J Cerebrovasc Endovasc Neurosurg.
2022 Mar;24(1):16-23. 10.7461/jcen.2021.E2021.07.001.
Cosmetic outcome after electrocautery versus non-electrocautery dissection of the temporalis muscle for pterional craniotomy
- Affiliations
-
- 1Department of Neurosurgery, Daegu Fatima Hospital, Daegu, Korea
- KMID: 2527591
- DOI: http://doi.org/10.7461/jcen.2021.E2021.07.001
Abstract
Objective
Despite the usefulness of pterional craniotomy (PC), its cosmetic outcome is questionable. Electrocautery (EC) causes injuries to adjacent structures, and it could be a factor that affects the cosmetic outcome. Evaluation of cosmetic outcome is difficult because it is often determined by patient’s subjective criteria. The objective of this study is to compare the cosmetic outcome after EC versus non-electrocautery (NEC) dissection of the temporalis muscle for PC by analyzing long-term follow-up data determined from both physician and patient’s aspects.
Methods
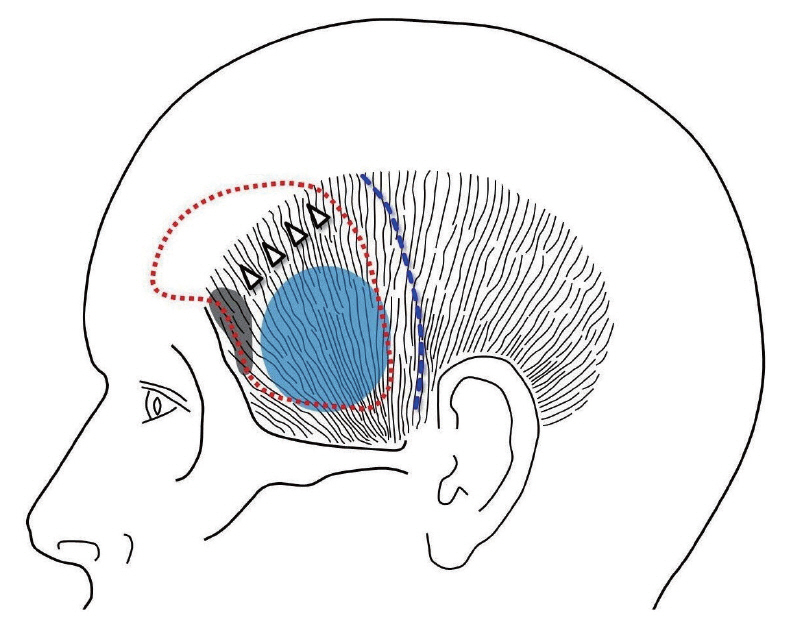
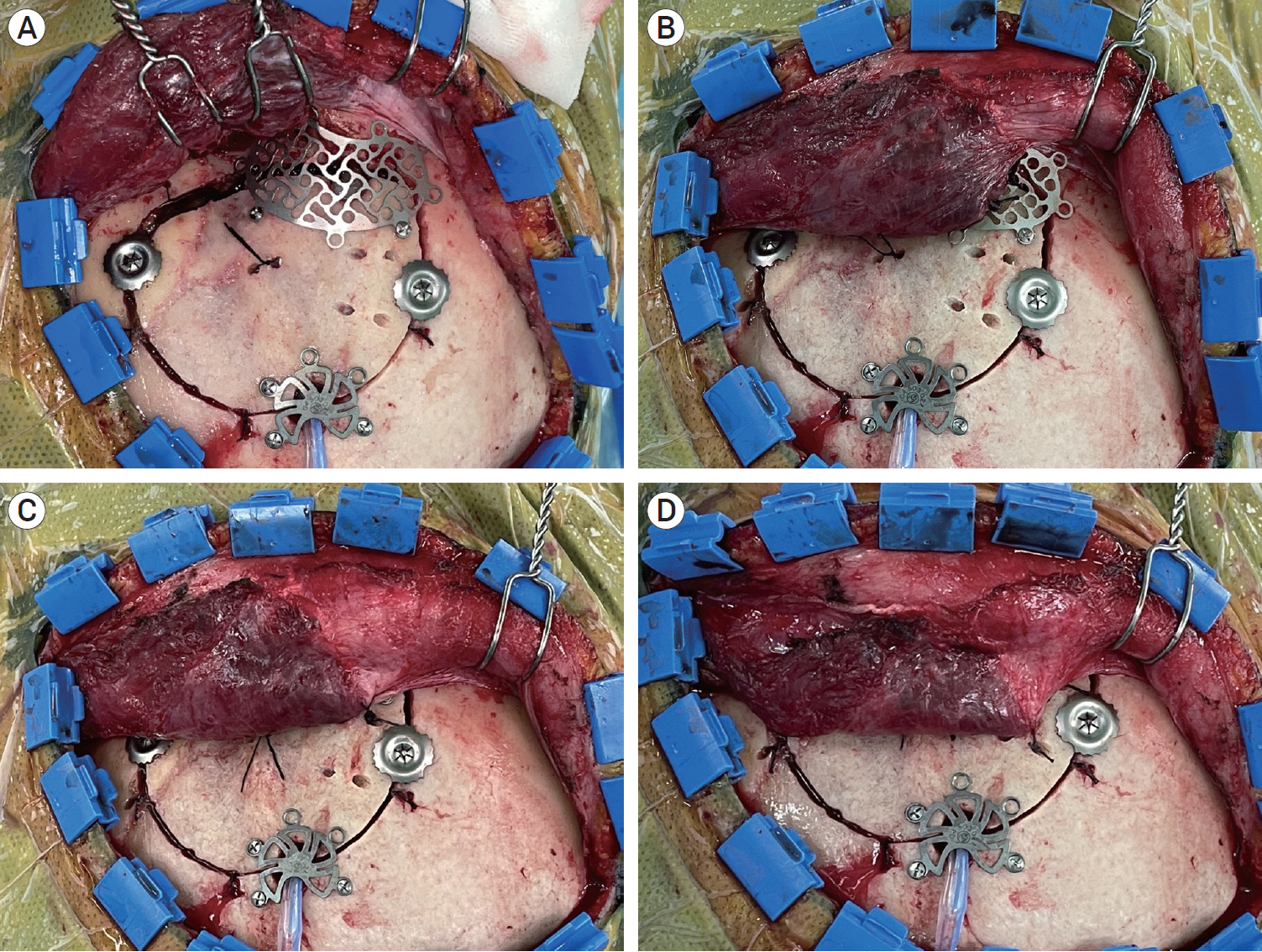
Patients at follow-ups between January 2014 and April 2021 after PCs were enrolled. The keyhole (KH) site, the inferior margin of the temporal line of the frontal bone (ITL), the mid-temporal (mid-T) area, and the posterior incision line (PIL) were inspected by a physician to check the presence of depressions. Patient’s cosmetic satisfaction was categorized into satisfactory, intermediate, or unsatisfactory by a survey. The presence of osteolysis was checked from the radiological images. Patients were classified into two groups; one with EC dissection and another with NEC retrograde dissection using a double-ended dissector.
Results
The incidences of depression at the mid-T area and osteolysis were higher in the EC group (p=0.001, p<0.001). The percentage of satisfactory cosmetic outcome was lower in the EC group (p=0.002). The presences of depression at the mid-T area and osteolysis were related with lower rate of satisfactory outcomes (p<0.001, p<0.001).
Conclusions
NEC dissection causes less destruction to adjacent structures and brings better cosmetic outcome after PC.
Keyword
Figure
Reference
-
1. Alsanad SM, Asim AAH, Gazzaffi IMA, Qureshi NA. History of cautery: The impact of ancient cultures. JAMMR. 2018; Mar. 25(9):1–17.
Article2. Bowles AP Jr. Reconstruction of the temporalis muscle for pterional and cranio-orbital craniotomies. Surg Neurol. 1999; Nov. 52(5):524–9.
Article3. de Andrade Júnior FC, de Andrade FC, de Araujo Filho CM, Carcagnolo Filho J. Dysfunction of the temporalis muscle after pterional craniotomy for intracranial aneurysms. Comparative, prospective and randomized study of one flap versus two flaps dieresis. Arq Neuropsiquiatr. 1998; Jun. 56(2):200–5.
Article4. Hwang SW, Abozed MM, Antoniou AJ, Malek AM, Heilman CB. Postoperative temporalis muscle atrophy and the use of electrocautery: a volumetric MRI comparison. Skull Base. 2010; Sep. 20(5):321–6.
Article5. Im TS, Lee YS, Suh SJ, Lee JH, Ryu KY, Kang DG. The Efficacy of Titanium Burr Hole Cover for Reconstruction of Skull Defect after Burr Hole Trephination of Chronic Subdural Hematoma. Korean J Neurotrauma. 2014; Oct. 10(2):76–81.
Article6. Kadri PA, Al-Mefty O. The anatomical basis for surgical preservation of temporal muscle. J Neurosurg. 2004; Mar. 100(3):517–22.
Article7. Kim S, Matic DB. The anatomy of temporal hollowing: the superficial temporal fat pad. J Craniofac Surg. 2005; Jul. 16(4):651–4.
Article8. Lee MS, Lee YS, Lee JH, Ryu KY, Kang DG. The efficacy of temporal mesh plate floating techinique for keyhole site depression after frontotemporal craniotomy. J Korean Neurotraumatol Soc. 2011; Oct. 7(2):78–82.
Article9. Miyazawa T. Less invasive reconstruction of the temporalis muscle for pterional craniotomy: modified procedures. Surg Neurol. 1998; Oct. 50(4):347–51. discussion 351.
Article10. William T. Bovie and electrosurgery. Surgery. 1996; Apr. 119(4):390–6.11. Oikawa S, Mizuno M, Muraoka S, Kobayashi S. Retrograde dissection of the temporalis muscle preventing muscle atrophy for pterional craniotomy. Technical note. J Neurosurg. 1996; Feb. 84(2):297–9.12. Park JH, Lee YS, Suh SJ, Lee JH, Ryu KY, Kang DG. A simple method for reconstruction of the temporalis muscle using contourable strut plate after pterional craniotomy: Introduction of the surgical techniques and analysis of its efficacy. J Cerebrovasc Endovasc Neurosurg. 2015; Jun. 17(2):93–100.
Article13. Ramachandran M, Aronson JK. John Marshall’s first description of surgical electrocautery. J R Soc Med. 2011; Sep. 104(9):355–60.
Article14. Thiensri T, Limpoka A, Burusapat C. Analysis of factors associated with temporal hollowing after pterional craniotomy. Indian J Plast Surg. 2020; Mar. 53(1):71–82.
Article15. Zager EL, DelVecchio DA, Bartlett SP. Temporal muscle microfixation in pterional craniotomies. Technical note. J Neurosurg. 1993; Dec. 79(6):946–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Subfascial Temporalis Dissection Method in Pterional Craniotomy
- Subfascial Osteoplastic Bone Flap in Pterional Approach: Technical Note
- A Simple Method for Reconstruction of the Temporalis Muscle Using Contourable Strut Plate after Pterional Craniotomy: Introduction of the Surgical Techniques and Analysis of Its Efficacy
- Corneal Astigmatism after Cataract Surgery: The Effect of Electrocautery
- Clinical Analysis of Tonsillectomy by Dissection and Snare, Electrocautery, and Laser