J Korean Med Sci.
2022 Mar;37(10):e77. 10.3346/jkms.2022.37.e77.
Perinatal Outcomes According to Accessibility to Maternal-Fetal and Neonatal Intensive Care Units by Region in Korea
- Affiliations
-
- 1Department of Pediatrics, Ajou University School of Medicine, Suwon, Korea
- 2Department of Obstetrics & Gynecology, Konkuk University School of Medicine, Seoul, Korea
- 3Mother & Child Medical Policy Support Team, National Medical Center, Seoul, Korea
- 4Public Health Statistics and Informatization Team, National Medical Center, Seoul, Korea
- 5Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2526982
- DOI: http://doi.org/10.3346/jkms.2022.37.e77
Abstract
- Background
Herein, we aimed to evaluate the maternal mortality ratio and perinatal mortality rate for different perinatal medical care service areas (PMCSAs), which were established by considering their geographical accessibility to maternal-fetal intensive care units (MFICUs) and neonatal intensive care units (NICUs), and to compare the PMCSAs according to their accessibility to these perinatal care services.
Methods
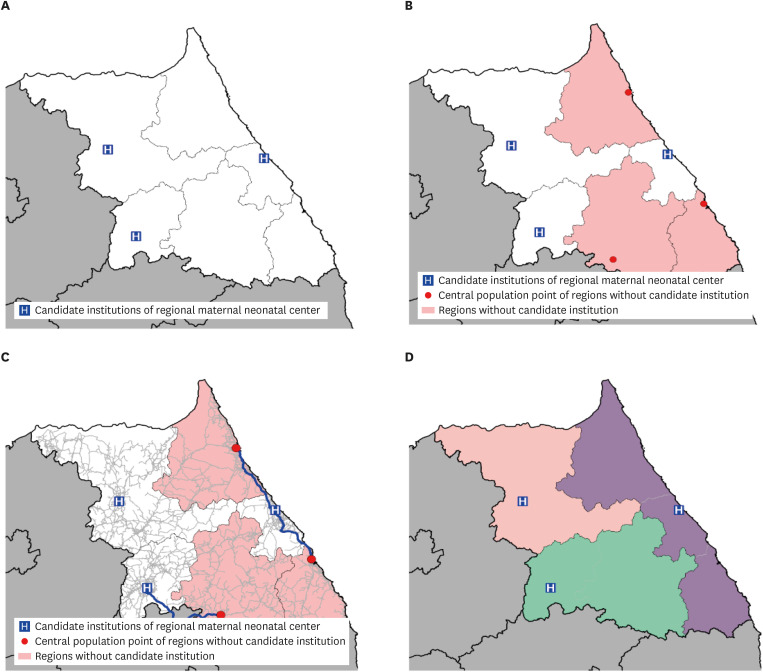
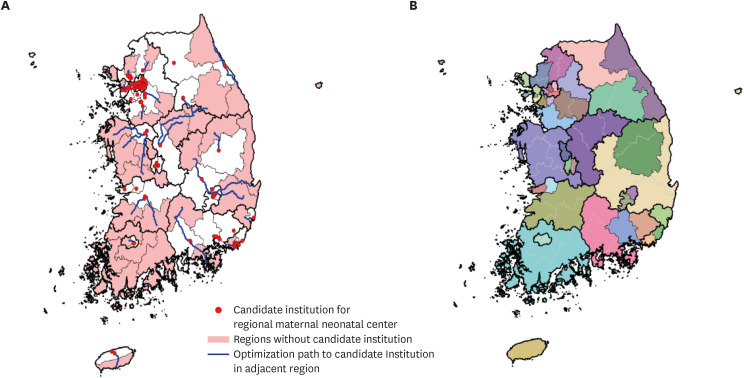
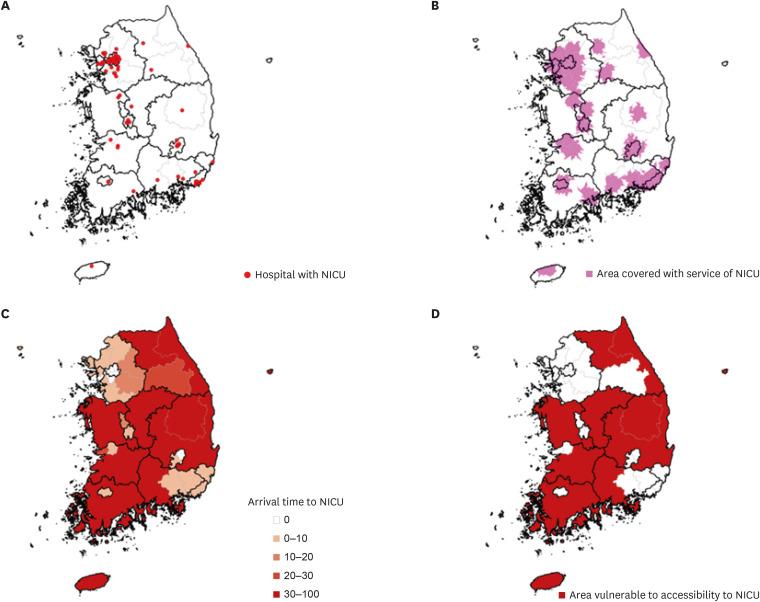
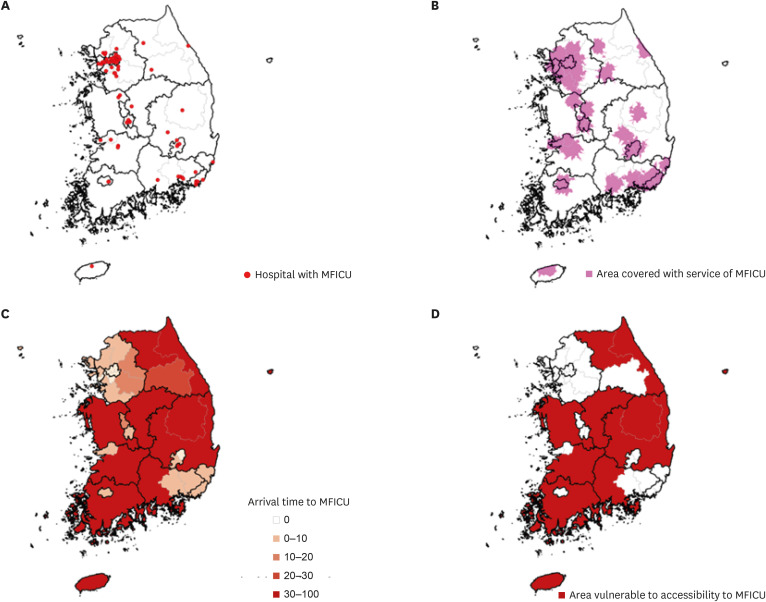
Based on the 70 hospital service areas (HSAs) across the country confirmed through the Dartmouth Atlas methodology analysis and gathering of expert opinions, the PMCSAs were designated by merging HSAs without MFICUs and NICUs to the nearest HSA that contained MFICUs and NICUs, based on which MFICU and NICU could be reached within the shortest amount of time from population-weighted centroids in HSAs. PMCSAs where 30% or more of the population could not access MFICUs and NICUs within 60 minutes were identified using the service module ArcGIS and were defined as having access vulnerability.
Results
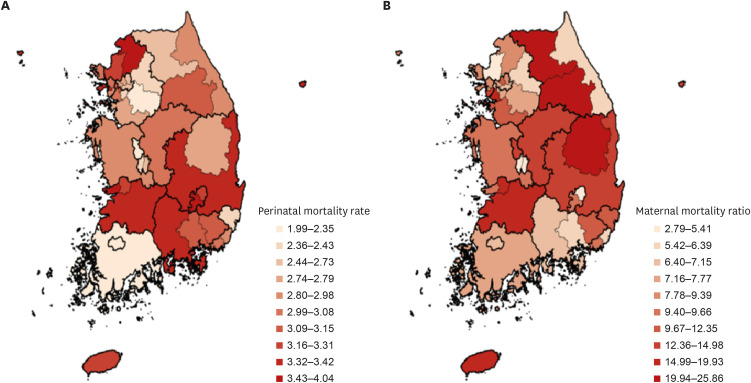
Thirty-three of 70 HSAs in the country did not contain MFICUs and NICUs, and 39 PMCSAs were finally derived by merging 70 HSAs. Ten of 39 PMCSAs (25.6%) were classified as having access vulnerability to MFICUs and NICUs. The national maternal mortality ratio was 9.42, with the highest ratio seen in the region of Wonju (25.86) and the lowest in Goyang (2.79). The national perinatal mortality rate was 2.86, with the highest and lowest rates observed in the Gunsan (4.04) and Sejong (1.99) regions, respectively. The perinatal mortality rates for areas vulnerable and invulnerable to maternal and neonatal healthcare accessibility were 2.97 and 2.92, respectively, but there was no statistically significant difference in this rate (P = 0.789). The maternal mortality ratio for areas vulnerable and invulnerable to maternal and neonatal healthcare accessibility were 14.28 and 9.48, respectively; this ratio was significantly higher in areas vulnerable to accessibility (P = 0.022).
Conclusion
Of the PMCSAs across the country, 25.6% (10/39) were deemed to be vulnerable to MFICU and NICU accessibility. There was no difference in the perinatal mortality rate between the vulnerable and invulnerable areas, but the maternal mortality ratio in vulnerable areas was significantly higher than that in invulnerable areas.
Keyword
Figure
Cited by 1 articles
-
Trends, Causes, and Solutions for Maternal Deaths in Republic of Korea
Se Jin Lee
J Korean Matern Child Health. 2024;28(4):145-149. doi: 10.21896/jkmch.2024.28.4.145.
Reference
-
1. Statistics Korea. Birth statistics in 2020. Updated 2021. Accessed September 28, 2021. http://kostat.go.kr/portal/eng/pressReleases/8/10/index.board .2. Joo S. Establishing an emergency maternal transport control center. J Korean Soc Matern Child Health. 2018; 22(1):1–6.
Article3. National Health Insurance Service, Health Insurance Review and Assessment Service. National health insurance statistical yearbook (2012–2019). Updated 2020. Accessed October 20, 2021. https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020045020000 .4. Ministry of the Interior and Safety. Resident population data (2012–2019). Updated in 2021. Accessed October 10, 2021. https://jumin.mois.go.kr/ .5. Easter SR, Robinson JN, Menard MK, Creanga AA, Xu X, Little SE, et al. Potential effects of regionalized maternity care on U.S. hospitals. Obstet Gynecol. 2019; 134(3):545–552. PMID: 31403590.
Article6. Hung P, Casey MM, Kozhimannil KB, Karaca-Mandic P, Moscovice IS. Rural-urban differences in access to hospital obstetric and neonatal care: how far is the closest one? J Perinatol. 2018; 38(6):645–652. PMID: 29453436.
Article7. Hein HA. Regionalization of perinatal health care: a lesson learned but lost. J Perinatol. 1999; 19(8 Pt 1):584–588. PMID: 10645525.
Article8. Chang YS. Past, present, and future of neonatology in Korea. J Korean Med Assoc. 2016; 59(7):487–489.
Article9. Lee JH, Noh OK, Chang YS. Korean Neonatal Network. Neonatal outcomes of very low birth weight infants in Korean Neonatal Network from 2013 to 2016. J Korean Med Sci. 2019; 34(5):e40. PMID: 30718992.
Article10. Shim JW, Kim MJ, Kim EK, Park HK, Song ES, Lee SM, et al. The impact of neonatal care resources on regional variation in neonatal mortality among very low birthweight infants in Korea. Paediatr Perinat Epidemiol. 2013; 27(2):216–225. PMID: 23374067.
Article11. Jung SY, Suh JH, Cha MI, Jung KY. Status and analysis of the accidental out-of-hospital deliveries transferred by emergency medical service providers. J Korean Soc Emerg Med. 2017; 28(3):240–247.12. Chang YS. Support Plan for the Establishment of a Regional Maternal and Neonatal Medical Care Center. 2020 Report of Division of Public Health, Ministry of Health and Welfare. Seoul, Korea: The Korean Society of Perinatology;2020.13. Health Insurance Review and Assessment Service. Provider Statistics Data. Wonju, Korea: Health Insurance Review and Assessment Service;2018.14. Kim Y. Study on the Classification of Essential Medical Care Rights and the Analysis of Medical Status. Sejong, Korea: Ministry of Health and Welfare;2019.15. Ministry of Health and Welfare. Measures to Enhance Reliable Regional Healthcare Services. Sejong, Korea: Ministry of Health and Welfare;2019.16. ESRI. Network analyst: closest facility analysis. ArcMap documentation. Updated 2020. Accessed December 23, 2020. https://desktop.arcgis.com/en/arcmap/latest/extensions/network-analyst/closest-facility.htm .17. ESRI. Network analyst: service area analysis. ArcMap documentation. Updated 2020. Accessed December 23, 2020. https://desktop.arcgis.com/en/arcmap/latest/extensions/network-analyst/service-area.htm .18. Statistics Korea. Cause of death statistics (2014–2018). Accessed December 28, 2020. https://mdis.kostat.go.kr/eng/pageLink.do?link=mdisDataService .19. Statistics Korea. Infant, maternal and perinatal mortality statistics (2018). Updated 2020. Accessed January 22, 2021. http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=2769 .20. Feltz CJ, Miller GE. An asymptotic test for the equality of coefficients of variation from k populations. Stat Med. 1996; 15(6):646–658. PMID: 8731006.21. Brace V, Kernaghan D, Penney G. Learning from adverse clinical outcomes: major obstetric haemorrhage in Scotland, 2003–05. BJOG. 2007; 114(11):1388–1396. PMID: 17949379.
Article22. Berg CJ, Harper MA, Atkinson SM, Bell EA, Brown HL, Hage ML, et al. Preventability of pregnancy-related deaths: results of a state-wide review. Obstet Gynecol. 2005; 106(6):1228–1234. PMID: 16319245.23. Wright JD, Herzog TJ, Shah M, Bonanno C, Lewin SN, Cleary K, et al. Regionalization of care for obstetric hemorrhage and its effect on maternal mortality. Obstet Gynecol. 2010; 115(6):1194–1200. PMID: 20502290.
Article24. Watkinson M, McIntosh N. Outcome of neonatal intensive care: obstetric implications for a regional service. Br J Obstet Gynaecol. 1986; 93(7):711–716. PMID: 3730341.
Article25. Siegel E, Gillings D, Campbell S, Guild P. A controlled evaluation of rural regional perinatal care: impact on mortality and morbidity. Am J Public Health. 1985; 75(3):246–253. PMID: 3976948.
Article26. Sims DG, Wynn J, Chiswick ML. Outcome for newborn babies declined admission to a regional neonatal intensive care unit. Arch Dis Child. 1982; 57(5):334–337. PMID: 7092287.
Article27. Mayfield JA, Rosenblatt RA, Baldwin LM, Chu J, Logerfo JP. The relation of obstetrical volume and nursery level to perinatal mortality. Am J Public Health. 1990; 80(7):819–823. PMID: 2356905.
Article28. McCormick MC, Shapiro S, Starfield BH. The regionalization of perinatal services. Summary of the evaluation of a national demonstration program. JAMA. 1985; 253(6):799–804. PMID: 2578581.
Article29. Chang YS. Moving forward to improve safety and quality of neonatal intensive care in Korea. J Korean Med Sci. 2018; 33(9):e89. PMID: 29441743.
Article30. Song IG, Shin SH, Kim HS. Improved regional disparities in neonatal care by government-led policies in Korea. J Korean Med Sci. 2018; 33(6):e43. PMID: 29349938.
Article31. Lee SY. Prenatal and postnatal care and its policy implications. Health Welf Policy Forum. 2016; 236:37–50.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bench-marking of Japanese Perinatal Center System for Improving Maternal and Neonatal Outcome in Korea
- Current Status and a Prospect of Neonatal Intensive Care Units in Korea
- Regionalization of neonatal care and neonatal transport system
- Meta Analysis of Elderly Gravida according to Postpartum Maternal, and Fetal and Neonatal Outcomes
- Current status of neonatal intensive care units in Korea