710–5.
Article31. Zhang L, Yao J, Zhang T, Jin J, Zeng X, Yue Z. Stellate ganglion block may prevent the development of neurogenic pulmonary edema and improve the outcome. Med Hypotheses. 2013; 80:158–61.
Article32. Rincon F, Maltenfort M, Dey S, Ghosh S, Vibbert M, Urtecho J, et al. The prevalence and impact of mortality of the acute respiratory distress syndrome on admissions of patients with ischemic stroke in the United States. J Intensive Care Med. 2014; 29:357–64.
Article33. Papazian L, Klompas M, Luyt CE. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. 2020; 46:888–906.
Article34. Othman AA, Abdelazim MS. Ventilator-associated pneumonia in adult intensive care unit prevalence and complications. Egypt J Crit Care Med. 2017; 5:61–3.
Article35. Ding C, Zhang Y, Yang Z, Wang J, Jin A, Wang W, et al. Incidence, temporal trend and factors associated with ventilator-associated pneumonia in mainland China: a systematic review and meta-analysis. BMC Infect Dis. 2017; 17:468.
Article36. Jovanovic B, Milan Z, Markovic-Denic L, Djuric O, Radinovic K, Doklestic K, et al. Risk factors for ventilator-associated pneumonia in patients with severe traumatic brain injury in a Serbian trauma centre. Int J Infect Dis. 2015; 38:46–51.
Article37. Di Pasquale M, Ferrer M, Esperatti M, Crisafulli E, Giunta V, Li Bassi G, et al. Assessment of severity of ICU-acquired pneumonia and association with etiology. Crit Care Med. 2014; 42:303–12.
Article38. Huang Y, Jiao Y, Zhang J, Xu J, Cheng Q, Li Y, et al. Microbial etiology and prognostic factors of ventilator-associated pneumonia: a multicenter retrospective study in Shanghai. Clin Infect Dis. 2018; 67(Suppl 2):S146–52.
Article39. Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016; 63:e61–111.40. Martin-Loeches I, Deja M, Koulenti D, Dimopoulos G, Marsh B, Torres A, et al. Potentially resistant microorganisms in intubated patients with hospital-acquired pneumonia: the interaction of ecology, shock and risk factors. Intensive Care Med. 2013; 39:672–81.
Article41. Bickenbach J, Zoremba N, Fries M, Dembinski R, Doering R, Ogawa E, et al. Low tidal volume ventilation in a porcine model of acute lung injury improves cerebral tissue oxygenation. Anesth Analg. 2009; 109:847–55.
Article42. Mikkelsen ME, Christie JD, Lanken PN, Biester RC, Thompson BT, Bellamy SL, et al. The adult respiratory distress syndrome cognitive outcomes study: long-term neuropsychological function in survivors of acute lung injury. Am J Respir Crit Care Med. 2012; 185:1307–15.
Article43. Fries M, Bickenbach J, Henzler D, Beckers S, Dembinski R, Sellhaus B, et al. S-100 protein and neurohistopathologic changes in a porcine model of acute lung injury. Anesthesiology. 2005; 102:761–7.
Article44. Bickenbach J, Biener I, Czaplik M, Nolte K, Dembinski R, Marx G, et al. Neurological outcome after experimental lung injury. Respir Physiol Neurobiol. 2011; 179:174–80.
Article45. Bassi TG, Rohrs EC, Reynolds SC. Systematic review of cognitive impairment and brain insult after mechanical ventilation. Crit Care. 2021; 25:99.
Article46. Hopkins RO, Gale SD, Weaver LK. Brain atrophy and cognitive impairment in survivors of acute respiratory distress syndrome. Brain Inj. 2006; 20:263–71.
Article47. Kamuf J, Garcia-Bardon A, Ziebart A, Thomas R, Folkert K, Frauenknecht K, et al. Lung injury does not aggravate mechanical ventilation-induced early cerebral inflammation or apoptosis in an animal model. PLoS One. 2018; 13:e0202131.
Article48. Al-Attar R, Childers CL, Nguyen VC, Pamenter ME, Storey KB. Differential protein phosphorylation is responsible for hypoxia-induced regulation of the Akt/mTOR pathway in naked mole rats. Comp Biochem Physiol A Mol Integr Physiol. 2020; 242:110653.
Article49. Caricato A, Conti G, Della Corte F, Mancino A, Santilli F, Sandroni C, et al. Effects of PEEP on the intracranial system of patients with head injury and subarachnoid hemorrhage: the role of respiratory system compliance. J Trauma. 2005; 58:571–6.
Article50. Heuer JF, Pelosi P, Hermann P, Perske C, Crozier TA, Brück W, et al. Acute effects of intracranial hypertension and ARDS on pulmonary and neuronal damage: a randomized experimental study in pigs. Intensive Care Med. 2011; 37:1182–91.
Article51. Robba C, Poole D, McNett M, Asehnoune K, Bösel J, Bruder N, et al. Mechanical ventilation in patients with acute brain injury: recommendations of the European Society of Intensive Care Medicine consensus. Intensive Care Med. 2020; 46:2397–410.
Article52. Della Torre V, Badenes R, Corradi F, Racca F, Lavinio A, Matta B, et al. Acute respiratory distress syndrome in traumatic brain injury: how do we manage it? J Thorac Dis. 2017; 9:5368–81.
Article53. Mascia L, Zavala E, Bosma K, Pasero D, Decaroli D, Andrews P, et al. High tidal volume is associated with the development of acute lung injury after severe brain injury: an international observational study. Crit Care Med. 2007; 35:1815–20.
Article54. Krebs J, Tsagogiorgas C, Pelosi P, Rocco PR, Hottenrott M, Sticht C, et al. Open lung approach with low tidal volume mechanical ventilation attenuates lung injury in rats with massive brain damage. Crit Care. 2014; 18:R59.
Article55. Borsellino B, Schultz MJ, Gama de Abreu M, Robba C, Bilotta F. Mechanical ventilation in neurocritical care patients: a systematic literature review. Expert Rev Respir Med. 2016; 10:1123–32.
Article56. Carney N, Totten AM, O'Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017; 80:6–15.
Article57. Asehnoune K, Roquilly A, Cinotti R. Respiratory management in patients with severe brain injury. Crit Care. 2018; 22:76.
Article58. Chapin JC, Downs JB, Douglas ME, Murphy EJ, Ruiz BC. Lung expansion, airway pressure transmission, and positive end-expiratory pressure. Arch Surg. 1979; 114:1193–7.
Article59. Nemer SN, Caldeira JB, Santos RG, Guimarães BL, Garcia JM, Prado D, et al. Effects of positive end-expiratory pressure on brain tissue oxygen pressure of severe traumatic brain injury patients with acute respiratory distress syndrome: A pilot study. J Crit Care. 2015; 30:1263–6.
Article60. Chen H, Chen K, Xu JQ, Zhang YR, Yu RG, Zhou JX. Intracranial pressure responsiveness to positive end-expiratory pressure is influenced by chest wall elastance: a physiological study in patients with aneurysmal subarachnoid hemorrhage. BMC Neurol. 2018; 18:124.
Article61. Ashton-Cleary DT, Duffy MR. Prone ventilation for refractory hypoxaemia in a patient with severe chest wall disruption and traumatic brain injury. Br J Anaesth. 2011; 107:1009–10.
Article62. Robba C, Rebora P, Banzato E, Wiegers E, Stocchetti N, Menon DK, et al. Incidence, risk factors, and effects on outcome of ventilator-associated pneumonia in patients with traumatic brain injury: analysis of a large, multicenter, prospective, observational longitudinal study. Chest. 2020; 158:2292–303.63. Kerr N, de Rivero Vaccari JP, Dietrich WD, Keane RW. Neural-respiratory inflammasome axis in traumatic brain injury. Exp Neurol. 2020; 323:113080.
Article64. Bortolotti P, Faure E, Kipnis E. Inflammasomes in tissue damages and immune disorders after trauma. Front Immunol. 2018; 9:1900.
Article65. Lee SW, de Rivero Vaccari JP, Truettner JS, Dietrich WD, Keane RW. The role of microglial inflammasome activation in pyroptotic cell death following penetrating traumatic brain injury. J Neuroinflammation. 2019; 16:27.
Article66. Kerr NA, de Rivero Vaccari JP, Weaver C, Dietrich WD, Ahmed T, Keane RW. Enoxaparin attenuates acute lung injury and inflammasome activation after traumatic brain injury. J Neurotrauma. 2021; 38:646–54.
Article