Ann Hepatobiliary Pancreat Surg.
2022 Feb;26(1):47-57. 10.14701/ahbps.21-080.
Is partial hepatectomy a curable treatment option for hepatocellular carcinoma accompanied by cirrhosis? A meta-analysis and cure model analysis
- Affiliations
-
- 1Department of Surgery, Catholic Kwandong University International St. Mary’s Hospital, Incheon, Korea
- KMID: 2526832
- DOI: http://doi.org/10.14701/ahbps.21-080
Abstract
- Backgrounds/Aims
It is challenging to assess the efficacy of partial hepatectomy (PH) as a treatment option for patients with hepatocellular carcinoma (HCC) accompanied by cirrhosis. This study aimed to determine the cure fraction of PH for HCC accompanied by cirrhosis compared to that for HCC without cirrhosis.
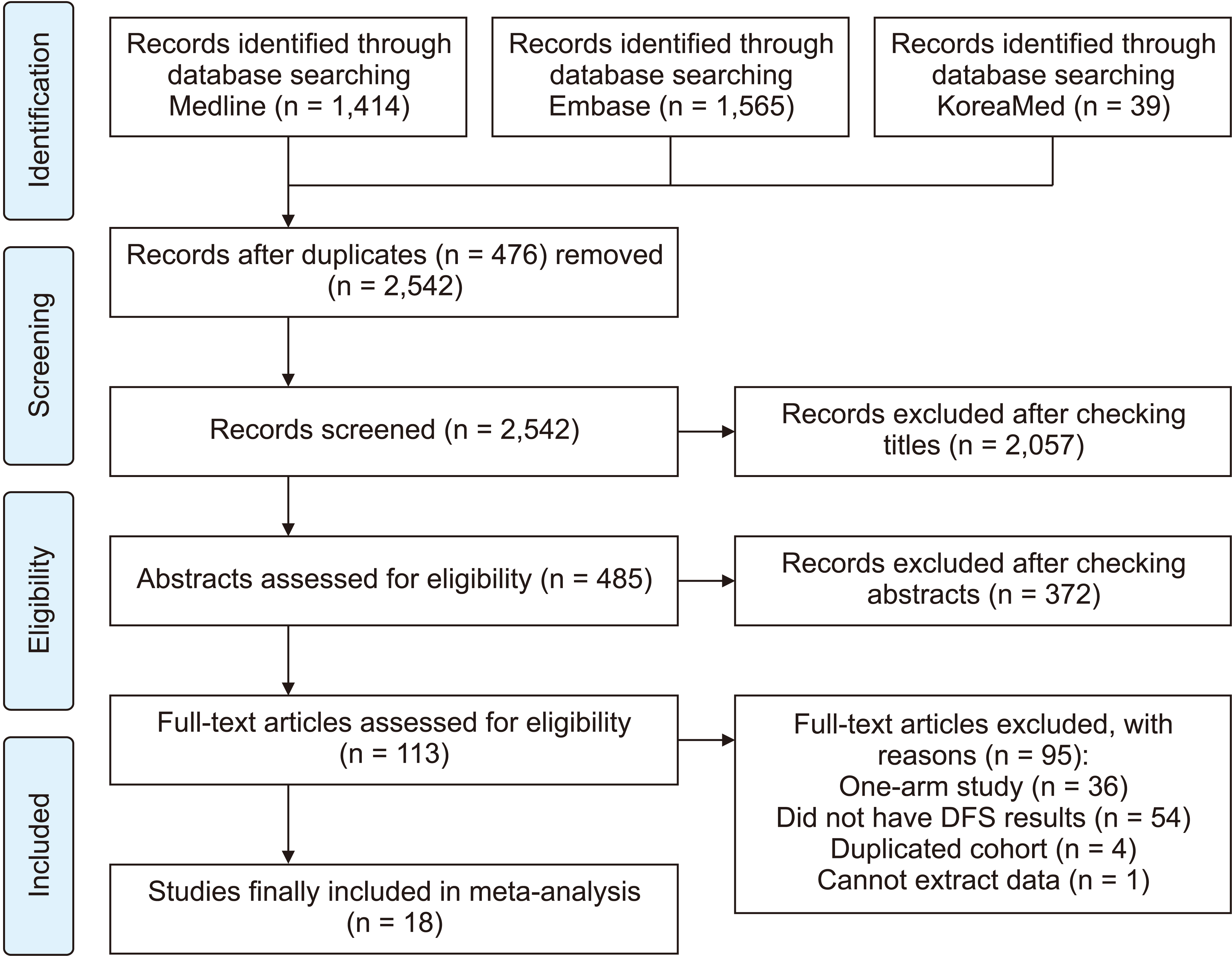
Methods
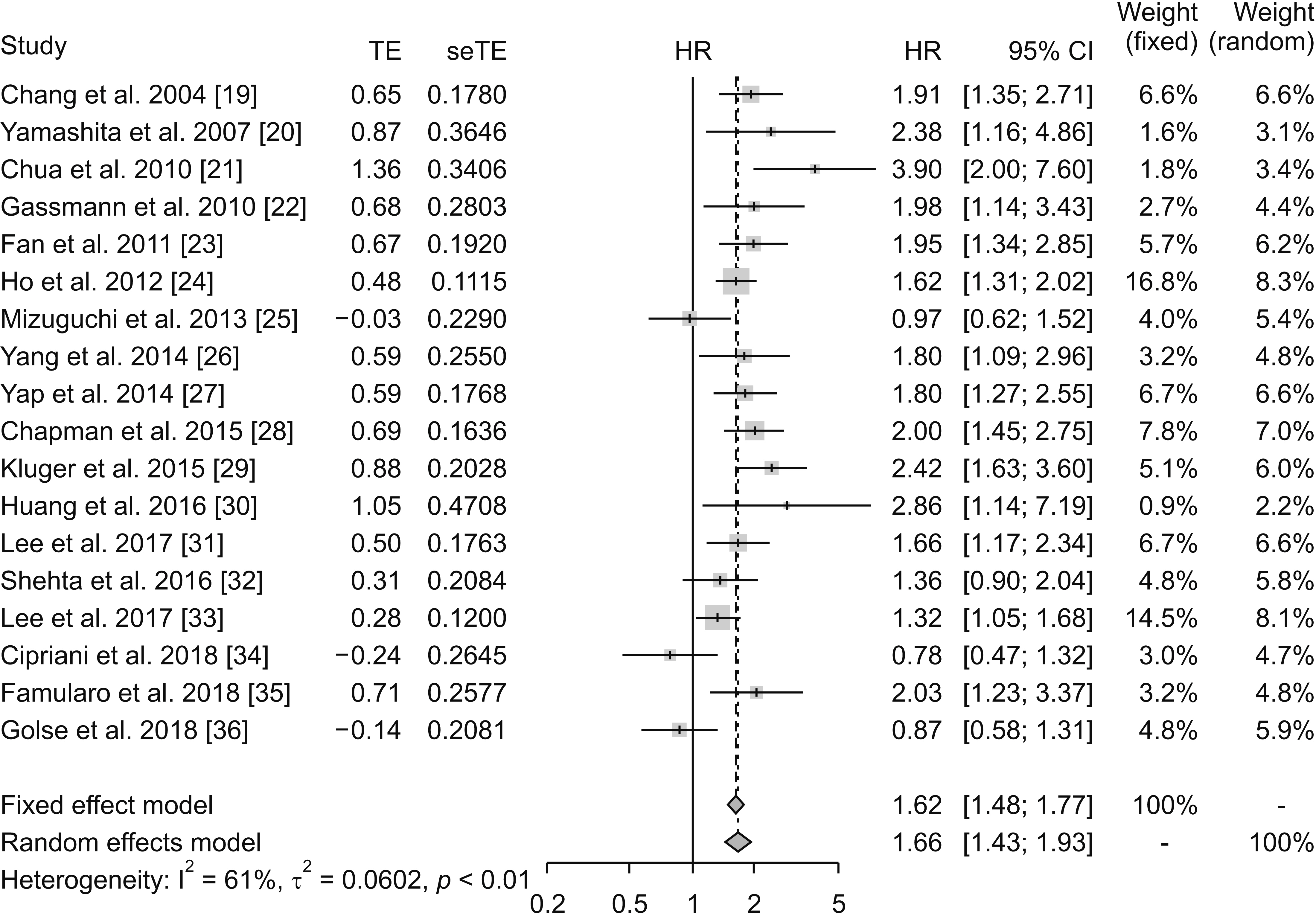
A systematic review was performed on outcomes of previous studies that compared recurrence-free survival (RFS) after PH in patients with HCC with or without cirrhosis. A meta-analysis was conducted to obtain the cumulative hazard ratio for two patient groups: cirrhosis and non-cirrhosis. Cure fractions after PH in both groups were determined using a cure model analysis.
Results
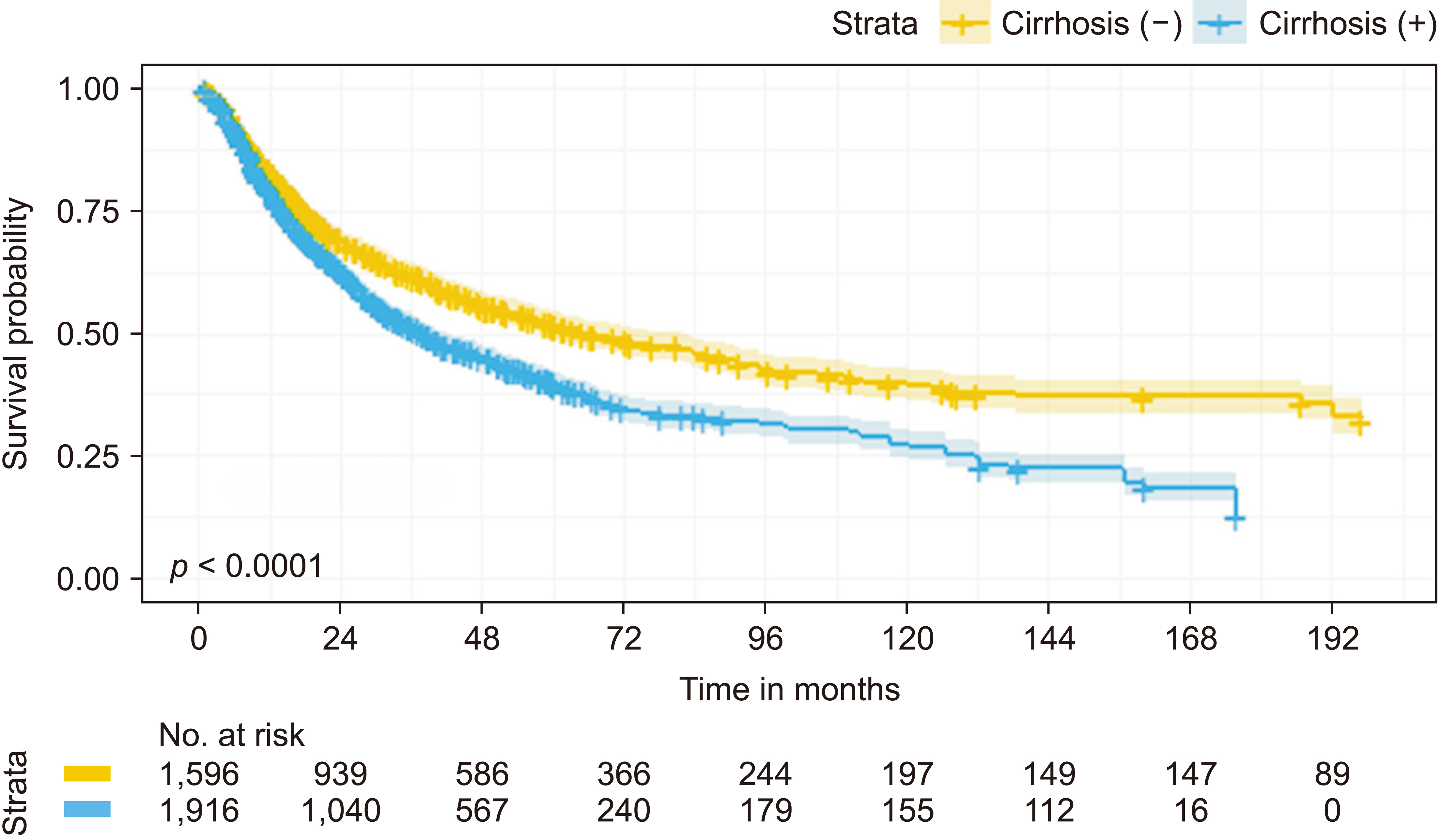
A total of 18 studies were eligible for meta-analysis and 13 studies were selected for the cure model analysis. The cumulative hazard ratio for RFS of the cirrhosis group compared to that of the non-cirrhosis group was 1.66 (95% confidence interval [CI], 1.43–1.93). Survival data of 3,512 patients in both groups were reconstructed from survival curves of original articles for cure model analysis. The probability of being statistically cured after PH for HCC was 14.1% (95% CI, 10.6%–18.1%) in the cirrhosis group lower than that (32.5%) in the non-cirrhosis group (95% CI, 28.6%–36.4%).
Conclusions
The prognosis after PH for HCC accompanied by cirrhosis is inferior to that for HCC without cirrhosis. However, a cure can be expected for one-seventh of patients with HCC accompanied by cirrhosis after PH.
Keyword
Figure
Reference
-
1. Lafaro KJ, Demirjian AN, Pawlik TM. 2015; Epidemiology of hepatocellular carcinoma. Surg Oncol Clin N Am. 24:1–17. DOI: 10.1016/j.soc.2014.09.001. PMID: 25444466.
Article2. Fujiwara N, Friedman SL, Goossens N, Hoshida Y. 2018; Risk factors and prevention of hepatocellular carcinoma in the era of precision medicine. J Hepatol. 68:526–549. DOI: 10.1016/j.jhep.2017.09.016. PMID: 28989095. PMCID: PMC5818315.
Article3. Petrick JL, Kelly SP, Altekruse SF, McGlynn KA, Rosenberg PS. 2016; Future of hepatocellular carcinoma incidence in the United States forecast through 2030. J Clin Oncol. 34:1787–1794. DOI: 10.1200/JCO.2015.64.7412. PMID: 27044939. PMCID: PMC4966339.
Article4. McGlynn KA, Petrick JL, London WT. 2015; Global epidemiology of hepatocellular carcinoma: an emphasis on demographic and regional variability. Clin Liver Dis. 19:223–238. DOI: 10.1016/j.cld.2015.01.001. PMID: 25921660. PMCID: PMC4712629.5. El-Serag HB, Siegel AB, Davila JA, Shaib YH, Cayton-Woody M, McBride R, et al. 2006; Treatment and outcomes of treating of hepatocellular carcinoma among Medicare recipients in the United States: a population-based study. J Hepatol. 44:158–166. DOI: 10.1016/j.jhep.2005.10.002. PMID: 16290309.
Article6. op den Winkel M, Nagel D, Sappl J, op den Winkel P, Lamerz R, Zech CJ, et al. 2012; Prognosis of patients with hepatocellular carcinoma. Validation and ranking of established staging-systems in a large western HCC-cohort. PLoS One. 7:e45066. DOI: 10.1371/journal.pone.0045066. PMID: 23071507. PMCID: PMC3465308.
Article7. Byam J, Renz J, Millis JM. 2013; Liver transplantation for hepatocellular carcinoma. Hepatobiliary Surg Nutr. 2:22–30. DOI: 10.3978/j.issn.2304-3881.2012.11.03. PMID: 24570911. PMCID: PMC3924634.8. Halazun KJ, Najjar M, Abdelmessih RM, Samstein B, Griesemer AD, Guarrera JV, et al. 2017; Recurrence after liver transplantation for hepatocellular carcinoma: a new MORAL to the story. Ann Surg. 265:557–564. DOI: 10.1097/SLA.0000000000001966. PMID: 27611615.9. Yao FY, Ferrell L, Bass NM, Watson JJ, Bacchetti P, Venook A, et al. 2001; Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 33:1394–1403. DOI: 10.1053/jhep.2001.24563. PMID: 11391528.
Article10. Krenzien F, Schmelzle M, Struecker B, Raschzok N, Benzing C, Jara M, et al. 2018; Liver transplantation and liver resection for cirrhotic patients with hepatocellular carcinoma: comparison of long-term survivals. J Gastrointest Surg. 22:840–848. DOI: 10.1007/s11605-018-3690-4. PMID: 29363019.
Article11. Zheng Z, Liang W, Milgrom DP, Zheng Z, Schroder PM, Kong NS, et al. 2014; Liver transplantation versus liver resection in the treatment of hepatocellular carcinoma: a meta-analysis of observational studies. Transplantation. 97:227–234. DOI: 10.1097/TP.0b013e3182a89383. PMID: 24142034.
Article12. Pinna AD, Yang T, Mazzaferro V, De Carlis L, Zhou J, Roayaie S, et al. 2018; Liver transplantation and hepatic resection can achieve cure for hepatocellular carcinoma. Ann Surg. 268:868–875. DOI: 10.1097/SLA.0000000000002889. PMID: 30080736.
Article13. Tsilimigras DI, Bagante F, Moris D, Merath K, Paredes AZ, Sahara K, et al. 2019; Defining the chance of cure after resection for hepatocellular carcinoma within and beyond the Barcelona Clinic Liver Cancer guidelines: a multi-institutional analysis of 1,010 patients. Surgery. 166:967–974. DOI: 10.1016/j.surg.2019.08.010. PMID: 31606196.
Article14. Lambert PC, Thompson JR, Weston CL, Dickman PW. 2007; Estimating and modeling the cure fraction in population-based cancer survival analysis. Biostatistics. 8:576–594. DOI: 10.1093/biostatistics/kxl030. PMID: 17021277.
Article15. Othus M, Barlogie B, Leblanc ML, Crowley JJ. 2012; Cure models as a useful statistical tool for analyzing survival. Clin Cancer Res. 18:3731–3736. DOI: 10.1158/1078-0432.CCR-11-2859. PMID: 22675175. PMCID: PMC3744099.
Article16. Guyot P, Ades AE, Ouwens MJ, Welton NJ. 2012; Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol. 12:9. DOI: 10.1186/1471-2288-12-9. PMID: 22297116. PMCID: PMC3313891.
Article17. R Development Core Team. R: a language and environment for statistical computing [Internet]. Available from: https://www.R-project.org/. Vienna: R Foundation for Statistical Computing;2017. cited 2020 Dec 1.18. Higgins JP, Thompson SG, Deeks JJ, Altman DG. 2003; Measuring inconsistency in meta-analyses. BMJ. 327:557–560. DOI: 10.1136/bmj.327.7414.557. PMID: 12958120. PMCID: PMC192859.
Article19. Chang CH, Chau GY, Lui WY, Tsay SH, King KL, Wu CW. 2004; Long-term results of hepatic resection for hepatocellular carcinoma originating from the noncirrhotic liver. Arch Surg. 139:320–325. DOI: 10.1001/archsurg.139.3.320. PMID: 15006892.
Article20. Yamashita Y, Taketomi A, Itoh S, Kitagawa D, Kayashima H, Harimoto N, et al. 2007; Longterm favorable results of limited hepatic resections for patients with hepatocellular carcinoma: 20 years of experience. J Am Coll Surg. 205:19–26. DOI: 10.1016/j.jamcollsurg.2007.01.069. PMID: 17617328.
Article21. Chua TC, Saxena A, Chu F, Liauw W, Zhao J, Morris DL. 2010; Clinicopathological determinants of survival after hepatic resection of hepatocellular carcinoma in 97 patients--experience from an Australian hepatobiliary unit. J Gastrointest Surg. 14:1370–1380. DOI: 10.1007/s11605-010-1277-9. PMID: 20585991.
Article22. Gassmann P, Spieker T, Haier J, Schmidt F, Mardin WA, Senninger N. 2010; Prognostic impact of underlying liver fibrosis and cirrhosis after curative resection of hepatocellular carcinoma. World J Surg. 34:2442–2451. DOI: 10.1007/s00268-010-0655-5. PMID: 20544346.
Article23. Fan ST, Poon RT, Yeung C, Lam CM, Lo CM, Yuen WK, et al. 2011; Outcome after partial hepatectomy for hepatocellular cancer within the Milan criteria. Br J Surg. 98:1292–1300. DOI: 10.1002/bjs.7583. PMID: 21656513.
Article24. Ho CM, Lee PH, Chen CL, Ho MC, Wu YM, Hu RH. 2012; Long-term outcomes after resection versus transplantation for hepatocellular carcinoma within UCSF criteria. Ann Surg Oncol. 19:826–833. DOI: 10.1245/s10434-011-1975-x. PMID: 21879276.
Article25. Mizuguchi T, Kawamoto M, Meguro M, Nakamura Y, Ota S, Hui TT, et al. 2013; Prognosis and predictors of surgical complications in hepatocellular carcinoma patients with or without cirrhosis after hepatectomy. World J Surg. 37:1379–1387. DOI: 10.1007/s00268-013-1989-6. PMID: 23479099.
Article26. Yang LY, Chang RM, Lau WY, Ou DP, Wu W, Zeng ZJ. 2014; Mesohepatectomy for centrally located large hepatocellular carcinoma: indications, techniques, and outcomes. Surgery. 156:1177–1187. DOI: 10.1016/j.surg.2014.05.012. PMID: 25444316.
Article27. Yap AQ, Millan CA, Wang JH, Wang CC, Lu SN, Wang SH, et al. 2014; How to improve the outcome in patients with AJCC stage I hepatocellular carcinoma. Anticancer Res. 34:3093–3103. PMID: 24922678.28. Chapman WC, Klintmalm G, Hemming A, Vachharajani N, Majella Doyle MB, DeMatteo R, et al. 2015; Surgical treatment of hepatocellular carcinoma in North America: can hepatic resection still be justified? J Am Coll Surg. 220:628–637. DOI: 10.1016/j.jamcollsurg.2014.12.030. PMID: 25728142.
Article29. Kluger MD, Salceda JA, Laurent A, Tayar C, Duvoux C, Decaens T, et al. 2015; Liver resection for hepatocellular carcinoma in 313 Western patients: tumor biology and underlying liver rather than tumor size drive prognosis. J Hepatol. 62:1131–1140. DOI: 10.1016/j.jhep.2014.12.018. PMID: 25529622.
Article30. Huang ZY, Liang BY, Xiong M, Dong KS, Zhang ZY, Zhang EL, et al. 2016; Severity of cirrhosis should determine the operative modality for patients with early hepatocellular carcinoma and compensated liver function. Surgery. 159:621–631. DOI: 10.1016/j.surg.2015.09.002. PMID: 26453137.
Article31. Lee HW, Choi GH, Kim DY, Park YN, Kim KS, Choi JS, et al. 2017; Less fibrotic burden differently affects the long-term outcomes of hepatocellular carcinoma after curative resection. Oncology. 93:224–232. DOI: 10.1159/000477173. PMID: 28571030.
Article32. Shehta A, Han HS, Yoon YS, Cho JY, Choi Y. 2016; Laparoscopic liver resection for hepatocellular carcinoma in cirrhotic patients: 10-year single-center experience. Surg Endosc. 30:638–648. DOI: 10.1007/s00464-015-4253-3. PMID: 26091992.
Article33. Lee EC, Kim SH, Park H, Lee SD, Lee SA, Park SJ. 2017; Survival analysis after liver resection for hepatocellular carcinoma: a consecutive cohort of 1002 patients. J Gastroenterol Hepatol. 32:1055–1063. DOI: 10.1111/jgh.13632. PMID: 27797420.
Article34. Cipriani F, Fantini C, Ratti F, Lauro R, Tranchart H, Halls M, et al. 2018; Laparoscopic liver resections for hepatocellular carcinoma. Can we extend the surgical indication in cirrhotic patients? Surg Endosc. 32:617–626. DOI: 10.1007/s00464-017-5711-x. PMID: 28717870.
Article35. Famularo S, Di Sandro S, Giani A, Lauterio A, Sandini M, De Carlis R, et al. 2018; Long-term oncologic results of anatomic vs. parenchyma-sparing resection for hepatocellular carcinoma. A propensity score-matching analysis. Eur J Surg Oncol. 44:1580–1587. DOI: 10.1016/j.ejso.2018.05.018. PMID: 29861336.
Article36. Golse N, El Bouyousfi A, Marques F, Bancel B, Mohkam K, Ducerf C, et al. 2018; Large hepatocellular carcinoma: does fibrosis really impact prognosis after resection? J Visc Surg. 155:265–273. DOI: 10.1016/j.jviscsurg.2017.10.015. PMID: 29525540.
Article37. Akcam AT, Saritas AG, Ulku A, Rencuzogullari A. 2019; Oncological outcomes of hepatic resection vs transplantation for localized hepatocellular carcinoma. Transplant Proc. 51:1147–1152. DOI: 10.1016/j.transproceed.2019.01.093. PMID: 31101189.
Article38. Xu XF, Xing H, Han J, Li ZL, Lau WY, Zhou YH, et al. 2019; Risk factors, patterns, and outcomes of late recurrence after liver resection for hepatocellular carcinoma: a multicenter study from China. JAMA Surg. 154:209–217. DOI: 10.1001/jamasurg.2018.4334. PMID: 30422241. PMCID: PMC6439634.
Article39. Li ZL, Yu JJ, Guo JW, Sui CJ, Dai BH, Zhang WG, et al. 2019; Liver resection is justified for multinodular hepatocellular carcinoma in selected patients with cirrhosis: a multicenter analysis of 1,066 patients. Eur J Surg Oncol. 45:800–807. DOI: 10.1016/j.ejso.2018.12.016. PMID: 30594407.
Article40. Affo S, Yu LX, Schwabe RF. 2017; The role of cancer-associated fibroblasts and fibrosis in liver cancer. Annu Rev Pathol. 12:153–186. DOI: 10.1146/annurev-pathol-052016-100322. PMID: 27959632. PMCID: PMC5720358.
Article41. Fattovich G, Stroffolini T, Zagni I, Donato F. 2004; Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology. 127(5 Suppl 1):S35–S50. DOI: 10.1053/j.gastro.2004.09.014. PMID: 15508101.
Article42. Ju MJ, Qiu SJ, Fan J, Xiao YS, Gao Q, Zhou J, et al. 2009; Peritumoral activated hepatic stellate cells predict poor clinical outcome in hepatocellular carcinoma after curative resection. Am J Clin Pathol. 131:498–510. DOI: 10.1309/AJCP86PPBNGOHNNL. PMID: 19289585.
Article43. Yu DC, Liu J, Chen J, Shao JJ, Shen X, Xia HG, et al. 2014; GGPPS1 predicts the biological character of hepatocellular carcinoma in patients with cirrhosis. BMC Cancer. 14:248. DOI: 10.1186/1471-2407-14-248. PMID: 24716791. PMCID: PMC4028285.
Article44. Lin Y, Liang R, Ye J, Li Q, Liu Z, Gao X, et al. 2019; A twenty gene-based gene set variation score reflects the pathological progression from cirrhosis to hepatocellular carcinoma. Aging (Albany NY). 11:11157–11169. DOI: 10.18632/aging.102518. PMID: 31811111. PMCID: PMC6932912.
Article45. Harimoto N, Yoshizumi T, Fujimoto Y, Motomura T, Mano Y, Toshima T, et al. 2018; Surgery for hepatocellular carcinoma in patients with Child-Pugh B cirrhosis: hepatic resection versus living donor liver transplantation. World J Surg. 42:2606–2616. DOI: 10.1007/s00268-018-4493-1. PMID: 29372372.
Article46. Margarit C, Escartín A, Castells L, Vargas V, Allende E, Bilbao I. 2005; Resection for hepatocellular carcinoma is a good option in Child-Turcotte-Pugh class A patients with cirrhosis who are eligible for liver transplantation. Liver Transpl. 11:1242–1251. DOI: 10.1002/lt.20398. PMID: 16184539.
Article47. Madkhali AA, Fadel ZT, Aljiffry MM, Hassanain MM. 2015; Surgical treatment for hepatocellular carcinoma. Saudi J Gastroenterol. 21:11–17. DOI: 10.4103/1319-3767.151216. PMID: 25672233. PMCID: PMC4355856.
Article48. Kulik L, Heimbach JK, Zaiem F, Almasri J, Prokop LJ, Wang Z, et al. 2018; Therapies for patients with hepatocellular carcinoma awaiting liver transplantation: a systematic review and meta-analysis. Hepatology. 67:381–400. DOI: 10.1002/hep.29485. PMID: 28859222.
Article49. Chedid MF, Kruel CRP, Pinto MA, Grezzana-Filho TJM, Leipnitz I, Kruel CDP, et al. 2017; Hepatocellular carcinoma: diagnosis and operative management. Arq Bras Cir Dig. 30:272–278. DOI: 10.1590/0102-6720201700040011. PMID: 29340553. PMCID: PMC5793147.
Article50. Jadlowiec CC, Taner T. 2016; Liver transplantation: current status and challenges. World J Gastroenterol. 22:4438–4445. DOI: 10.3748/wjg.v22.i18.4438. PMID: 27182155. PMCID: PMC4858627.
Article51. Chan DL, Alzahrani NA, Morris DL, Chua TC. 2014; Systematic review of efficacy and outcomes of salvage liver transplantation after primary hepatic resection for hepatocellular carcinoma. J Gastroenterol Hepatol. 29:31–41. DOI: 10.1111/jgh.12399. PMID: 24117517.
Article52. Muaddi H, Al-Adra DP, Beecroft R, Ghanekar A, Moulton CA, Doyle A, et al. 2018; Liver transplantation is equally effective as a salvage therapy for patients with hepatocellular carcinoma recurrence following radiofrequency ablation or liver resection with curative intent. Ann Surg Oncol. 25:991–999. DOI: 10.1245/s10434-017-6329-x. PMID: 29327179.
Article53. Qu W, Zhu ZJ, Sun LY, Wei L, Liu Y, Zeng ZG. 2015; Salvage liver transplantation for hepatocellular carcinoma recurrence after primary liver resection. Clin Res Hepatol Gastroenterol. 39:93–97. DOI: 10.1016/j.clinre.2014.07.006. PMID: 25150375.
Article54. Zheng S, Xie Q, Cheng J. 2018; Salvage liver transplant for hepatocellular carcinoma: rescues and benefits. Transl Gastroenterol Hepatol. 3:65. DOI: 10.21037/tgh.2018.09.06. PMID: 30363838. PMCID: PMC6182042.
Article55. Lacaze L, Scotté M. 2015; Surgical treatment of intra hepatic recurrence of hepatocellular carcinoma. World J Hepatol. 7:1755–1760. DOI: 10.4254/wjh.v7.i13.1755. PMID: 26167248. PMCID: PMC4491904.
Article56. Chan AC, Chan SC, Chok KS, Cheung TT, Chiu DW, Poon RT, et al. 2013; Treatment strategy for recurrent hepatocellular carcinoma: salvage transplantation, repeated resection, or radiofrequency ablation? Liver Transpl. 19:411–419. DOI: 10.1002/lt.23605. PMID: 23447460.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Associating microwave ablation and portal vein ligation for staged hepatectomy for the treatment of huge hepatocellular carcinoma with cirrhosis
- Prognostic Factors and Clinicopathologic Features after Resection of Small Hepatocellular Carcinoma (< or =2 cm)
- Outcome after Partial Hepatectomy for Hepatocellular Carcinoma Combined with Liver Cirrhosis
- Comparing efficacies of different treatment regimens in patients with hepatocellular carcinoma accompanied by portal vein tumor thrombus using network meta-analysis
- Survival rate of hepatectomy according to liver cirrhosis in hepatoculluar carcinoma