Diabetes Metab J.
2022 Mar;46(2):198-221. 10.4093/dmj.2021.0347.
Peripheral Neuropathy Phenotyping in Rat Models of Type 2 Diabetes Mellitus: Evaluating Uptake of the Neurodiab Guidelines and Identifying Future Directions
- Affiliations
-
- 1Department of Pharmacology, School of Medical Sciences, University of New South Wales (UNSW) Sydney, Sydney, Australia
- 2Department of Exercise Physiology, School of Medical Sciences, University of New South Wales (UNSW) Sydney, Sydney, Australia
- 3Department of Exercise and Rehabilitation, School of Medical, Indigenous and Health Science, University of Wollongong, Wollongong, Australia
- KMID: 2527715
- DOI: http://doi.org/10.4093/dmj.2021.0347
Abstract
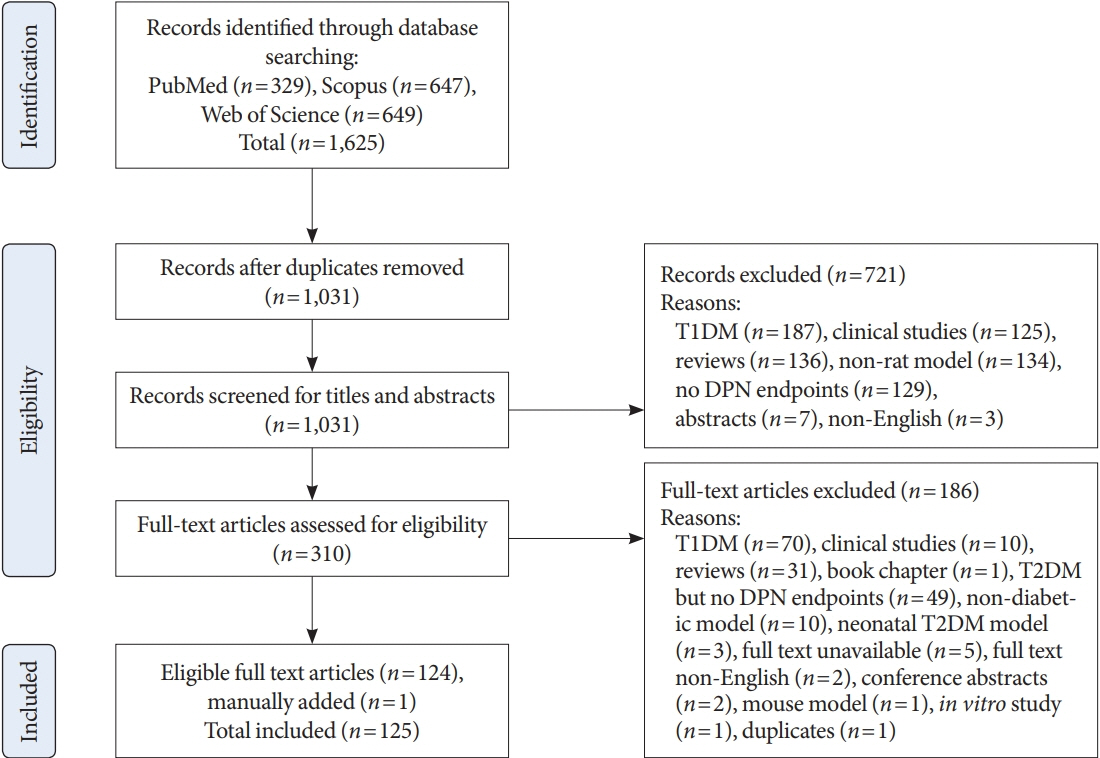
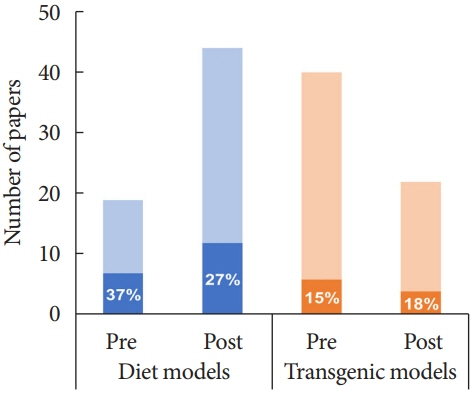
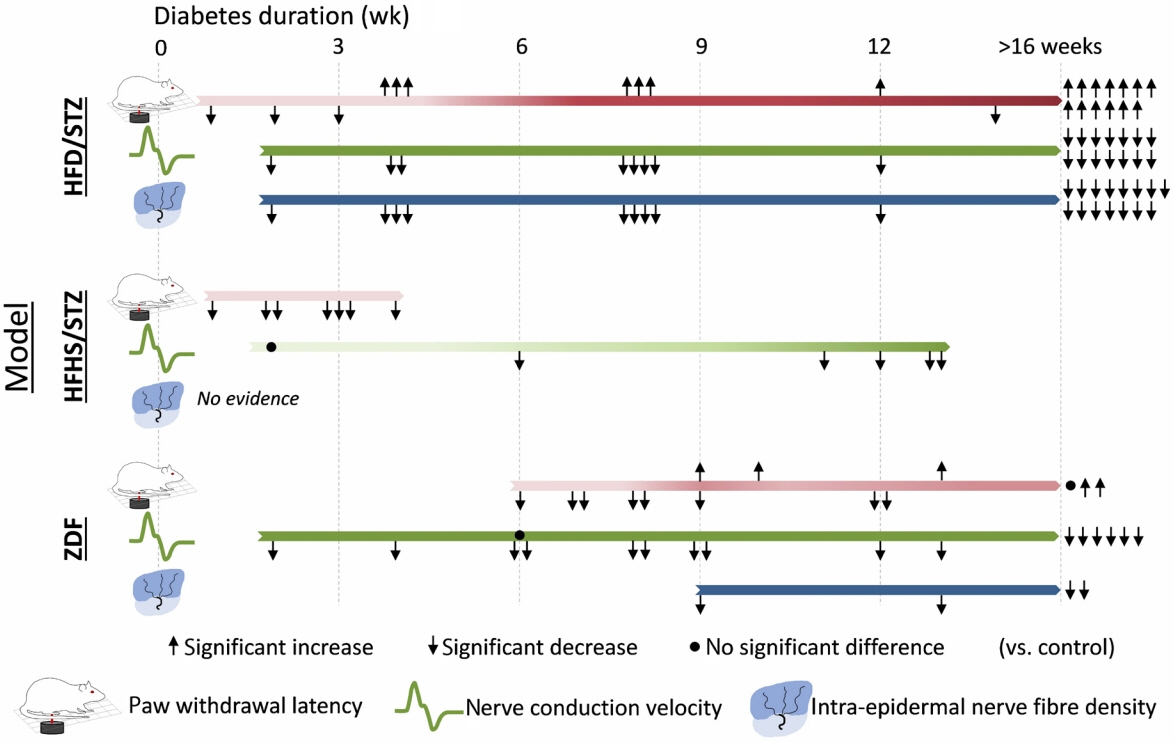
- Diabetic peripheral neuropathy (DPN) affects over half of type 2 diabetes mellitus (T2DM) patients, with an urgent need for effective pharmacotherapies. While many rat and mouse models of T2DM exist, the phenotyping of DPN has been challenging with inconsistencies across laboratories. To better characterize DPN in rodents, a consensus guideline was published in 2014 to accelerate the translation of preclinical findings. Here we review DPN phenotyping in rat models of T2DM against the ‘Neurodiab’ criteria to identify uptake of the guidelines and discuss how DPN phenotypes differ between models and according to diabetes duration and sex. A search of PubMed, Scopus and Web of Science databases identified 125 studies, categorised as either diet and/or chemically induced models or transgenic/spontaneous models of T2DM. The use of diet and chemically induced T2DM models has exceeded that of transgenic models in recent years, and the introduction of the Neurodiab guidelines has not appreciably increased the number of studies assessing all key DPN endpoints. Combined high-fat diet and low dose streptozotocin rat models are the most frequently used and well characterised. Overall, we recommend adherence to Neurodiab guidelines for creating better animal models of DPN to accelerate translation and drug development.
Keyword
Figure
Reference
-
1. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019; 157:107843.
Article2. Feldman EL, Callaghan BC, Pop-Busui R, Zochodne DW, Wright DE, Bennett DL, et al. Diabetic neuropathy. Nat Rev Dis Primers. 2019; 5:41.
Article3. Biessels GJ, Bril V, Calcutt NA, Cameron NE, Cotter MA, Dobrowsky R, et al. Phenotyping animal models of diabetic neuropathy: a consensus statement of the diabetic neuropathy study group of the EASD (Neurodiab). J Peripher Nerv Syst. 2014; 19:77–87.
Article4. Feldman EL, Nave KA, Jensen TS, Bennett DL. New horizons in diabetic neuropathy: mechanisms, bioenergetics, and pain. Neuron. 2017; 93:1296–313.
Article5. Pop-Busui R, Boulton AJ, Feldman EL, Bril V, Freeman R, Malik RA, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017; 40:136–54.
Article6. Azmi S, Petropoulos IN, Ferdousi M, Ponirakis G, Alam U, Malik RA. An update on the diagnosis and treatment of diabetic somatic and autonomic neuropathy. F1000Res. 2019; 8 (F1000 Faculty Rev):186.
Article7. Sima AA, Zhang W, Xu G, Sugimoto K, Guberski D, Yorek MA. A comparison of diabetic polyneuropathy in type II diabetic BBZDR/Wor rats and in type I diabetic BB/Wor rats. Diabetologia. 2000; 43:786–93.
Article8. Sima AA. Diabetic neuropathy in type 1 and type 2 diabetes and the effects of C-peptide. J Neurol Sci. 2004; 220:133–6.
Article9. Sima AA, Nathaniel V, Bril V, McEwen TA, Greene DA. Histopathological heterogeneity of neuropathy in insulin-dependent and non-insulin-dependent diabetes, and demonstration of axo-glial dysjunction in human diabetic neuropathy. J Clin Invest. 1988; 81:349–64.
Article10. Callaghan BC, Little AA, Feldman EL, Hughes RA. Enhanced glucose control for preventing and treating diabetic neuropathy. Cochrane Database Syst Rev. 2012; 6:CD007543.
Article11. Christensen DH, Knudsen ST, Gylfadottir SS, Christensen LB, Nielsen JS, Beck-Nielsen H, et al. Metabolic factors, lifestyle habits, and possible polyneuropathy in early type 2 diabetes: a nationwide study of 5,249 patients in the Danish Centre for Strategic Research in type 2 diabetes (DD2) cohort. Diabetes Care. 2020; 43:1266–75.
Article12. Stino AM, Rumora AE, Kim B, Feldman EL. Evolving concepts on the role of dyslipidemia, bioenergetics, and inflammation in the pathogenesis and treatment of diabetic peripheral neuropathy. J Peripher Nerv Syst. 2020; 25:76–84.
Article13. Hossain MJ, Kendig MD, Wild BM, Issar T, Krishnan AV, Morris MJ, et al. Evidence of altered peripheral nerve function in a rodent model of diet-induced prediabetes. Biomedicines. 2020; 8:313.
Article14. Yorek MA. Alternatives to the streptozotocin-diabetic rodent. Int Rev Neurobiol. 2016; 127:89–112.
Article15. O’Brien PD, Sakowski SA, Feldman EL. Mouse models of diabetic neuropathy. ILAR J. 2014; 54:259–72.
Article16. Islam MS. Animal models of diabetic neuropathy: progress since 1960s. J Diabetes Res. 2013; 2013:149452.
Article17. Hargreaves K, Dubner R, Brown F, Flores C, Joris J. A new and sensitive method for measuring thermal nociception in cutaneous hyperalgesia. Pain. 1988; 32:77–88.
Article18. Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods. 1994; 53:55–63.19. Ferrier J, Marchand F, Balayssac D. Assessment of mechanical allodynia in rats using the electronic von Frey test. Bio Protoc. 2016; 6:e1933.20. Beiswenger KK, Calcutt NA, Mizisin AP. Epidermal nerve fiber quantification in the assessment of diabetic neuropathy. Acta Histochem. 2008; 110:351–62.
Article21. Lauria G, Lombardi R, Borgna M, Penza P, Bianchi R, Savino C, et al. Intraepidermal nerve fiber density in rat foot pad: neuropathologic-neurophysiologic correlation. J Peripher Nerv Syst. 2005; 10:202–8.
Article22. Lauria G, Cornblath DR, Johansson O, McArthur JC, Mellgren SI, Nolano M, et al. EFNS guidelines on the use of skin biopsy in the diagnosis of peripheral neuropathy. Eur J Neurol. 2005; 12:747–58.
Article23. Quattrini C, Tavakoli M, Jeziorska M, Kallinikos P, Tesfaye S, Finnigan J, et al. Surrogate markers of small fiber damage in human diabetic neuropathy. Diabetes. 2007; 56:2148–54.
Article24. Reed MJ, Meszaros K, Entes LJ, Claypool MD, Pinkett JG, Gadbois TM, et al. A new rat model of type 2 diabetes: the fatfed, streptozotocin-treated rat. Metabolism. 2000; 49:1390–4.
Article25. Skovso S. Modeling type 2 diabetes in rats using high fat diet and streptozotocin. J Diabetes Investig. 2014; 5:349–58.
Article26. Gao F, Zheng ZM. Animal models of diabetic neuropathic pain. Exp Clin Endocrinol Diabetes. 2014; 122:100–6.
Article27. Mehta BK, Nerkar D, Banerjee S. Characterization of peripheral neuropathy in rat model of type 2 diabetes. Indian J Pharm Educ Res. 2017; 51:92–101.
Article28. Ding Y, Dai X, Zhang Z, Jiang Y, Ma X, Cai X, et al. Proanthocyanidins protect against early diabetic peripheral neuropathy by modulating endoplasmic reticulum stress. J Nutr Biochem. 2014; 25:765–72.
Article29. Ding Y, Dai X, Jiang Y, Zhang Z, Li Y. Functional and morphological effects of grape seed proanthocyanidins on peripheral neuropathy in rats with type 2 diabetes mellitus. Phytother Res. 2014; 28:1082–7.
Article30. Lu M, Yi T, Xiong Y, Wang Q, Yin N. Cortex Mori Radicis extract promotes neurite outgrowth in diabetic rats by activating PI3K/AKT signaling and inhibiting Ca2+ influx associated with the upregulation of transient receptor potential canonical channel 1. Mol Med Rep. 2020; 21:320–8.
Article31. Dang JK, Wu Y, Cao H, Meng B, Huang CC, Chen G, et al. Establishment of a rat model of type II diabetic neuropathic pain. Pain Med. 2014; 15:637–46.
Article32. Sharma AK, Sharma A, Kumari R, Kishore K, Sharma D, Srinivasan BP, et al. Sitagliptin, sitagliptin and metformin, or sitagliptin and amitriptyline attenuate streptozotocin-nicotinamide induced diabetic neuropathy in rats. J Biomed Res. 2012; 26:200–10.33. Moustafa PE, Abdelkader NF, El Awdan SA, El-Shabrawy OA, Zaki HF. Extracellular matrix remodeling and modulation of inflammation and oxidative stress by sulforaphane in experimental diabetic peripheral neuropathy. Inflammation. 2018; 41:1460–76.
Article34. Moustafa PE, Abdelkader NF, El Awdan SA, El-Shabrawy OA, Zaki HF. Liraglutide ameliorated peripheral neuropathy in diabetic rats: involvement of oxidative stress, inflammation and extracellular matrix remodeling. J Neurochem. 2018; 146:173–85.
Article35. Yang XY, Sun L, Xu P, Gong LL, Qiang GF, Zhang L, et al. Effects of salvianolic scid A on plantar microcirculation and peripheral nerve function in diabetic rats. Eur J Pharmacol. 2011; 665:40–6.
Article36. Feng Y, Ge Y, Wu M, Xie Y, Wang M, Chen Y, et al. Long non coding RNAs regulate inflammation in diabetic peripheral neuropathy by acting as ceRNAs targeting miR-146a-5p. Diabetes Metab Syndr Obes. 2020; 13:413–22.37. Feng Y, Chen L, Luo Q, Wu M, Chen Y, Shi X. Involvement of microRNA-146a in diabetic peripheral neuropathy through the regulation of inflammation. Drug Des Devel Ther. 2018; 12:171–7.
Article38. Chen L, Li B, Chen B, Shao Y, Luo Q, Shi X, et al. Thymoquinone alleviates the experimental diabetic peripheral neuropathy by modulation of inflammation. Sci Rep. 2016; 6:31656.
Article39. He J, Yuan GH, Zhang JQ, Guo XH. Approach to creating early diabetic peripheral neuropathy rat model. Beijing Da Xue Xue Bao Yi Xue Ban. 2019; 51:1150–4.40. Coppey LJ, Shevalye H, Obrosov A, Davidson EP, Yorek MA. Determination of peripheral neuropathy in high-fat diet fed low-dose streptozotocin-treated female C57Bl/6J mice and Sprague-Dawley rats. J Diabetes Investig. 2018; 9:1033–40.
Article41. Oza MJ, Kulkarni YA. Formononetin ameliorates diabetic neuropathy by increasing expression of SIRT1 and NGF. Chem Biodivers. 2020; 17:e2000162.
Article42. Davidson EP, Coppey LJ, Holmes A, Yorek MA. Effect of inhibition of angiotensin converting enzyme and/or neutral endopeptidase on vascular and neural complications in high fat fed/low dose streptozotocin-diabetic rats. Eur J Pharmacol. 2012; 677:180–7.
Article43. Davidson EP, Coppey LJ, Holmes A, Dake B, Yorek MA. Effect of treatment of high fat fed/low dose streptozotocin-diabetic rats with Ilepatril on vascular and neural complications. Eur J Pharmacol. 2011; 668:497–506.
Article44. Zhu YB, Jia GL, Wang JW, Ye XY, Lu JH, Chen JL, et al. Activation of CaMKII and GluR1 by the PSD-95-GluN2B couplingdependent phosphorylation of GluN2B in the spinal cord in a rat model of type-2 diabetic neuropathic pain. J Neuropathol Exp Neurol. 2020; 79:800–8.
Article45. Zhou YF, Ying XM, He XF, Shou SY, Wei JJ, Tai ZX, et al. Suppressing PKC-dependent membrane P2X3 receptor upregulation in dorsal root ganglia mediated electroacupuncture analgesia in rat painful diabetic neuropathy. Purinergic Signal. 2018; 14:359–69.
Article46. Zhou CH, Zhang MX, Zhou SS, Li H, Gao J, Du L, et al. SIRT1 attenuates neuropathic pain by epigenetic regulation of mGluR1/5 expressions in type 2 diabetic rats. Pain. 2017; 158:130–9.
Article47. He XF, Wei JJ, Shou SY, Fang JQ, Jiang YL. Effects of electroacupuncture at 2 and 100 Hz on rat type 2 diabetic neuropathic pain and hyperalgesia-related protein expression in the dorsal root ganglion. J Zhejiang Univ Sci B. 2017; 18:239–48.
Article48. Ahlawat A, Sharma S. A new promising simultaneous approach for attenuating type II diabetes mellitus induced neuropathic pain in rats: iNOS inhibition and neuroregeneration. Eur J Pharmacol. 2018; 818:419–28.
Article49. Jain D, Bansal MK, Dalvi R, Upganlawar A, Somani R. Protective effect of diosmin against diabetic neuropathy in experimental rats. J Integr Med. 2014; 12:35–41.
Article50. Davidson EP, Coppey LJ, Holmes A, Yorek MA. Changes in corneal innervation and sensitivity and acetylcholine-mediated vascular relaxation of the posterior ciliary artery in a type 2 diabetic rat. Invest Ophthalmol Vis Sci. 2012; 53:1182–7.
Article51. Coppey L, Davidson E, Shevalye H, Obrosov A, Torres M, Yorek MA. Progressive loss of corneal nerve fibers and sensitivity in rats modeling obesity and type 2 diabetes is reversible with omega-3 fatty acid intervention: supporting cornea analyses as a marker for peripheral neuropathy and treatment. Diabetes Metab Syndr Obes. 2020; 13:1367–84.52. Holmes A, Coppey LJ, Davidson EP, Yorek MA. Rat models of diet-induced obesity and high fat/low dose streptozotocin type 2 diabetes: effect of reversal of high fat diet compared to treatment with enalapril or menhaden oil on glucose utilization and neuropathic endpoints. J Diabetes Res. 2015; 2015:307285.
Article53. Barriere DA, Noll C, Roussy G, Lizotte F, Kessai A, Kirby K, et al. Combination of high-fat/high-fructose diet and low-dose streptozotocin to model long-term type-2 diabetes complications. Sci Rep. 2018; 8:424.
Article54. Coppey L, Davidson E, Shevalye H, Obrosov A, Yorek M. Effect of early and late interventions with dietary oils on vascular and neural complications in a type 2 diabetic rat model. J Diabetes Res. 2019; 2019:5020465.
Article55. Davidson EP, Coppey LJ, Shevalye H, Obrosov A, Kardon RH, Yorek MA. Impaired corneal sensation and nerve loss in a type 2 rat model of chronic diabetes is reversible with combination therapy of menhaden oil, α-lipoic acid, and enalapril. Cornea. 2017; 36:725–31.
Article56. Yorek MS, Davidson EP, Poolman P, Coppey LJ, Obrosov A, Holmes A, et al. Corneal sensitivity to hyperosmolar eye drops: a novel behavioral assay to assess diabetic peripheral neuropathy. Invest Ophthalmol Vis Sci. 2016; 57:2412–9.
Article57. Davidson EP, Holmes A, Coppey LJ, Yorek MA. Effect of combination therapy consisting of enalapril, α-lipoic acid, and menhaden oil on diabetic neuropathy in a high fat/low dose streptozotocin treated rat. Eur J Pharmacol. 2015; 765:258–67.
Article58. Davidson EP, Coppey LJ, Kardon RH, Yorek MA. Differences and similarities in development of corneal nerve damage and peripheral neuropathy and in diet-induced obesity and type 2 diabetic rats. Invest Ophthalmol Vis Sci. 2014; 55:1222–30.
Article59. Coppey LJ, Holmes A, Davidson EP, Yorek MA. Partial replacement with menhaden oil improves peripheral neuropathy in high-fat-fed low-dose streptozotocin type 2 diabetic rat. J Nutr Metab. 2012; 2012:950517.
Article60. Ferhatovic L, Banozic A, Kostic S, Sapunar D, Puljak L. Sex differences in pain-related behavior and expression of calcium/calmodulin-dependent protein kinase II in dorsal root ganglia of rats with diabetes type 1 and type 2. Acta Histochem. 2013; 115:496–504.
Article61. Davidson EP, Coppey LJ, Shevalye H, Obrosov A, Yorek MA. Effect of dietary content of menhaden oil with or without salsalate on neuropathic endpoints in high-fat-fed/low-dose streptozotocin-treated Sprague Dawley Rats. J Diabetes Res. 2018; 2018:2967127.
Article62. Yang R, Li L, Yuan H, Liu H, Gong Y, Zou L, et al. Quercetin relieved diabetic neuropathic pain by inhibiting upregulated P2X4 receptor in dorsal root ganglia. J Cell Physiol. 2019; 234:2756–64.
Article63. Yuan H, Ouyang S, Yang R, Li S, Gong Y, Zou L, et al. Osthole alleviated diabetic neuropathic pain mediated by the P2X4 receptor in dorsal root ganglia. Brain Res Bull. 2018; 142:289–96.
Article64. Fink B, Coppey L, Davidson E, Shevalye H, Obrosov A, Chheda PR, et al. Effect of mitoquinone (Mito-Q) on neuropathic endpoints in an obese and type 2 diabetic rat model. Free Radic Res. 2020; 54:311–8.
Article65. Rao S, Liu S, Zou L, Jia T, Zhao S, Wu B, et al. The effect of sinomenine in diabetic neuropathic pain mediated by the P2X3 receptor in dorsal root ganglia. Purinergic Signal. 2017; 13:227–35.
Article66. Peng H, Zou L, Xie J, Wu H, Wu B, Zhu G, et al. lncRNA NONRATT021972 siRNA decreases diabetic neuropathic pain mediated by the P2X3 receptor in dorsal root ganglia. Mol Neurobiol. 2017; 54:511–23.
Article67. Jia T, Rao J, Zou L, Zhao S, Yi Z, Wu B, et al. Nanoparticle-encapsulated curcumin inhibits diabetic neuropathic pain involving the P2Y12 receptor in the dorsal root ganglia. Front Neurosci. 2018; 11:755.
Article68. Niphakis MJ, Cognetta AB 3rd, Chang JW, Buczynski MW, Parsons LH, Byrne F, et al. Evaluation of NHS carbamates as a potent and selective class of endocannabinoid hydrolase inhibitors. ACS Chem Neurosci. 2013; 4:1322–32.
Article69. Aghdam AM, Shahabi P, Karimi-Sales E, Ghiasi R, SadighEteghad S, Mahmoudi J, et al. Swimming exercise induced reversed expression of miR-96 and its target gene NaV1.3 in diabetic peripheral neuropathy in rats. Chin J Physiol. 2018; 61:124–9.
Article70. Elkholy SE, Elaidy SM, El-Sherbeeny NA, Toraih EA, ElGawly HW. Neuroprotective effects of ranolazine versus pioglitazone in experimental diabetic neuropathy: targeting Nav1.7 channels and PPAR-γ. Life Sci. 2020; 250:117557.
Article71. Boric M, Jelicic Kadic A, Puljak L. Cutaneous expression of calcium/calmodulin-dependent protein kinase II in rats with type 1 and type 2 diabetes. J Chem Neuroanat. 2014; 61-62:140–6.
Article72. Boric M, Skopljanac I, Ferhatovic L, Jelicic Kadic A, Banozic A, Puljak L. Reduced epidermal thickness, nerve degeneration and increased pain-related behavior in rats with diabetes type 1 and 2. J Chem Neuroanat. 2013; 53:33–40.
Article73. Davidson EP, Coppey LJ, Shevalye H, Obrosov A, Yorek MA. Vascular and neural complications in type 2 diabetic rats: improvement by sacubitril/valsartan greater than valsartan alone. Diabetes. 2018; 67:1616–26.
Article74. Wu YB, Li HQ, Ren MS, Li WT, Lv XY, Wang L. CHOP/ORP150 ratio in endoplasmic reticulum stress: a new mechanism for diabetic peripheral neuropathy. Cell Physiol Biochem. 2013; 32:367–79.
Article75. Ferhatovic L, Banozic A, Kostic S, Kurir TT, Novak A, Vrdoljak L, et al. Expression of calcium/calmodulin-dependent protein kinase II and pain-related behavior in rat models of type 1 and type 2 diabetes. Anesth Analg. 2013; 116:712–21.
Article76. Chandramoorthy HC, Bin-Jaliah I, Karari H, Rajagopalan P, Ahmed Shariff ME, Al-Hakami A, et al. MSCs ameliorates DPN induced cellular pathology via [Ca2+ ]i homeostasis and scavenging the pro-inflammatory cytokines. J Cell Physiol. 2018; 233:1330–41.
Article77. Zhang Z, Ding X, Zhou Z, Qiu Z, Shi N, Zhou S, et al. Sirtuin 1 alleviates diabetic neuropathic pain by regulating synaptic plasticity of spinal dorsal horn neurons. Pain. 2019; 160:1082–92.
Article78. Lin JY, He YN, Zhu N, Peng B. Metformin attenuates increase of synaptic number in the rat spinal dorsal horn with painful diabetic neuropathy induced by type 2 diabetes: a stereological study. Neurochem Res. 2018; 43:2232–9.
Article79. Kelany ME, Hakami TM, Omar AH, Abdallah MA. Combination of sitagliptin and insulin against type 2 diabetes mellitus with neuropathy in rats: neuroprotection and role of oxidative and inflammation stress. Pharmacology. 2016; 98:242–50.
Article80. Li K, Shi X, Luo M, Wu P, Zhang M, et al. Taurine protects against myelin damage of sciatic nerve in diabetic peripheral neuropathy rats by controlling apoptosis of schwann cells via NGF/Akt/GSK3β pathway. Exp Cell Res. 2019; 383:111557.
Article81. Hong QX, Xu SY, Dai SH, Zhao WX. Expression profiling of spinal genes in peripheral neuropathy model rats with type 2 diabetes mellitus. Int J Clin Exp Med. 2016; 9:6376–84.82. Xi P, Zhang C, Li Y. Association of TNF-alpha with type-2 diabetic mechanical hyperalgesia in rats. Biomed Res. 2017; 28:305–8.83. Kumar NP, Annamalai AR, Thakur RS. Antinociceptive property of Emblica officinalis Gaertn (Amla) in high fat diet-fed/low dose streptozotocin induced diabetic neuropathy in rats. Indian J Exp Biol. 2009; 47:737–42.84. Meng B, Shen LL, Shi XT, Gong YS, Fan XF, Li J, et al. Effects of curcumin on TTX-R sodium currents of dorsal root ganglion neurons in type 2 diabetic rats with diabetic neuropathic pain. Neurosci Lett. 2015; 605:59–64.
Article85. Nanjundan PK, Arunachalam A, Thakur RS. Antinociceptive property of Trigonella foenum graecum (Fenugreek seeds) in high fat diet-fed/low dose streptozotocin induced diabetic neuropathy in rats. Pharmacologyonline. 2009; 2:24–36.86. Dawane JS, Pandit VA, Bhosale MS, Khatavkar PS. Evaluation of effect of nishamalaki on STZ and HFHF diet induced diabetic neuropathy in Wistar rats. J Clin Diagn Res. 2016; 10:FF01–5.87. Wang S, Wang Z, Li L, Zou L, Gong Y, Jia T, et al. P2Y12 shRNA treatment decreases SGC activation to relieve diabetic neuropathic pain in type 2 diabetes mellitus rats. J Cell Physiol. 2018; 233:9620–8.
Article88. Li L, Sheng X, Zhao S, Zou L, Han X, Gong Y, et al. Nanoparticle-encapsulated emodin decreases diabetic neuropathic pain probably via a mechanism involving P2X3 receptor in the dorsal root ganglia. Purinergic Signal. 2017; 13:559–68.
Article89. Yu W, Zhao GQ, Cao RJ, Zhu ZH, Li K. LncRNA NONRATT021972 was associated with neuropathic pain scoring in patients with type 2 diabetes. Behav Neurol. 2017; 2017:2941297.
Article90. Szkudelski T. Streptozotocin-nicotinamide-induced diabetes in the rat: characteristics of the experimental model. Exp Biol Med (Maywood). 2012; 237:481–90.
Article91. Deuis JR, Dvorakova LS, Vetter I. Methods used to evaluate pain behaviors in rodents. Front Mol Neurosci. 2017; 10:284.
Article92. Fellmann L, Nascimento AR, Tibirica E, Bousquet P. Murine models for pharmacological studies of the metabolic syndrome. Pharmacol Ther. 2013; 137:331–40.
Article93. Srinivasan K, Ramarao P. Animal models in type 2 diabetes research: an overview. Indian J Med Res. 2007; 125:451–72.94. Phillips MS, Liu Q, Hammond HA, Dugan V, Hey PJ, Caskey CJ, et al. Leptin receptor missense mutation in the fatty Zucker rat. Nat Genet. 1996; 13:18–9.
Article95. Peterson RG, Shaw WN, Neel MA, Little LA, Eichberg J. Zucker diabetic fatty rat as a model for non-insulin-dependent diabetes mellitus. Ilar J. 1990; 32:16–9.
Article96. Pick A, Clark J, Kubstrup C, Levisetti M, Pugh W, Bonner-Weir S, et al. Role of apoptosis in failure of beta-cell mass compensation for insulin resistance and beta-cell defects in the male Zucker diabetic fatty rat. Diabetes. 1998; 47:358–64.
Article97. Shibata T, Takeuchi S, Yokota S, Kakimoto K, Yonemori F, Wakitani K. Effects of peroxisome proliferator-activated receptor-alpha and -gamma agonist, JTT-501, on diabetic complications in Zucker diabetic fatty rats. Br J Pharmacol. 2000; 130:495–504.
Article98. Shiota M, Printz RL. Diabetes in Zucker diabetic fatty rat. Methods Mol Biol. 2012; 933:103–23.
Article99. Hempe J, Elvert R, Schmidts HL, Kramer W, Herling AW. Appropriateness of the Zucker diabetic fatty rat as a model for diabetic microvascular late complications. Lab Anim. 2012; 46:32–9.
Article100. Sugimoto K, Rashid IB, Kojima K, Shoji M, Tanabe J, Tamasawa N, et al. Time course of pain sensation in rat models of insulin resistance, type 2 diabetes, and exogenous hyperinsulinaemia. Diabetes Metab Res Rev. 2008; 24:642–50.101. Oltman CL, Coppey LJ, Gellett JS, Davidson EP, Lund DD, Yorek MA. Progression of vascular and neural dysfunction in sciatic nerves of Zucker diabetic fatty and Zucker rats. Am J Physiol Endocrinol Metab. 2005; 289:E113–22.
Article102. Lirk P, Verhamme C, Boeckh R, Stevens MF, ten Hoope W, Gerner P, et al. Effects of early and late diabetic neuropathy on sciatic nerve block duration and neurotoxicity in Zucker diabetic fatty rats. Br J Anaesth. 2015; 114:319–26.
Article103. Davidson EP, Coppey LJ, Holmes A, Lupachyk S, Dake BL, Oltman CL, et al. Characterization of diabetic neuropathy in the Zucker diabetic Sprague-Dawley rat: a new animal model for type 2 diabetes. J Diabetes Res. 2014; 2014:714273.
Article104. Singh J, Yousuf MS, Jones KE, Shelemey PT, Joy T, Macandili H, et al. Characterization of the Nile Grass Rat as a unique model for type 2 diabetic polyneuropathy. J Neuropathol Exp Neurol. 2018; 77:469–78.
Article105. Zhai X, Sun C, Rong P, Li S, McCabe MF, Wang X, et al. A correlative relationship between chronic pain and insulin resistance in Zucker fatty rats: role of downregulation of insulin receptors. J Pain. 2016; 17:404–13.106. Vera G, Lopez-Miranda V, Herradon E, Martin MI, Abalo R. Characterization of cannabinoid-induced relief of neuropathic pain in rat models of type 1 and type 2 diabetes. Pharmacol Biochem Behav. 2012; 102:335–43.
Article107. Romanovsky D, Walker JC, Dobretsov M. Pressure pain precedes development of type 2 disease in Zucker rat model of diabetes. Neurosci Lett. 2008; 445:220–3.
Article108. Li F, Abatan OI, Kim H, Burnett D, Larkin D, Obrosova IG, et al. Taurine reverses neurological and neurovascular deficits in Zucker diabetic fatty rats. Neurobiol Dis. 2006; 22:669–76.
Article109. Otto KJ, Wyse BD, Cabot PJ, Smith MT. Longitudinal study of painful diabetic neuropathy in the Zucker diabetic fatty rat model of type 2 diabetes: impaired basal G-protein activity appears to underpin marked morphine hyposensitivity at 6 months. Pain Med. 2011; 12:437–50.
Article110. De Visser A, Hemming A, Yang C, Zaver S, Dhaliwal R, Jawed Z, et al. The adjuvant effect of hypertension upon diabetic peripheral neuropathy in experimental type 2 diabetes. Neurobiol Dis. 2014; 62:18–30.
Article111. Li S, Sun C, Rong P, Zhai X, Zhang J, Baker M, et al. Auricular vagus nerve stimulation enhances central serotonergic function and inhibits diabetic neuropathy development in Zucker fatty rats. Mol Pain. 2018; 14:1744806918787368.
Article112. Shi J, Jiang K, Li Z. Involvement of spinal glutamate transporter-1 in the development of mechanical allodynia and hyperalgesia associated with type 2 diabetes. J Pain Res. 2016; 9:1121–9.
Article113. Coppey LJ, Gellett JS, Davidson EP, Dunlap JA, Yorek MA. Changes in endoneurial blood flow, motor nerve conduction velocity and vascular relaxation of epineurial arterioles of the sciatic nerve in ZDF-obese diabetic rats. Diabetes Metab Res Rev. 2002; 18:49–56.
Article114. Liu S, Zou L, Xie J, Xie W, Wen S, Xie Q, et al. LncRNA NONRATT021972 siRNA regulates neuropathic pain behaviors in type 2 diabetic rats through the P2X7 receptor in dorsal root ganglia. Mol Brain. 2016; 9:44.
Article115. Feng H, Lu G, Li Q, Liu Z. Inhibition of adenylyl cyclase in the spinal cord alleviates painful diabetic neuropathy in Zucker diabetic fatty rats. Can J Diabetes. 2017; 41:177–83.
Article116. Paniagua N, Giron R, Goicoechea C, Lopez-Miranda V, Vela JM, Merlos M, et al. Blockade of sigma 1 receptors alleviates sensory signs of diabetic neuropathy in rats. Eur J Pain. 2017; 21:61–72.
Article117. Yang Y, Zhang Z, Guan J, Liu J, Ma P, Gu K, et al. Administrations of thalidomide into the rostral ventromedial medulla alleviates painful diabetic neuropathy in Zucker diabetic fatty rats. Brain Res Bull. 2016; 125:144–51.
Article118. Ni GL, Cui R, Shao AM, Wu ZM. Salidroside ameliorates diabetic neuropathic pain in rats by inhibiting neuroinflammation. J Mol Neurosci. 2017; 63:9–16.
Article119. Zhuang HX, Wuarin L, Fei ZJ, Ishii DN. Insulin-like growth factor (IGF) gene expression is reduced in neural tissues and liver from rats with non-insulin-dependent diabetes mellitus, and IGF treatment ameliorates diabetic neuropathy. J Pharmacol Exp Ther. 1997; 283:366–74.120. Gilloteaux J, Subramanian K, Solomon N, Nicaise C. The leptin receptor mutation of the obese Zucker rat causes sciatic nerve demyelination with a centripetal pattern defect. Ultrastruct Pathol. 2018; 42:377–408.
Article121. Sugimoto K, Kojima K, Baba M, Yasujima M. Olmesartan ameliorates peripheral nerve dysfunction in Zucker diabetic fatty rats. J Hypertens. 2011; 29:1337–46.
Article122. Rutten K, Gould SA, Bryden L, Doods H, Christoph T, Pekcec A. Standard analgesics reverse burrowing deficits in a rat CCI model of neuropathic pain, but not in models of type 1 and type 2 diabetes-induced neuropathic pain. Behav Brain Res. 2018; 350:129–38.
Article123. Griggs RB, Donahue RR, Adkins BG, Anderson KL, Thibault O, Taylor BK. Pioglitazone inhibits the development of hyperalgesia and sensitization of spinal nociresponsive neurons in type 2 diabetes. J Pain. 2016; 17:359–73.
Article124. Shevalye H, Watcho P, Stavniichuk R, Dyukova E, Lupachyk S, Obrosova IG. Metanx alleviates multiple manifestations of peripheral neuropathy and increases intraepidermal nerve fiber density in Zucker diabetic fatty rats. Diabetes. 2012; 61:2126–33.
Article125. La Fontaine J, Chen C, Hunt N, Jude E, Lavery L. Type 2 diabetes and metformin influence on fracture healing in an experimental rat model. J Foot Ankle Surg. 2016; 55:955–60.
Article126. Brussee V, Guo G, Dong Y, Cheng C, Martinez JA, Smith D, et al. Distal degenerative sensory neuropathy in a long-term type 2 diabetes rat model. Diabetes. 2008; 57:1664–73.
Article127. Garcia-Perez E, Schonberger T, Sumalla M, Stierstorfer B, Sola R, Doods H, et al. Behavioural, morphological and electrophysiological assessment of the effects of type 2 diabetes mellitus on large and small nerve fibres in Zucker diabetic fatty, Zucker lean and Wistar rats. Eur J Pain. 2018; 22:1457–72.
Article128. Shimoshige Y, Ikuma K, Yamamoto T, Takakura S, Kawamura I, Seki J, et al. The effects of zenarestat, an aldose reductase inhibitor, on peripheral neuropathy in Zucker diabetic fatty rats. Metabolism. 2000; 49:1395–9.
Article129. Russell JW, Berent-Spillson A, Vincent AM, Freimann CL, Sullivan KA, Feldman EL. Oxidative injury and neuropathy in diabetes and impaired glucose tolerance. Neurobiol Dis. 2008; 30:420–9.
Article130. Thakur V, Sadanandan J, Chattopadhyay M. High-mobility group box 1 protein signaling in painful diabetic neuropathy. Int J Mol Sci. 2020; 21:881.
Article131. Ten Hoope W, Hollmann MW, de Bruin K, Verberne HJ, Verkerk AO, Tan HL, et al. Pharmacodynamics and pharmacokinetics of lidocaine in a Rodent model of diabetic neuropathy. Anesthesiology. 2018; 128:609–19.
Article132. Marshall AG, Lee-Kubli C, Azmi S, Zhang M, Ferdousi M, Mixcoatl-Zecuatl T, et al. Spinal disinhibition in experimental and clinical painful diabetic neuropathy. Diabetes. 2017; 66:1380–90.
Article133. Peterson RG. alpha-Glucosidase inhibitors in diabetes: lessons from animal studies. Eur J Clin Invest. 1994; 24 Suppl 3:11–8.134. Oltman CL, Davidson EP, Coppey LJ, Kleinschmidt TL, Yorek MA. Treatment of Zucker diabetic fatty rats with AVE7688 improves vascular and neural dysfunction. Diabetes Obes Metab. 2009; 11:223–33.
Article135. Oltman CL, Davidson EP, Coppey LJ, Kleinschmidt TL, Lund DD, Adebara ET, et al. Vascular and neural dysfunction in Zucker diabetic fatty rats: a difficult condition to reverse. Diabetes Obes Metab. 2008; 10:64–74.
Article136. Davis JE, Cain J, Banz WJ, Peterson RG. Age-related differences in response to high-fat feeding on adipose tissue and metabolic profile in ZDSD rats. ISRN Obes. 2013; 2013:584547.
Article137. Reinwald S, Peterson RG, Allen MR, Burr DB. Skeletal changes associated with the onset of type 2 diabetes in the ZDF and ZDSD rodent models. Am J Physiol Endocrinol Metab. 2009; 296:E765–74.
Article138. Peterson RG, Jackson CV, Zimmerman K, de Winter W, Huebert N, Hansen MK. Characterization of the ZDSD rat: a translational model for the study of metabolic syndrome and type 2 diabetes. J Diabetes Res. 2015; 2015:487816.
Article139. Yang K, Gotzmann J, Kuny S, Huang H, Sauve Y, Chan CB. Five stages of progressive β-cell dysfunction in the laboratory Nile rat model of type 2 diabetes. J Endocrinol. 2016; 229:343–56.
Article140. Chaabo F, Pronczuk A, Maslova E, Hayes K. Nutritional correlates and dynamics of diabetes in the Nile rat (Arvicanthis niloticus): a novel model for diet-induced type 2 diabetes and the metabolic syndrome. Nutr Metab (Lond). 2010; 7:29.
Article141. Santos-Nogueira E, Redondo Castro E, Mancuso R, Navarro X. Randall-Selitto test: a new approach for the detection of neuropathic pain after spinal cord injury. J Neurotrauma. 2012; 29:898–904.
Article142. Jensen TS, Yaksh TL. Comparison of the antinociceptive action of mu and delta opioid receptor ligands in the periaqueductal gray matter, medial and paramedial ventral medulla in the rat as studied by the microinjection technique. Brain Res. 1986; 372:301–12.143. Chapman CR, Casey KL, Dubner R, Foley KM, Gracely RH, Reading AE. Pain measurement: an overview. Pain. 1985; 22:1–31.
Article144. Irwin S, Houde RW, Bennett DR, Hendershot LC, Seevers MH. The effects of morphine methadone and meperidine on some reflex responses of spinal animals to nociceptive stimulation. J Pharmacol Exp Ther. 1951; 101:132–43.145. Elzinga SE, Savelieff MG, O’Brien PD, Mendelson FE, Hayes JM, Feldman EL. Sex differences in insulin resistance, but not peripheral neuropathy, in a diet-induced prediabetes mouse model. Dis Model Mech. 2021; 14:dmm048909.
Article146. Eid SA, Feldman EL. Advances in diet-induced rodent models of metabolically acquired peripheral neuropathy. Dis Model Mech. 2021; 14:dmm049337.
Article147. Liu Y, Sebastian B, Liu B, Zhang Y, Fissel JA, Pan B, et al. Sensory and autonomic function and structure in footpads of a diabetic mouse model. Sci Rep. 2017; 7:41401.
Article148. Schmidt RE. Autonomic neuropathy in experimental models of diabetes mellitus. Handb Clin Neurol. 2014; 126:579–602.
Article149. Morgenstern J, Groener JB, Jende JM, Kurz FT, Strom A, Gopfert J, et al. Neuron-specific biomarkers predict hypo- and hyperalgesia in individuals with diabetic peripheral neuropathy. Diabetologia. 2021; 64:2843–55.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Self-Foot Reflexology on Peripheral Blood Circulation and Peripheral Neuropathy in patients with Diabetes Mellitus
- Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus in Korea
- Gastroesophageal Reflux Disease in Type II Diabetes Mellitus With or Without Peripheral Neuropathy
- Letter: The Necessity of the Simple Tests for Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus Patients without Neuropathic Symptoms in Clinical Practice (Diabetes Metab J 2018;42:442-6)
- Response: The Necessity of the Simple Tests for Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus Patients without Neuropathic Symptoms in Clinical Practice (Diabetes Metab J 2018;42:442–6)