J Korean Neurosurg Soc.
2022 Mar;65(2):297-306. 10.3340/jkns.2021.0114.
Clinical Implications of the Mitotic Index as a Predictive Factor for Malignant Transformation of Atypical Meningiomas
- Affiliations
-
- 1Department of Neurosurgery, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- 2Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2527186
- DOI: http://doi.org/10.3340/jkns.2021.0114
Abstract
Objective
: Intracranial atypical meningiomas have a poor prognosis and high rates of recurrence. Moreover, up to one-third of the recurrences undergo high-grade transformation into malignant meningiomas. We aimed to investigate the clinical factors that can predict the propensity of malignant transformation from atypical to anaplastic meningiomas.
Methods
: Between 2001 and 2018, all patients with atypical meningioma, in whom the tumors had undergone malignant transformation to anaplastic meningioma, were included. The patients’ medical records documenting the diagnosis of atypical meningioma prior to malignant transformation were reviewed to identify the predictors of transformation. The control group comprised 56 patients with atypical meningiomas who were first diagnosed between January 2017 and December 2018 and had no malignant transformation.
Results
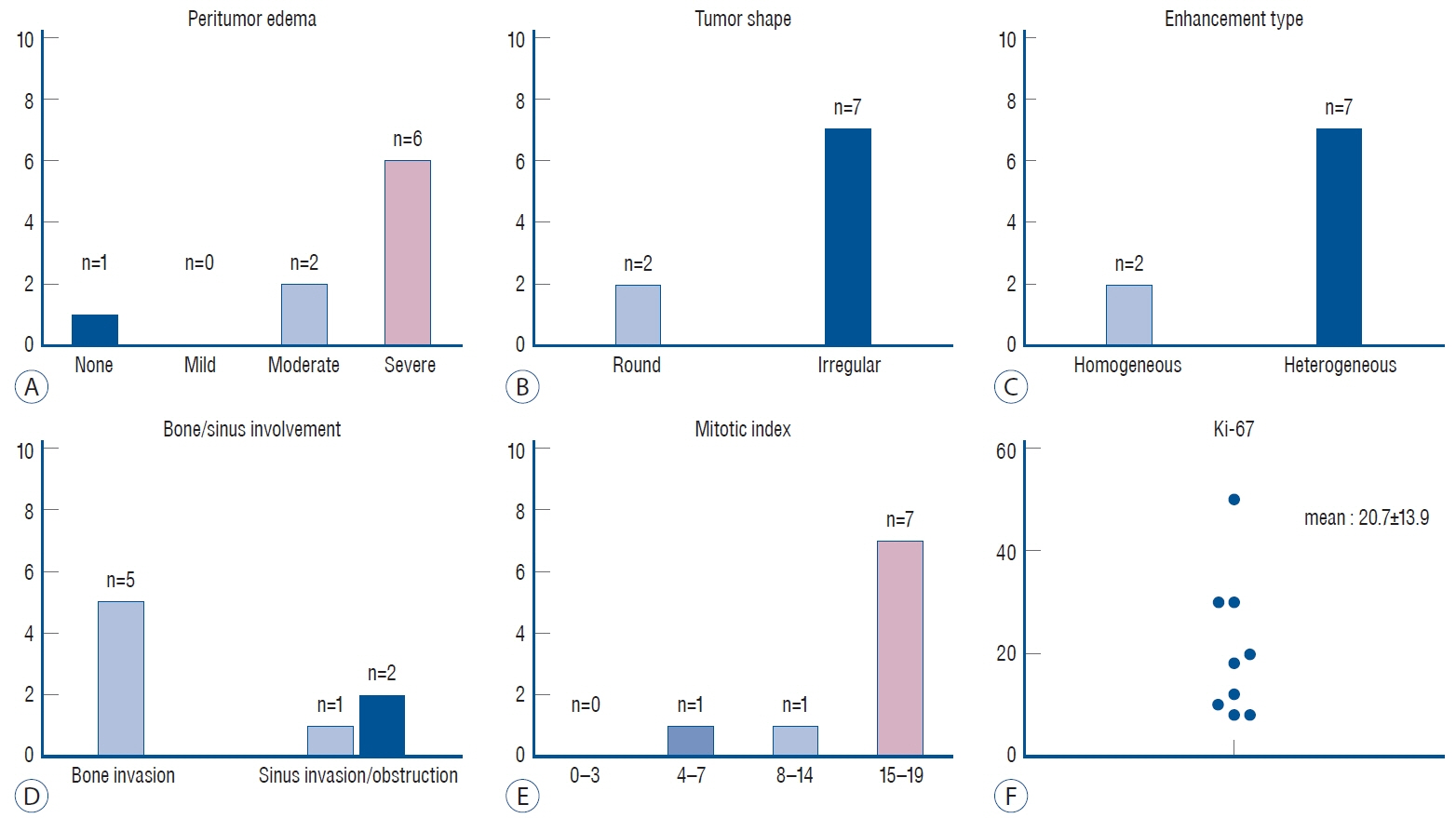
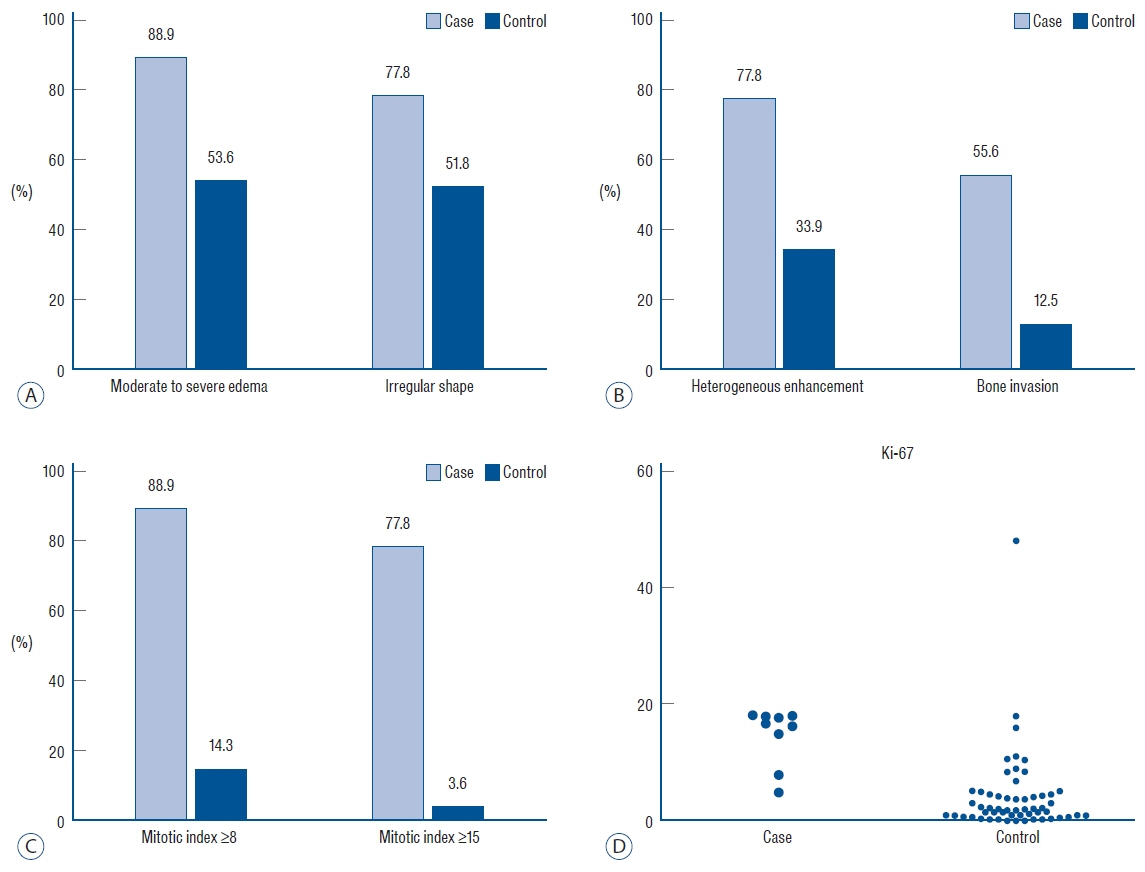
: Nine patients in whom the atypical meningiomas underwent malignant transformation were included. The median time interval from diagnosis of atypical meningioma to malignant transformation was 19 months (range, 7–78). The study group showed a significant difference in heterogeneous enhancement (77.8% vs. 33.9%), bone invasion (55.6% vs. 12.5%), mitotic index (MI; 14.8±4.9 vs. 3.5±3.9), and Ki-67 index (20.7±13.9 vs. 9.5±7.1) compared with the control group. In multivariate analysis, increased MI (odds ratio, 1.436; 95% confidence interval, 1.127–1.900; p=0.004) was the only significant factor for predicting malignant transformation.
Conclusion
: An increased MI within atypical meningiomas might be used as a predictor of malignant transformation. Tumors at high risk for malignant transformation might require more attentive surveillance and management than other atypical meningiomas.
Figure
Reference
-
References
1. Adegbite AB, Khan MI, Paine KW, Tan LK. The recurrence of intracranial meningiomas after surgical treatment. J Neurosurg. 58:51–56. 1983.
Article2. Aghi MK, Carter BS, Cosgrove GR, Ojemann RG, Amin-Hanjani S, Martuza RL, et al. Long-term recurrence rates of atypical meningiomas after gross total resection with or without postoperative adjuvant radiation. Neurosurgery. 64:56–60. discussion 60. 2009.
Article3. Aizer AA, Bi WL, Kandola MS, Lee EQ, Nayak L, Rinne ML, et al. Extent of resection and overall survival for patients with atypical and malignant meningioma. Cancer. 121:4376–4381. 2015.
Article4. Al-Mefty O, Kadri PA, Pravdenkova S, Sawyer JR, Stangeby C, Husain M. Malignant progression in meningioma: documentation of a series and analysis of cytogenetic findings. J Neurosurg. 101:210–218. 2004.
Article5. Alvarez F, Roda JM, Pérez Romero M, Morales C, Sarmiento MA, Blázquez MG. Malignant and atypical meningiomas: a reappraisal of clinical, histological, and computed tomographic features. Neurosurgery. 20:688–694. 1987.
Article6. Ammendola S, Bariani E, Eccher A, Capitanio A, Ghimenton C, Pantanowitz L, et al. The histopathological diagnosis of atypical meningioma: glass slide versus whole slide imaging for grading assessment. Virchows Arch. 478:474–756. 2021.
Article7. Arai H, Beppu T, Wada T, Yoshida Y, Kubo Y, Suzuki M, et al. Pathological analyses of early recurrence and malignant transformation in meningiomas. Brain Tumor Pathol. 15:37–40. 1998.
Article8. Ayerbe J, Lobato RD, de la Cruz J, Alday R, Rivas JJ, Gómez PA, et al. Risk factors predicting recurrence in patients operated on for intracranial meningioma. A multivariate analysis. Acta Neurochir (Wien). 141:921–932. 1999.
Article9. Barresi V, Lionti S, Caliri S, Caffo M. Histopathological features to define atypical meningioma: what does really matter for prognosis? Brain Tumor Pathol. 35:168–180. 2018.
Article10. Bollag RJ, Vender JR, Sharma S. Anaplastic meningioma: progression from atypical and chordoid morphotype with morphologic spectral variation at recurrence. Neuropathology. 30:279–287. 2010.
Article11. Brokinkel B, Spille DC, Brokinkel C, Hess K, Paulus W, Bormann E, et al. The Simpson grading: defining the optimal threshold for gross total resection in meningioma surgery. Neurosurg Rev. 44:1713–1720. 2021.
Article12. Budohoski KP, Clerkin J, Millward CP, O’Halloran PJ, Waqar M, Looby S, et al. Predictors of early progression of surgically treated atypical meningiomas. Acta Neurochir (Wien). 160:1813–1822. 2018.
Article13. Claus EB, Bondy ML, Schildkraut JM, Wiemels JL, Wrensch M, Black PM. Epidemiology of intracranial meningioma. Neurosurgery. 57:1088–1095. discussion 1088-1095. 2005.
Article14. Dietemann JL, Heldt N, Burguet JL, Medjek L, Maitrot D, Wackenheim A. CT findings in malignant meningiomas. Neuroradiology. 23:207–209. 1982.
Article15. Domingues PH, Sousa P, Otero Á, Gonçalves JM, Ruiz L, de Oliveira C, et al. Proposal for a new risk stratification classification for meningioma based on patient age, WHO tumor grade, size, localization, and karyotype. Neuro Oncol. 16:735–747. 2014.
Article16. Duregon E, Cassenti A, Pittaro A, Ventura L, Senetta R, Rudà R, et al. Better see to better agree: phosphohistone H3 increases interobserver agreement in mitotic count for meningioma grading and imposes new specific thresholds. Neuro Oncol. 17:663–669. 2015.
Article17. Goldbrunner R, Minniti G, Preusser M, Jenkinson MD, Sallabanda K, Houdart E, et al. EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol. 17:e383–e391. 2016.
Article18. Ide M, Jimbo M, Kubo O, Yamamoto M, Imanaga H. Peritumoral brain edema associated with meningioma--histological study of the tumor margin and surrounding brain. Neurol Med Chir (Tokyo). 32:65–71. 1992.19. Ildan F, Erman T, Göçer AI, Tuna M, Bağdatoğlu H, Cetinalp E, et al. Predicting the probability of meningioma recurrence in the preoperative and early postoperative period: a multivariate analysis in the midterm follow-up. Skull Base. 17:157–171. 2007.
Article20. Ishino S, Hashimoto N, Fushiki S, Date K, Mori T, Fujimoto M, et al. Loss of material from chromosome arm 1p during malignant progression of meningioma revealed by fluorescent in situ hybridization. Cancer. 83:360–366. 1998.
Article21. Jääskeläinen J, Haltia M, Laasonen E, Wahlström T, Valtonen S. The growth rate of intracranial meningiomas and its relation to histology. An analysis of 43 patients. Surg Neurol. 24:165–172. 1985.
Article22. Jääskeläinen J, Haltia M, Servo A. Atypical and anaplastic meningiomas: radiology, surgery, radiotherapy, and outcome. Surg Neurol. 25:233–242. 1986.
Article23. Jellinger K, Slowik F. Histological subtypes and prognostic problems in meningiomas. J Neurol. 208:279–298. 1975.
Article24. Kawahara Y, Nakada M, Hayashi Y, Kai Y, Hayashi Y, Uchiyama N, et al. Prediction of high-grade meningioma by preoperative MRI assessment. J Neurooncol. 108:147–152. 2012.
Article25. Kim D, Niemierko A, Hwang WL, Stemmer-Rachamimov AO, Curry WT, Barker FG, et al. Histopathological prognostic factors of recurrence following definitive therapy for atypical and malignant meningiomas. J Neurosurg. 128:1123–1132. 2018.
Article26. Krayenbühl N, Pravdenkova S, Al-Mefty O. De novo versus transformed atypical and anaplastic meningiomas: comparisons of clinical course, cytogenetics, cytokinetics, and outcome. Neurosurgery. 61:495–503. discussion 503-504. 2007.27. Kwon SM, Kim JH, Yoo HJ, Kim YH, Hong SH, Cho YH, et al. Predictive factors for high-grade transformation in benign meningiomas. Clin Neurol Neurosurg. 195:105897. 2020.
Article28. Lamszus K, Kluwe L, Matschke J, Meissner H, Laas R, Westphal M. Allelic losses at 1p, 9q, 10q, 14q, and 22q in the progression of aggressive meningiomas and undifferentiated meningeal sarcomas. Cancer Genet Cytogenet. 110:103–110. 1999.
Article29. Lee KD, DePowell JJ, Air EL, Dwivedi AK, Kendler A, McPherson CM. Atypical meningiomas: is postoperative radiotherapy indicated? Neurosurg Focus. 35:E15. 2013.
Article30. Lindblom A, Ruttledge M, Collins VP, Nordenskjöld M, Dumanski JP. Chromosomal deletions in anaplastic meningiomas suggest multiple regions outside chromosome 22 as important in tumor progression. Int J Cancer. 56:354–357. 1994.
Article31. Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol (Berl). 131:803–820. 2016.
Article32. Maiuri F, Mariniello G, Barbato M, Corvino S, Guadagno E, Chiariotti L, et al. Malignant intraventricular meningioma: literature review and case report. Neurosurg Rev. 2021; [Epub ahead of print].
Article33. Mantle RE, Lach B, Delgado MR, Baeesa S, Bélanger G. Predicting the probability of meningioma recurrence based on the quantity of peritumoral brain edema on computerized tomography scanning. J Neurosurg. 91:375–383. 1999.
Article34. Nakasu S, Nakasu Y, Nakajima M, Matsuda M, Handa J. Preoperative identification of meningiomas that are highly likely to recur. J Neurosurg. 90:455–462. 1999.
Article35. Nanda A, Bir SC, Konar S, Maiti T, Kalakoti P, Jacobsohn JA, et al. Outcome of resection of WHO grade II meningioma and correlation of pathological and radiological predictive factors for recurrence. J Clin Neurosci. 31:112–121. 2016.
Article36. Olar A, Wani KM, Sulman EP, Mansouri A, Zadeh G, Wilson CD, et al. Mitotic index is an independent predictor of recurrence-free survival in meningioma. Brain Pathol. 25:266–275. 2015.
Article37. Olmsted WW, McGee TP. Prognosis in meningioma through evaluation of skull bone patterns. Radiology. 123:375–377. 1977.
Article38. Palma L, Celli P, Franco C, Cervoni L, Cantore G. Long-term prognosis for atypical and malignant meningiomas: a study of 71 surgical cases. J Neurosurg. 86:793–800. 1997.
Article39. Perry A, Scheithauer BW, Stafford SL, Lohse CM, Wollan PC. “Malignancy” in meningiomas: a clinicopathologic study of 116 patients, with grading implications. Cancer. 85:2046–2056. 1999.40. Perry A, Stafford SL, Scheithauer BW, Suman VJ, Lohse CM. Meningioma grading: an analysis of histologic parameters. Am J Surg Pathol. 21:1455–1465. 1997.41. Peyre M, Gauchotte G, Giry M, Froehlich S, Pallud J, Graillon T, et al. De novo and secondary anaplastic meningiomas: a study of clinical and histomolecular prognostic factors. Neuro Oncol. 20:1113–1121. 2018.
Article42. Ribalta T, McCutcheon IE, Aldape KD, Bruner JM, Fuller GN. The mitosis-specific antibody anti-phosphohistone-H3 (PHH3) facilitates rapid reliable grading of meningiomas according to WHO 2000 criteria. Am J Surg Pathol. 28:1532–1536. 2004.
Article43. Salah F, Tabbarah A, ALArab Y N, Asmar K, Tamim H, Makki M, et al. Can CT and MRI features differentiate benign from malignant meningiomas? Clin Radiol. 74:898.e15–898.e23. 2019.
Article44. Salpietro FM, Alafaci C, Lucerna S, Iacopino DG, Todaro C, Tomasello F. Peritumoral edema in meningiomas: microsurgical observations of different brain tumor interfaces related to computed tomography. Neurosurgery. 35:638–641. discussion 641-642. 1994.45. San-Miguel T, Cerdá-Nicolás M, Gil-Benso R, Callaghan RC, MuñozHidalgo L, López-Ginés C. Evolution to malignancy: a genetic stepwise study of tumor suppressor genes loss in a recurrent meningioma. Clin Neuropathol. 34:237–239. 2015.
Article46. Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 20:22–39. 1957.
Article47. Sun SQ, Kim AH, Cai C, Murphy RK, DeWees T, Sylvester P, et al. Management of atypical cranial meningiomas, part 1: predictors of recurrence and the role of adjuvant radiation after gross total resection. Neurosurgery. 75:347–354. discussion 354-355; quiz 355. 2014.48. Vranic A, Popovic M, Cör A, Prestor B, Pizem J. Mitotic count, brain invasion, and location are independent predictors of recurrence-free survival in primary atypical and malignant meningiomas: a study of 86 patients. Neurosurgery. 67:1124–1132. 2010.
Article49. Wang F, Xu D, Liu Y, Lin Y, Wei Q, Gao Q, et al. Risk factors associated with postoperative recurrence in atypical intracranial meningioma: analysis of 263 cases at a single neurosurgical centre. Acta Neurochir (Wien). 161:2563–2570. 2019.
Article50. Younis G, Sawaya R. Intracranial osteolytic malignant meningiomas appearing as extracranial soft-tissue masses. Neurosurgery. 30:932–935. 1992.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Recurrence of a Lateral Ventricle Meningioma with Malignant Transformation
- Immunohistochemical Analysis of Progesterone Receptor in Intracranial Meningiomas
- Correlation of histopathologic classification with proliferative activity and DNA ploidy in 120 intracranial meningiomas, with special reference to atypical meningioma
- Relationship between Flow Cytometric Features and Clinical Behavior of Meningiomas
- Malignant Transformation of Meningioma With TERT Promoter Mutation: A Case Report