Korean J Gastroenterol.
2022 Feb;79(2):61-65. 10.4166/kjg.2022.017.
Chicago Classification ver. 4.0: Diagnosis of Achalasia and Esophagogastric Junction Outflow Obstruction
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2526785
- DOI: http://doi.org/10.4166/kjg.2022.017
Abstract
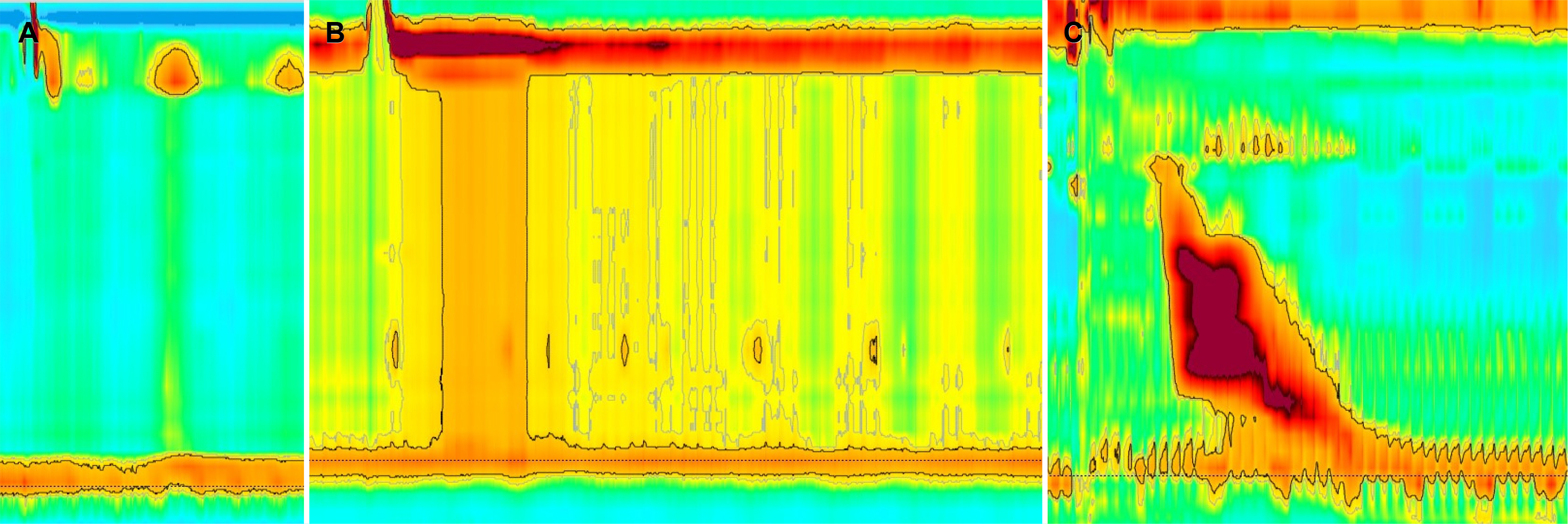
- Achalasia is a common esophageal motility disorder characterized by inappropriate relaxation of the lower esophageal sphincter and a loss of normal peristalsis in the esophageal body. The newly suggested Chicago Classification ver. 4.0 recommends conclusive diagnoses of types 1, 2, and 3. A conclusive diagnosis of type 3 achalasia requires no appreciable peristalsis compared to the previously used ver. 3.0. In the case of inconclusive diagnosis of achalasia, additional tests, including timed barium esophagogram (TBE) or functional lumen imaging probe (FLIP), are strongly recommended in ver. 4.0. Esophagogastric junction outflow obstruction (EGJOO) in Chicago Classification ver. 3.0 was defined as an elevated median integrated relaxation pressure (IRP) without evidence of achalasia. On the other hand, the diagnosis of EGJOO in Chicago Classification ver. 4.0 requires elevated IRP in both positions, elevated intrabolus pressure, positive clinical symptoms, and additional positive test by TBE or FLIP. The newly suggested Chicago Classification Classification ver. 4.0 will be helpful in an accurate diagnosis of esophageal motility disorders, including achalasia and EGJOO.
Keyword
Figure
Reference
-
1. Clouse RE, Staiano A, Alrakawi A, Haroian L. 2000; Application of topographical methods to clinical esophageal manometry. Am J Gastroenterol. 95:2720–2730. DOI: 10.1111/j.1572-0241.2000.03178.x. PMID: 11051340.
Article2. Pandolfino JE, Ghosh SK, Rice J, Clarke JO, Kwiatek MA, Kahrilas PJ. 2008; Classifying esophageal motility by pressure topography characteristics: a study of 400 patients and 75 controls. Am J Gastroenterol. 103:27–37. DOI: 10.1111/j.1572-0241.2007.01532.x. PMID: 17900331.
Article3. Kahrilas PJ, Bredenoord AJ, Fox M, et al. 2015; The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 27:160–174. DOI: 10.1111/nmo.12477. PMID: 25469569. PMCID: PMC4308501.
Article4. Yadlapati R, Kahrilas PJ, Fox MR, et al. 2021; Esophageal motility disorders on high-resolution manometry: Chicago Classification version 4.0©. Neurogastroenterol Motil. 33:e14058. DOI: 10.1111/nmo.14058. PMID: 33373111. PMCID: PMC8034247.5. Fox MR, Bredenoord AJ. 2008; Oesophageal high-resolution manometry: moving from research into clinical practice. Gut. 57:405–423. DOI: 10.1136/gut.2007.127993. PMID: 17895358.
Article6. Pandolfino JE, Gawron AJ. 2015; Achalasia: a systematic review. JAMA. 313:1841–1852. DOI: 10.1001/jama.2015.2996. PMID: 25965233.7. Ghosh SK, Pandolfino JE, Rice J, Clarke JO, Kwiatek M, Kahrilas PJ. 2007; Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol. 293:G878–G885. DOI: 10.1152/ajpgi.00252.2007. PMID: 17690172.
Article8. Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. 2008; Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 135:1526–1533. DOI: 10.1053/j.gastro.2008.07.022. PMID: 18722376. PMCID: PMC2894987.
Article9. Jung HK, Hong SJ, Lee OY, et al. 2020; 2019 Seoul consensus on esophageal achalasia guidelines. J Neurogastroenterol Motil. 26:180–203. DOI: 10.5056/jnm20014. PMID: 32235027. PMCID: PMC7176504.
Article10. Khan A, Yadlapati R, Gonlachanvit S, et al. 2021; Chicago Classification update (version 4.0): technical review on diagnostic criteria for achalasia. Neurogastroenterol Motil. 33:e14182. DOI: 10.1111/nmo.14182. PMID: 34190376.
Article11. Yadlapati R, Pandolfino JE, Fox MR, Bredenoord AJ, Kahrilas PJ. 2021; What is new in Chicago Classification version 4.0? Neurogastroenterol Motil. 33:e14053. DOI: 10.1111/nmo.14053. PMID: 33340190. PMCID: PMC8098672.
Article12. Bredenoord AJ, Babaei A, Carlson D, et al. 2021; Esophagogastric junction outflow obstruction. Neurogastroenterol Motil. 33:e14193. DOI: 10.1111/nmo.14193. PMID: 34120375. PMCID: PMC8748852.
Article13. Blonski W, Kumar A, Feldman J, Richter JE. 2018; Timed barium swallow: diagnostic role and predictive value in untreated achalasia, esophagogastric junction outflow obstruction, and non-achalasia dysphagia. Am J Gastroenterol. 113:196–203. DOI: 10.1038/ajg.2017.370. PMID: 29257145.
Article14. Savarino E, di Pietro M, Bredenoord AJ, et al. 2020; Use of the functional lumen imaging probe in clinical esophagology. Am J Gastroenterol. 115:1786–1796. DOI: 10.14309/ajg.0000000000000773. PMID: 33156096.
Article15. Roman S, Hebbard G, Jung KW, et al. 2021; Chicago Classification update (v4.0): technical review on diagnostic criteria for distal esophageal spasm. Neurogastroenterol Motil. 33:e14119. DOI: 10.1111/nmo.14119. PMID: 33666299.
Article16. Ratuapli SK, Crowell MD, DiBaise JK, et al. 2015; Opioid-induced esophageal dysfunction (OIED) in patients on chronic opioids. Am J Gastroenterol. 110:979–984. DOI: 10.1038/ajg.2015.154. PMID: 26032150.
Article17. Sweis R, Anggiansah A, Wong T, Kaufman E, Obrecht S, Fox M. 2011; Normative values and inter-observer agreement for liquid and solid bolus swallows in upright and supine positions as assessed by esophageal high-resolution manometry. Neurogastroenterol Motil. 23:509–e198. DOI: 10.1111/j.1365-2982.2011.01682.x. PMID: 21342362.
Article18. Triggs JR, Carlson DA, Beveridge C, et al. 2019; Upright integrated relaxation pressure facilitates characterization of esophagogastric junction outflow obstruction. Clin Gastroenterol Hepatol. 17:2218–2226.e2. DOI: 10.1016/j.cgh.2019.01.024. PMID: 30708108. PMCID: PMC6663640.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Approach for Esophagogastric Junction Outflow Obstruction
- Understanding the Chicago Classification: From Tracings to Patients
- Additional Diagnostic Yield of the Rapid Drink Challenge in Chicago Classification Version 4.0 Compared With Version 3.0
- Chicago Classification ver. 4.0: An Overview of Esophageal Motility Disorders on High-resolution Manometry
- Esophagogastric Junction Outflow Obstruction Transformed to Type II Achalasia