Ann Surg Treat Res.
2022 Apr;102(4):185-192. 10.4174/astr.2022.102.4.185.
Incidental gallbladder cancer: a retrospective clinical study of 40 cases
- Affiliations
-
- 1Department of Surgical Oncology, Balcalı Training and Research Hospital, Cukurova University, Adana, Turkey
- 2Department of Pathology, Cengiz Gokcek Gynecology, Obstetrics, and Pediatrics Hospital, Gaziantep, Turkey
- 3Department of General Surgery, Seyhan Government Hospital, Adana, Turkey
- 4Department of Surgical Oncology, Hatay Training and Research Hospital, Hatay, Turkey
- KMID: 2527835
- DOI: http://doi.org/10.4174/astr.2022.102.4.185
Abstract
- Purpose
Cholecystectomy is one of the most common surgeries today due to gallbladder diseases. The most prevalent malignancy of the biliary tract is gallbladder cancer. We aimed to discuss the results of our patients who underwent cholecystectomy for benign reasons in our clinic and who had gallbladder cancer due to pathology.
Methods
The results of cholecystectomy performed in General Surgery Clinic of Seyhan Government Hospital were evaluated. Cases diagnosed as gallbladder as a result of histopathological examination were included. Preoperative ultrasonography, laboratory findings, and postoperative pathology results of the patients were reviewed retrospectively. The pathologist repeated histopathological evaluations.
Results
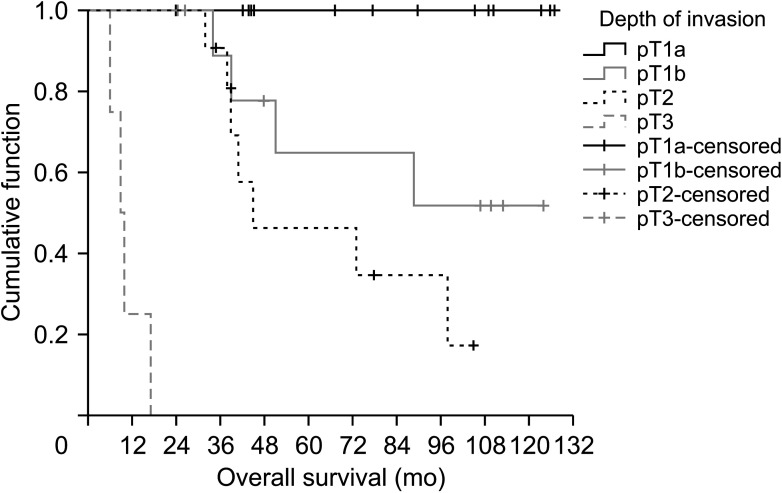
Between 2010 and 2019, incidental gallbladder cancer (IGBC) was detected in 40 patients (0.3%) in 11,680 cholecystectomy operations. Of the patients diagnosed with IGBC, 14 (35.0%) were T1a, 11 (27.5%) were T1b, 11 (27.5%) were T2, and 4 (10.0%) were T3. T4 tumor was not seen in any patient. Three patients who were T1b at initial evaluation were identified as T2 at evaluation for the study. The pathology results of 37 patients (92.5%) were adenocarcinoma, 2 (5.0%) were adenosquamous type, and 1 (0.5%) was squamous cell carcinoma.
Conclusion
There has been a remarkable increase in the number of IGBCs over the past 20 years. Appropriate staging and histopathological evaluation are essential in guiding the surgeon’s operation. It is crucial to accurately determine the T stage, the most influential parameter on patient survival and residual recurrences. The distinction between pathologic (p) T1a and pT1b should be made carefully. Surgery is the only potentially curative method.
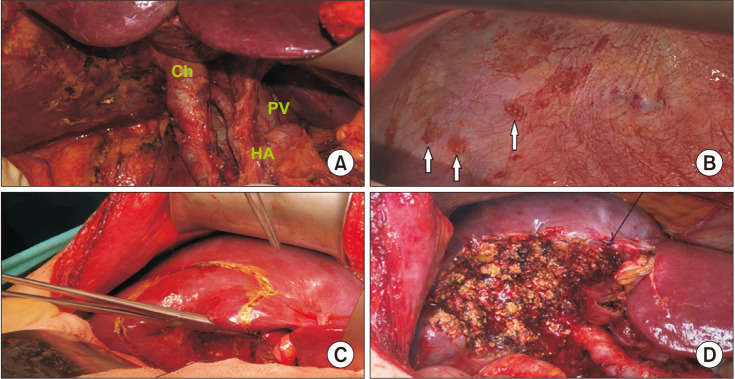
Figure
Reference
-
1. Fuks D, Regimbeau JM, Le Treut YP, Bachellier P, Raventos A, Pruvot FR, et al. Incidental gallbladder cancer by the AFC-GBC-2009 Study Group. World J Surg. 2011; 35:1887–1897. PMID: 21547420.
Article2. Pitt SC, Jin LX, Hall BL, Strasberg SM, Pitt HA. Incidental gallbladder cancer at cholecystectomy: when should the surgeon be suspicious? Ann Surg. 2014; 260:128–133. PMID: 24509205.3. Ahn Y, Park CS, Hwang S, Jang HJ, Choi KM, Lee SG. Incidental gallbladder cancer after routine cholecystectomy: when should we suspect it preoperatively and what are predictors of patient survival? Ann Surg Treat Res. 2016; 90:131–138. PMID: 26942156.
Article4. Nagarajan G, Kundalia K. Should every cholecystectomy specimen be sent for histopathology to identify incidental gall bladder cancer? Indian J Cancer. 2020; 57:2–3. PMID: 32129293.
Article5. Zaidi MY, Abou-Alfa GK, Ethun CG, Shrikhande SV, Goel M, Nervi B, et al. Evaluation and management of incidental gallbladder cancer. Chin Clin Oncol. 2019; 8:37. PMID: 31431030.
Article6. Chan KM, Yu MC, Lee WC, Jan YY, Chen MF. Adenosquamous/squamous cell carcinoma of the gallbladder. J Surg Oncol. 2007; 95:129–134. PMID: 17262729.
Article7. Agarwal AK, Kalayarasan R, Singh S, Javed A, Sakhuja P. All cholecystectomy specimens must be sent for histopathology to detect inapparent gallbladder cancer. HPB (Oxford). 2012; 14:269–273. PMID: 22404266.
Article8. Fahim RB, McDonald JR, Richards JC, Ferris DO. Carcinoma of the gallbladder: a study of its modes of spread. Ann Surg. 1962; 156:114–124. PMID: 13891308.9. Pawlik TM, Gleisner AL, Vigano L, Kooby DA, Bauer TW, Frilling A, et al. Incidence of finding residual disease for incidental gallbladder carcinoma: implications for re-resection. J Gastrointest Surg. 2007; 11:1478–1487. PMID: 17846848.
Article10. Butte JM, Kingham TP, Gönen M, D’Angelica MI, Allen PJ, Fong Y, et al. Residual disease predicts outcomes after definitive resection for incidental gallbladder cancer. J Am Coll Surg. 2014; 219:416–429. PMID: 25087941.
Article11. Fong Y, Malhotra S. Gallbladder cancer: recent advances and current guidelines for surgical therapy. Adv Surg. 2001; 35:1–20. PMID: 11579805.12. Lundgren L, Muszynska C, Ros A, Persson G, Gimm O, Valter L, et al. Are incidental gallbladder cancers missed with a selective approach of gallbladder histology at cholecystectomy? World J Surg. 2018; 42:1092–1099. PMID: 28900706.
Article13. Chatelain D, Fuks D, Farges O, Attencourt C, Pruvot FR, Regimbeau JM. Pathology report assessment of incidental gallbladder carcinoma diagnosed from cholecystectomy specimens: results of a French multicentre survey. Dig Liver Dis. 2013; 45:1056–1060. PMID: 23948233.
Article14. Ethun CG, Postlewait LM, Le N, Pawlik TM, Buettner S, Poultsides G, et al. A novel pathology-based preoperative risk score to predict locoregional residual and distant disease and survival for incidental gallbladder cancer: a 10-institution study from the U.S. Extrahepatic Biliary Malignancy Consortium. Ann Surg Oncol. 2017; 24:1343–1350. PMID: 27812827.
Article15. Geramizadeh B, Kashkooe A. Incidental gall bladder adenocarcinoma in cholecystectomy specimens; a single center experience and review of the literature. Middle East J Dig Dis. 2018; 10:249–253. PMID: 31049173.
Article16. Muszynska C, Lundgren L, Lindell G, Andersson R, Nilsson J, Sandström P, et al. Predictors of incidental gallbladder cancer in patients undergoing cholecystectomy for benign gallbladder disease: results from a population-based gallstone surgery registry. Surgery. 2017; 162:256–263. PMID: 28400123.
Article17. Hamdani NH, Qadri SK, Aggarwalla R, Bhartia VK, Chaudhuri S, Debakshi S, et al. Clinicopathological study of gall bladder carcinoma with special reference to gallstones: our 8-year experience from eastern India. Asian Pac J Cancer Prev. 2012; 13:5613–5617. PMID: 23317226.
Article18. Kwon AH, Imamura A, Kitade H, Kamiyama Y. Unsuspected gallbladder cancer diagnosed during or after laparoscopic cholecystectomy. J Surg Oncol. 2008; 97:241–245. PMID: 18095299.
Article19. Søreide K, Guest RV, Harrison EM, Kendall TJ, Garden OJ, Wigmore SJ. Systematic review of management of incidental gallbladder cancer after cholecystectomy. Br J Surg. 2019; 106:32–45. PMID: 30582640.
Article20. Jang JY, Heo JS, Han Y, Chang J, Kim JR, Kim H, et al. Impact of type of surgery on survival outcome in patients with early gallbladder cancer in the era of minimally invasive surgery: oncologic safety of laparoscopic surgery. Medicine (Baltimore). 2016; 95:e3675. PMID: 27258495.21. Aloia TA, Járufe N, Javle M, Maithel SK, Roa JC, Adsay V, et al. Gallbladder cancer: expert consensus statement. HPB (Oxford). 2015; 17:681–690. PMID: 26172135.
Article22. Krell RW, Wei AC. Gallbladder cancer: surgical management. Chin Clin Oncol. 2019; 8:36. PMID: 31431029.
Article23. Benson AB, D’Angelica MI, Abbott DE, Abrams TA, Alberts SR, Anaya DA, et al. Guidelines insights: hepatobiliary cancers, version 2.2019. J Natl Compr Canc Netw. 2019; 17:302–310. PMID: 30959462.
Article24. D’Angelica M, Dalal KM, DeMatteo RP, Fong Y, Blumgart LH, Jarnagin WR. Analysis of the extent of resection for adenocarcinoma of the gallbladder. Ann Surg Oncol. 2009; 16:806–816. PMID: 18985272.
Article25. Araida T, Higuchi R, Hamano M, Kodera Y, Takeshita N, Ota T, et al. Hepatic resection in 485 R0 pT2 and pT3 cases of advanced carcinoma of the gallbladder: results of a Japanese Society of Biliary Surgery survey: a multicenter study. J Hepatobiliary Pancreat Surg. 2009; 16:204–215. PMID: 19219399.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Feature of Incidental Gallbladder Cancer Diagnosed after Laparoscopic Cholecystectomy due to Gallbladder Polyps
- Cholelithiasis as a Risk Factor for Gallbladder Cancer
- When Do We Need Reoperation in Incidental Gallbladder Cancer after Laparoscopic Cholecystectomy?
- The appropriate surgical strategy for T1b gallbladder cancer incidentally diagnosed after a simple cholecystectomy
- Agenesis of the Gallbladder