Clin Exp Otorhinolaryngol.
2022 Feb;15(1):49-59. 10.21053/ceo.2021.00920.
Cytokines and Inflammation in Meniere Disease
- Affiliations
-
- 1Otology and Neurotology Group CTS495, Department of Genomic Medicine, Centre for Genomics and Oncological Research (GENYO), Pfizer-University of Granada-Junta de Andalucía, PTS, Granada, Spain
- 2Department of Otolaryngology, Instituto de Investigación Biosanitaria ibs. Granada, Hospital Universitario Virgen de las Nieves, Granada, Spain
- 3Sensorineural Pathology Programme, Centro de Investigación Biomédica en Red en Enfermedades Raras, CIBERER, Madrid, Spain
- 4Department of Surgery, Division of Otolaryngology, Universidad de Granada, Granada, Spain
- KMID: 2527112
- DOI: http://doi.org/10.21053/ceo.2021.00920
Abstract
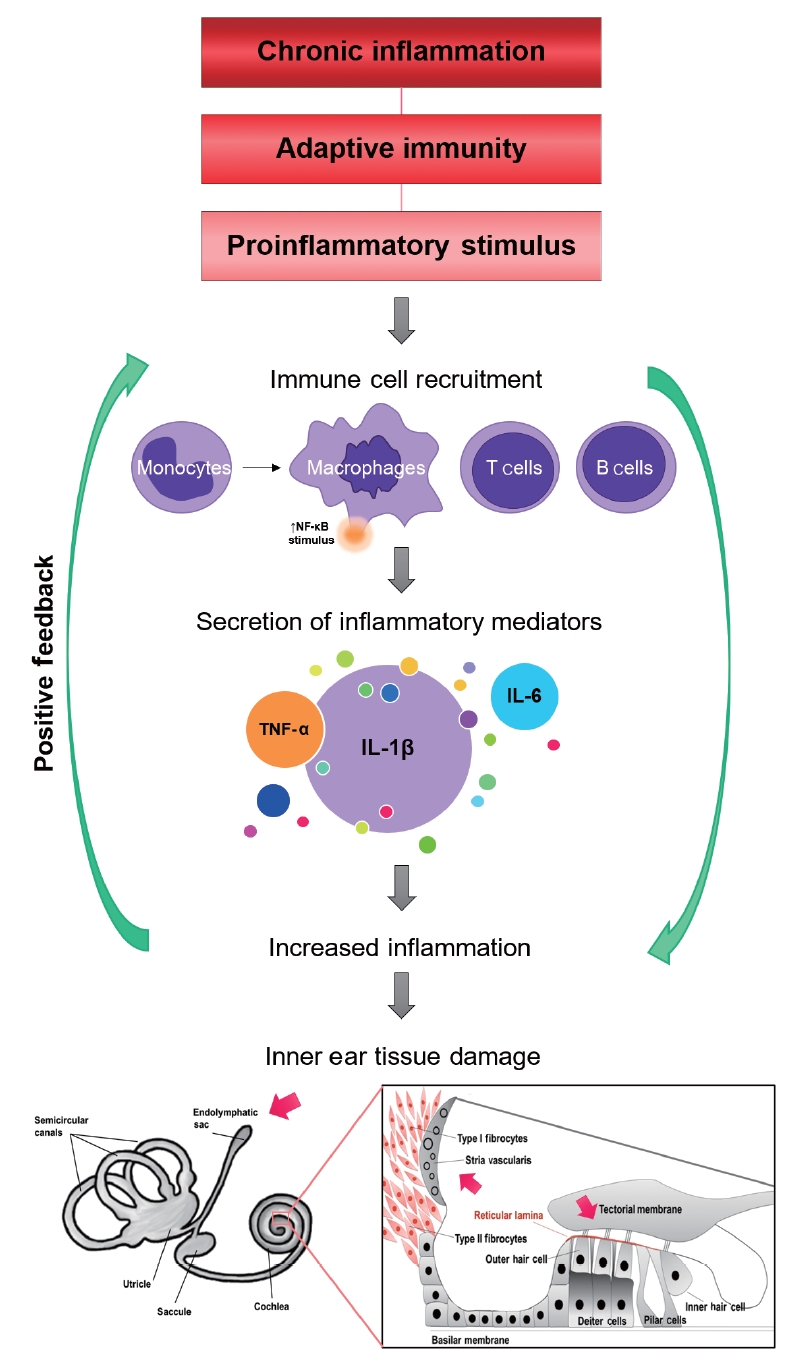
- Meniere disease (MD) is a rare set of conditions associated with the accumulation of endolymph in the cochlear duct and the vestibular labyrinth with a decrease of endocochlear potential. It is considered a chronic inflammatory disorder of the inner ear with a multifactorial origin. The clinical syndrome includes several groups of patients with a core phenotype: sensorineural hearing loss, episodes of vertigo, and tinnitus with a non-predictable course. Genetic factors and the innate immune response seem to play a central role in the pathophysiology of the condition. Autoimmune MD should be diagnosed if a patient fulfills the diagnostic criteria for MD and one of the following autoimmune disorders: autoimmune thyroid disease, psoriasis, autoimmune arthritis, ankylosing spondylitis, or systemic lupus erythematosus. We summarize the evidence to support autoimmune MD as an endophenotype in bilateral MD associated with the allelic variant rs4947296 and nuclear factor-kappa B (NF-κB)-mediated inflammation, the role of cytokines (particularly interleukin-1β and tumor necrosis factor-α) in defining a subset of patients with autoinflammation, and the potential role of cytokines as biomarkers to distinguish between patients with MD and vestibular migraine. Finally, we also introduce a list of potential drugs that could regulate the immune response in MD with potential for repurposing in clinical trials.
Figure
Cited by 1 articles
-
Reprogramming Macrophage Phenotypes With Photobiomodulation for Improved Inflammation Control in ENT Organ Tissues
Ken Woo, Yeon Soo Kim, Celine Abueva, Seung Hoon Woo
Clin Exp Otorhinolaryngol. 2025;18(1):1-13. doi: 10.21053/ceo.2024.00286.
Reference
-
1. Amanat S, Requena T, Lopez-Escamez JA. A systematic review of extreme phenotype strategies to search for rare variants in genetic studies of complex disorders. Genes (Basel). 2020; Aug. 11(9):987.
Article2. Espinosa-Sanchez JM, Lopez-Escamez JA. Meniere’s disease. Handb Clin Neurol. 2016; 137:257–77.3. Stahle J, Friberg U, Svedberg A. Long-term progression of Meniere’s disease. Acta Otolaryngol Suppl. 1991; 485:78–83.
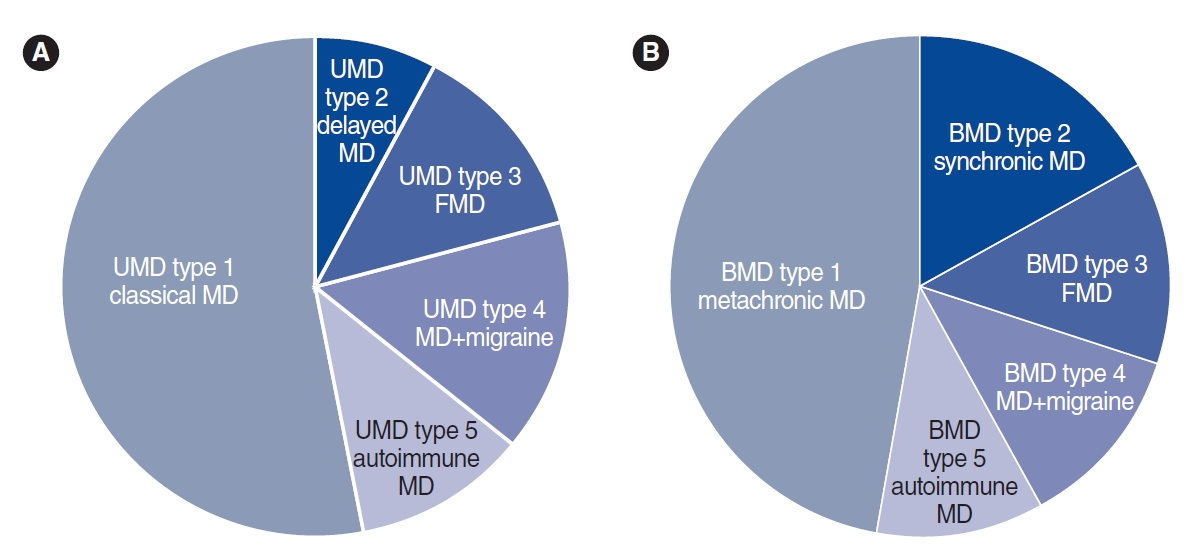
Article4. Lopez-Escamez JA, Carey J, Chung WH, Goebel JA, Magnusson M, Mandala M, et al. Diagnostic criteria for Meniere’s disease. J Vestib Res. 2015; Mar. 25(1):1–7.5. Frejo L, Soto-Varela A, Santos-Perez S, Aran I, Batuecas-Caletrio A, Perez-Guillen V, et al. Clinical subgroups in bilateral Meniere disease. Front Neurol. 2016; Oct. 7:182.
Article6. Frejo L, Martin-Sanz E, Teggi R, Trinidad G, Soto-Varela A, SantosPerez S, et al. Extended phenotype and clinical subgroups in unilateral Meniere disease: a cross-sectional study with cluster analysis. Clin Otolaryngol. 2017; Dec. 42(6):1172–80.
Article7. Requena T, Espinosa-Sanchez JM, Cabrera S, Trinidad G, Soto-Varela A, Santos-Perez S, et al. Familial clustering and genetic heterogeneity in Meniere’s disease. Clin Genet. 2014; Mar. 85(3):245–52.
Article8. Lee JM, Kim MJ, Jung J, Kim HJ, Seo YJ, Kim SH. Genetic aspects and clinical characteristics of familial Meniere’s disease in a South Korean population. Laryngoscope. 2015; Sep. 125(9):2175–80.
Article9. Roman-Naranjo P, Gallego-Martinez A, Lopez Escamez JA. Genetics of vestibular syndromes. Curr Opin Neurol. 2018; Feb. 31(1):105–10.
Article10. Birgerson L, Gustavson KH, Stahle J. Familial Meniere’s disease: a genetic investigation. Am J Otol. 1987; Jul. 8(4):323–6.11. Klar J, Frykholm C, Friberg U, Dahl N. A Meniere’s disease gene linked to chromosome 12p12.3. Am J Med Genet B Neuropsychiatr Genet. 2006; Jul. 141(5):463–7.
Article12. Morrison AW, Bailey ME, Morrison GA. Familial Meniere’s disease: clinical and genetic aspects. J Laryngol Otol. 2009; Jan. 123(1):29–37.13. Oliveira CA, Ferrari I, Messias CI. Occurrence of familial Meniere’s syndrome and migraine in Brasilia. Ann Otol Rhinol Laryngol. 2002; Mar. 111(3 Pt 1):229–36.
Article14. Arweiler-Harbeck D, Horsthemke B, Jahnke K, Hennies HC. Genetic aspects of familial Meniere’s disease. Otol Neurotol. 2011; Jun. 32(4):695–700.15. Hietikko E, Kotimaki J, Okuloff A, Sorri M, Mannikko M. A replication study on proposed candidate genes in Meniere’s disease, and a review of the current status of genetic studies. Int J Audiol. 2012; Nov. 51(11):841–5.16. Roman-Naranjo P, Gallego-Martinez A, Soto-Varela A, Aran I, Moleon M, Espinosa-Sanchez JM, et al. Burden of rare variants in the OTOG gene in familial Meniere’s disease. Ear Hear. 2020; Nov/Dec. 41(6):1598–605.
Article17. Sajjadi H, Paparella MM. Meniere’s disease. Lancet. 2008; Aug. 372(9636):406–14.
Article18. Paparella MM, Djalilian HR. Etiology, pathophysiology of symptoms, and pathogenesis of Meniere’s disease. Otolaryngol Clin North Am. 2002; Jun. 35(3):529–45.
Article19. Greco A, Gallo A, Fusconi M, Marinelli C, Macri GF, de Vincentiis M. Meniere’s disease might be an autoimmune condition. Autoimmun Rev. 2012; Aug. 11(10):731–8.
Article20. Kim SH, Kim JY, Lee HJ, Gi M, Kim BG, Choi JY. Autoimmunity as a candidate for the etiopathogenesis of Meniere’s disease: detection of autoimmune reactions and diagnostic biomarker candidate. PLoS One. 2014; Oct. 9(10):e111039.
Article21. Joannovic D. Zur Wirkung fermentativ gewonner spaltungsprodukte aus Geweben und Bakterien. Wein Klin Wschr. 1920; 70:1410–11.22. Masugi M, Tomizuka Y. Uber die spezifisch zytotoxischen Veranderungen der Niere und sehr Leber durch das spezifische Antiserum (Nephrotoxin und Hepatoxin). Trans Jap Pathol. 1931; 21:329–41.23. Lehnhardt E. Pathogenesis of sudden hearing disorders. Dtsch Gesundheitsw. 1958; Jan. 13(4):105–9.24. Kikuchi M. On the “sympathetic otitis.” Zibi Rinsyo Kyoto. Dtsch Gesundheitsw. 1959; 52:600.25. Beickert P. On the problem of perception deafness and autoallergy. Z Laryngol Rhinol Otol. 1961; Nov. 40:837–42.26. Yoshihiko T, Yukihiro S. Studies on experimental allergic (isoimmune) labyrinthitis in guinea pigs. Acta Otolaryngol. 1964; Jul. 58:49–64.
Article27. McCabe BF. Autoimmune sensorineural hearing loss. Ann Otol Rhinol Laryngol. 1979; Sep-Oct. 88(5 Pt 1):585–9.
Article28. Verdoodt D, Van Camp G, Ponsaerts P, Van Rompaey V. On the pathophysiology of DFNA9: effect of pathogenic variants in the COCH gene on inner ear functioning in human and transgenic mice. Hear Res. 2021; Mar. 401:108162.
Article29. Baruah P. Cochlin in autoimmune inner ear disease: is the search for an inner ear autoantigen over. Auris Nasus Larynx. 2014; Dec. 41(6):499–501.
Article30. Danial-Farran N, Chervinsky E, Nadar-Ponniah PT, Cohen Barak E, Taiber S, Khayat M, et al. Homozygote loss-of-function variants in the human COCH gene underlie hearing loss. Eur J Hum Genet. 2021; Feb. 29(2):338–42.
Article31. Jung J, Yoo JE, Choe YH, Park SC, Lee HJ, Lee HJ, et al. Cleaved cochlin sequesters pseudomonas aeruginosa and activates innate immunity in the inner ear. Cell Host Microbe. 2019; Apr. 25(4):513–25.
Article32. Hughes GB, Kinney SE, Barna BP, Calabrese LH. Autoimmune reactivity in Meniere’s disease: a preliminary report. Laryngoscope. 1983; Apr. 93(4):410–7.
Article33. Tyrrell JS, Whinney DJ, Ukoumunne OC, Fleming LE, Osborne NJ. Prevalence, associated factors, and comorbid conditions for Meniere’s disease. Ear Hear. 2014; Jul-Aug. 35(4):e162–9.34. Hietikko E, Kotimaki J, Sorri M, Mannikko M. High incidence of Meniere-like symptoms in relatives of Meniere patients in the areas of Oulu University Hospital and Kainuu Central Hospital in Finland. Eur J Med Genet. 2013; Jun. 56(6):279–85.
Article35. Gazquez I, Soto-Varela A, Aran I, Santos S, Batuecas A, Trinidad G, et al. High prevalence of systemic autoimmune diseases in patients with Meniere’s disease. PLoS One. 2011; 6(10):e26759.36. Bovo R, Ciorba A, Martini A. Vertigo and autoimmunity. Eur Arch Otorhinolaryngol. 2010; Jan. 267(1):13–9.
Article37. Chiarella G, Di Domenico M, Petrolo C, Saccomanno M, Rothenberger R, Giordano A, et al. A proteomics-driven assay defines specific plasma protein signatures in different stages of Meniere’s disease. J Cell Biochem. 2014; Jun. 115(6):1097–100.38. Lopez-Escamez JA, Saenz-Lopez P, Gazquez I, Moreno A, Gonzalez-Oller C, Soto-Varela A, et al. Polymorphisms of CD16A and CD32 Fcγ receptors and circulating immune complexes in Meniere’s disease: a case-control study. BMC Med Genet. 2011; Jan. 12:2.39. Gloddek B, Arnold W. Clinical and experimental studies of autoimmune inner ear disease. Acta Otolaryngol Suppl. 2002; (548):10–4.
Article40. Yoo TJ, Yazawa Y, Tomoda K, Floyd R. Type II collagen-induced autoimmune endolymphatic hydrops in guinea pig. Science. 1983; Oct. 222(4619):65–7.
Article41. Yoo TJ. Etiopathogenesis of Meniere’s disease: a hypothesis. Ann Otol Rhinol Laryngol Suppl. 1984; Sep-Oct. 113:6–12.
Article42. Brookes GB. Circulating immune complexes in Meniere’s disease. Arch Otolaryngol Head Neck Surg. 1986; May. 112(5):536–40.
Article43. Yoo TJ, Shea J Jr, Ge X, Kwon SS, Yazawa Y, Sener O, et al. Presence of autoantibodies in the sera of Meniere’s disease. Ann Otol Rhinol Laryngol. 2001; May. 110(5 Pt 1):425–9.
Article44. Bernstein JM, Shanahan TC, Schaffer FM. Further observations on the role of the MHC genes and certain hearing disorders. Acta Otolaryngol. 1996; Sep. 116(5):666–71.
Article45. Gazquez I, Moreno A, Aran I, Soto-Varela A, Santos S, Perez-Garrigues H, et al. MICA-STR A.4 is associated with slower hearing loss progression in patients with Meniere’s disease. Otol Neurotol. 2012; Feb. 33(2):223–9.46. Requena T, Gazquez I, Moreno A, Batuecas A, Aran I, Soto-Varela A, et al. Allelic variants in TLR10 gene may influence bilateral affectation and clinical course of Meniere’s disease. Immunogenetics. 2013; May. 65(5):345–55.
Article47. Cabrera S, Sanchez E, Requena T, Martinez-Bueno M, Benitez J, Perez N, et al. Intronic variants in the NFKB1 gene may influence hearing forecast in patients with unilateral sensorineural hearing loss in Meniere’s disease. PLoS One. 2014; Nov. 9(11):e112171.
Article48. Frejo L, Requena T, Okawa S, Gallego-Martinez A, Martinez-Bueno M, Aran I, et al. Regulation of Fn14 receptor and NF-κB underlies inflammation in Meniere’s disease. Front Immunol. 2017; Dec. 8:1739.
Article49. Xu WD, Zhao Y, Liu Y. Role of the TWEAK/Fn14 pathway in autoimmune diseases. Immunol Res. 2016; Feb. 64(1):44–50.
Article50. Rask-Andersen H, Danckwardt-Lilliestrom N, Friberg U, House W. Lymphocyte-macrophage activity in the human endolymphatic sac. Acta Otolaryngol Suppl. 1991; 485:15–7.
Article51. Okano T, Nakagawa T, Ito J. Distribution of bone marrow-derived cells in the vestibular end organs and the endolymphatic sac. Acta Otolaryngol Suppl. 2010; Nov. (563):88–94.
Article52. Moller MN, Kirkeby S, Vikesa J, Nielsen FC, Caye-Thomasen P. Gene expression in the human endolymphatic sac: the solute carrier molecules in endolymphatic fluid homeostasis. Otol Neurotol. 2015; Jun. 36(5):915–22.53. Moller MN, Kirkeby S, Vikesa J, Nielsen FC, Caye-Thomasen P. Expression of histamine receptors in the human endolymphatic sac: the molecular rationale for betahistine use in Menieres disease. Eur Arch Otorhinolaryngol. 2016; Jul. 273(7):1705–10.
Article54. Hu BH, Zhang C, Frye MD. Immune cells and non-immune cells with immune function in mammalian cochleae. Hear Res. 2018; May. 362:14–24.
Article55. O’Malley JT, Nadol JB Jr, McKenna MJ. Anti CD163+, Iba1+, and CD68+ cells in the adult human inner ear: normal distribution of an unappreciated class of macrophages/microglia and implications for inflammatory otopathology in humans. Otol Neurotol. 2016; Jan. 37(1):99–108.56. Liu W, Molnar M, Garnham C, Benav H, Rask-Andersen H. Macrophages in the human cochlea: saviors or predators: a study using super-resolution immunohistochemistry. Front Immunol. 2018; Feb. 9:223.57. Kampfe Nordstrom C, Danckwardt-Lilliestrom N, Laurell G, Liu W, Rask-Andersen H. The human endolymphatic sac and inner ear immunity: macrophage interaction and molecular expression. Front Immunol. 2019; Feb. 9:3181.58. Moller MN, Kirkeby S, Vikesa J, Nielsen FC, Caye-Thomasen P. Gene expression demonstrates an immunological capacity of the human endolymphatic sac. Laryngoscope. 2015; Aug. 125(8):E269–75.59. Broderick L. Hereditary autoinflammatory disorders: recognition and treatment. Immunol Allergy Clin North Am. 2019; Feb. 39(1):13–29.60. Martinez-Quiles N, Goldbach-Mansky R. Updates on autoinflammatory diseases. Curr Opin Immunol. 2018; Dec. 55:97–105.
Article61. Adams JC, Seed B, Lu N, Landry A, Xavier RJ. Selective activation of nuclear factor kappa B in the cochlea by sensory and inflammatory stress. Neuroscience. 2009; May. 160(2):530–9.
Article62. Nie H, Zheng Y, Li R, Guo TB, He D, Fang L, et al. Phosphorylation of FOXP3 controls regulatory T cell function and is inhibited by TNF-α in rheumatoid arthritis. Nat Med. 2013; Mar. 19(3):322–8.
Article63. Ren J, Li H, Lu Y. The determinations of tumor necrosis factor and interleukin 6 in serum of patients with sudden sensorineural hearing loss. Lin Chuang Er Bi Yan Hou Ke Za Zhi. 1998; Jul. 12(7):311–3.64. Rahman MU, Poe DS, Choi HK. Etanercept therapy for immunemediated cochleovestibular disorders: preliminary results in a pilot study. Otol Neurotol. 2001; Sep. 22(5):619–24.
Article65. Keithley EM, Wang X, Barkdull GC. Tumor necrosis factor alpha can induce recruitment of inflammatory cells to the cochlea. Otol Neurotol. 2008; Sep. 29(6):854–9.66. Wang X, Truong T, Billings PB, Harris JP, Keithley EM. Blockage of immune-mediated inner ear damage by etanercept. Otol Neurotol. 2003; Jan. 24(1):52–7.
Article67. Lobo D, Trinidad A, Garcia-Berrocal JR, Verdaguer JM, Ramirez-Camacho R. TNFalpha blockers do not improve the hearing recovery obtained with glucocorticoid therapy in an autoimmune experimental labyrinthitis. Eur Arch Otorhinolaryngol. 2006; Jul. 263(7):622–6.
Article68. Kassner SS, Schottler S, Bonaterra GA, Stern-Strater J, Sommer U, Hormann K, et al. Proinflammatory and proadhesive activation of lymphocytes and macrophages in sudden sensorineural hearing loss. Audiol Neurootol. 2011; 16(4):254–62.
Article69. Suslu N, Yilmaz T, Gursel B. Utility of immunologic parameters in the evaluation of Meniere’s disease. Acta Otolaryngol. 2009; Nov. 129(11):1160–5.
Article70. Svrakic M, Pathak S, Goldofsky E, Hoffman R, Chandrasekhar SS, Sperling N, et al. Diagnostic and prognostic utility of measuring tumor necrosis factor in the peripheral circulation of patients with immune-mediated sensorineural hearing loss. Arch Otolaryngol Head Neck Surg. 2012; Nov. 138(11):1052–8.
Article71. Pathak S, Stern C, Vambutas A. N-Acetylcysteine attenuates tumor necrosis factor alpha levels in autoimmune inner ear disease patients. Immunol Res. 2015; Dec. 63(1-3):236–45.
Article72. Blesa S, Cortijo J, Mata M, Serrano A, Closa D, Santangelo F, et al. Oral N-acetylcysteine attenuates the rat pulmonary inflammatory response to antigen. Eur Respir J. 2003; Mar. 21(3):394–400.
Article73. Angeli SI, Abi-Hachem RN, Vivero RJ, Telischi FT, Machado JJ. LN-Acetylcysteine treatment is associated with improved hearing outcome in sudden idiopathic sensorineural hearing loss. Acta Otolaryngol. 2012; Apr. 132(4):369–76.
Article74. Thornberry NA, Bull HG, Calaycay JR, Chapman KT, Howard AD, Kostura MJ, et al. A novel heterodimeric cysteine protease is required for interleukin-1 beta processing in monocytes. Nature. 1992; Apr. 356(6372):768–74.
Article75. Zheng D, Liwinski T, Elinav E. Inflammasome activation and regulation: toward a better understanding of complex mechanisms. Cell Discov. 2020; Jun. 6:36.
Article76. Andrei C, Margiocco P, Poggi A, Lotti LV, Torrisi MR, Rubartelli A. Phospholipases C and A2 control lysosome-mediated IL-1 beta secretion: implications for inflammatory processes. Proc Natl Acad Sci U S A. 2004; 101(26):9745–50.77. Sims JE, Smith DE. The IL-1 family: regulators of immunity. Nat Rev Immunol. 2010; Feb. 10(2):89–102.
Article78. Pathak S, Vambutas A. Autoimmune inner ear disease patient-associated 28-kDa proinflammatory IL-1β fragment results from caspase-7-mediated cleavage in vitro. JCI Insight. 2020; Feb. 5(3):e130845.
Article79. Mandrup-Poulsen T, Pickersgill L, Donath MY. Blockade of interleukin 1 in type 1 diabetes mellitus. Nat Rev Endocrinol. 2010; Mar. 6(3):158–66.
Article80. Arend WP. Cytokine imbalance in the pathogenesis of rheumatoid arthritis: the role of interleukin-1 receptor antagonist. Semin Arthritis Rheum. 2001; Apr. 30(5 Suppl 2):1–6.
Article81. Luheshi NM, Rothwell NJ, Brough D. Dual functionality of interleukin-1 family cytokines: implications for anti-interleukin-1 therapy. Br J Pharmacol. 2009; Aug. 157(8):1318–29.
Article82. Ligumsky M, Simon PL, Karmeli F, Rachmilewitz D. Role of interleukin 1 in inflammatory bowel disease: enhanced production during active disease. Gut. 1990; Jun. 31(6):686–9.
Article83. Gosselin D, Rivest S. Role of IL-1 and TNF in the brain: twenty years of progress on a Dr. Jekyll/Mr. Hyde duality of the innate immune system. Brain Behav Immun. 2007; Mar. 21(3):281–9.
Article84. Hawkins PN, Lachmann HJ, McDermott MF. Interleukin-1-receptor antagonist in the Muckle-Wells syndrome. N Engl J Med. 2003; Jun. 348(25):2583–4.
Article85. Hull KM, Shoham N, Chae JJ, Aksentijevich I, Kastner DL. The expanding spectrum of systemic autoinflammatory disorders and their rheumatic manifestations. Curr Opin Rheumatol. 2003; Jan. 15(1):61–9.
Article86. Pathak S, Goldofsky E, Vivas EX, Bonagura VR, Vambutas A. IL-1β is overexpressed and aberrantly regulated in corticosteroid nonresponders with autoimmune inner ear disease. J Immunol. 2011; Feb. 186(3):1870–9.
Article87. Nakanishi H, Kawashima Y, Kurima K, Chae JJ, Ross AM, PintoPatarroyo G, et al. NLRP3 mutation and cochlear autoinflammation cause syndromic and nonsyndromic hearing loss DFNA34 responsive to anakinra therapy. Proc Natl Acad Sci U S A. 2017; Sep. 114(37):E7766–75.88. Gattorno M, Martini A. Beyond the NLRP3 inflammasome: autoinflammatory diseases reach adolescence. Arthritis Rheum. 2013; May. 65(5):1137–47.89. Agostini L, Martinon F, Burns K, McDermott MF, Hawkins PN, Tschopp J. NALP3 forms an IL-1beta-processing inflammasome with increased activity in Muckle-Wells autoinflammatory disorder. Immunity. 2004; Mar. 20(3):319–25.
Article90. Stojanov S, Kastner DL. Familial autoinflammatory diseases: genetics, pathogenesis and treatment. Curr Opin Rheumatol. 2005; Sep. 17(5):586–99.
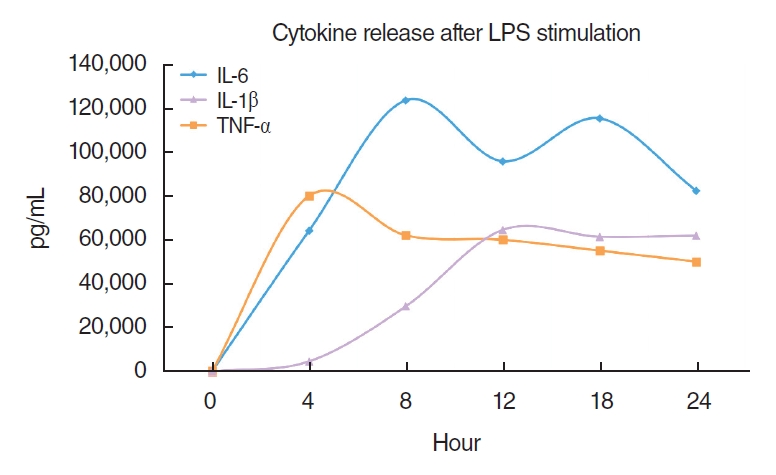
Article91. Gattorno M, Tassi S, Carta S, Delfino L, Ferlito F, Pelagatti MA, et al. Pattern of interleukin-1beta secretion in response to lipopolysaccharide and ATP before and after interleukin-1 blockade in patients with CIAS1 mutations. Arthritis Rheum. 2007; Sep. 56(9):3138–48.
Article92. Church LD, Cook GP, McDermott MF. Primer: inflammasomes and interleukin 1beta in inflammatory disorders. Nat Clin Pract Rheumatol. 2008; Jan. 4(1):34–42.93. Hashimoto S, Billings P, Harris JP, Firestein GS, Keithley EM. Innate immunity contributes to cochlear adaptive immune responses. Audiol Neurootol. 2005; Jan-Feb. 10(1):35–43.
Article94. Henderson C, Goldbach-Mansky R. Monogenic IL-1 mediated autoinflammatory and immunodeficiency syndromes: finding the right balance in response to danger signals. Clin Immunol. 2010; May. 135(2):210–22.
Article95. Mirault T, Launay D, Cuisset L, Hachulla E, Lambert M, Queyrel V, et al. Recovery from deafness in a patient with Muckle-Wells syndrome treated with anakinra. Arthritis Rheum. 2006; May. 54(5):1697–700.
Article96. Mantovani A, Bonecchi R, Martinez FO, Galliera E, Perrier P, Allavena P, et al. Tuning of innate immunity and polarized responses by decoy receptors. Int Arch Allergy Immunol. 2003; Oct. 132(2):109–15.
Article97. Vambutas A, Lesser M, Mullooly V, Pathak S, Zahtz G, Rosen L, et al. Early efficacy trial of anakinra in corticosteroid-resistant autoimmune inner ear disease. J Clin Invest. 2014; Sep. 124(9):4115–22.
Article98. Frejo L, Gallego-Martinez A, Requena T, Martin-Sanz E, Amor-Dorado JC, Soto-Varela A, et al. Proinflammatory cytokines and response to molds in mononuclear cells of patients with Meniere disease. Sci Rep. 2018; Apr. 8(1):5974.
Article99. Flook M, Frejo L, Gallego-Martinez A, Martin-Sanz E, Rossi-Izquierdo M, Amor-Dorado JC, et al. Differential proinflammatory signature in vestibular migraine and meniere disease. Front Immunol. 2019; Jun. 10:1229.
Article100. Cai T, Jen HI, Kang H, Klisch TJ, Zoghbi HY, Groves AK. Characterization of the transcriptome of nascent hair cells and identification of direct targets of the Atoh1 transcription factor. J Neurosci. 2015; Apr. 35(14):5870–83.
Article101. Honda K, Kim SH, Kelly MC, Burns JC, Constance L, Li X, et al. Molecular architecture underlying fluid absorption by the developing inner ear. Elife. 2017; Oct. 6:e26851.
Article102. Elkon R, Milon B, Morrison L, Shah M, Vijayakumar S, Racherla M, et al. RFX transcription factors are essential for hearing in mice. Nat Commun. 2015; Oct. 6:8549.
Article103. Hirano T. IL-6 in inflammation, autoimmunity and cancer. Int Immunol. 2021; Mar. 33(3):127–48.
Article104. Winkles JA. The TWEAK-Fn14 cytokine-receptor axis: discovery, biology and therapeutic targeting. Nat Rev Drug Discov. 2008; May. 7(5):411–25.
Article105. Burkly LC. Regulation of tissue responses: the TWEAK/Fn14 pathway and other TNF/TNFR superfamily members that activate non-canonical NFκB signaling. Front Immunol. 2015; Mar. 6:92.
Article106. Baxter FO, Came PJ, Abell K, Kedjouar B, Huth M, Rajewsky K, et al. IKKbeta/2 induces TWEAK and apoptosis in mammary epithelial cells. Development. 2006; Sep. 133(17):3485–94.107. Park JS, Kwok SK, Lim MA, Oh HJ, Kim EK, Jhun JY, et al. TWEAK promotes osteoclastogenesis in rheumatoid arthritis. Am J Pathol. 2013; Sep. 183(3):857–67.
Article108. Michaelson JS, Wisniacki N, Burkly LC, Putterman C. Role of TWEAK in lupus nephritis: a bench-to-bedside review. J Autoimmun. 2012; Sep. 39(3):130–42.
Article109. Serafini B, Magliozzi R, Rosicarelli B, Reynolds R, Zheng TS, Aloisi F. Expression of TWEAK and its receptor Fn14 in the multiple sclerosis brain: implications for inflammatory tissue injury. J Neuropathol Exp Neurol. 2008; Dec. 67(12):1137–48.
Article110. Stephan D, Sbai O, Wen J, Couraud PO, Putterman C, Khrestchatisky M, et al. TWEAK/Fn14 pathway modulates properties of a human microvascular endothelial cell model of blood brain barrier. J Neuroinflammation. 2013; Jan. 10:9.
Article111. Sun SC. Non-canonical NF-κB signaling pathway. Cell Res. 2011; Jan. 21(1):71–85.
Article112. Ramadass V, Vaiyapuri T, Tergaonkar V. Small molecule NF-κB pathway inhibitors in clinic. Int J Mol Sci. 2020; Jul. 21(14):5164.
Article113. Gilmore TD, Herscovitch M. Inhibitors of NF-kappaB signaling: 785 and counting. Oncogene. 2006; Oct. 25(51):6887–99.114. Ren Z, Wang L, Cui J, Huoc Z, Xue J, Cui H, et al. Resveratrol inhibits NF-kB signaling through suppression of p65 and IkappaB kinase activities. Pharmazie. 2013; Aug. 68(8):689–94.115. Crow MK, Ronnblom L. Type I interferons in host defence and inflammatory diseases. Lupus Sci Med. 2019; May. 6(1):e000336.
Article116. Tanaka T, Narazaki M, Kishimoto T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol. 2014; Sep. 6(10):a016295.
Article117. Tansey MG, Szymkowski DE. The TNF superfamily in 2009: new pathways, new indications, and new drugs. Drug Discov Today. 2009; Dec. 14(23-24):1082–8.
Article118. Lis K, Kuzawinska O, Balkowiec-Iskra E. Tumor necrosis factor inhibitors: state of knowledge. Arch Med Sci. 2014; Dec. 10(6):1175–85.119. Smolen JS, Landewe R, Breedveld FC, Buch M, Burmester G, Dougados M, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis. 2014; Mar. 73(3):492–509.120. Dinarello CA. Overview of the IL-1 family in innate inflammation and acquired immunity. Immunol Rev. 2018; Jan. 281(1):8–27.
Article121. Gabay C, Lamacchia C, Palmer G. IL-1 pathways in inflammation and human diseases. Nat Rev Rheumatol. 2010; Apr. 6(4):232–41.
Article122. Ren K, Torres R. Role of interleukin-1beta during pain and inflammation. Brain Res Rev. 2009; Apr. 60(1):57–64.123. Dhimolea E. Canakinumab. MAbs. 2010; Jan-Feb. 2(1):3–13.
Article124. Rincon M, Irvin CG. Role of IL-6 in asthma and other inflammatory pulmonary diseases. Int J Biol Sci. 2012; 8(9):1281–90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Comparison of the Magnetic Resonance Images in the Patient With Definite Meniere's Disease Before and After Endolymphatic Sac Decompression
- The History of Meniere's Disease: Until the Discovery of Endolymphatic Hydrops (1862-1938)
- Two Cases of Successful Treatment With Topiramate in Patients With Meniere's Disease With Migraine
- Prosper Meniere and Meniere's Disease
- Stellate Ganglion Block for Postoperative Recurred Meniere's Disease: A case report