Neurointervention.
2022 Mar;17(1):54-57. 10.5469/neuroint.2021.00458.
Subsequent Subarachnoid Hemorrhage from Clinically Unrelated Vertebral Artery Dissection after Thrombolytic Therapy
- Affiliations
-
- 1Department of Neurology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 2Department of Neurology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea
- KMID: 2526627
- DOI: http://doi.org/10.5469/neuroint.2021.00458
Abstract
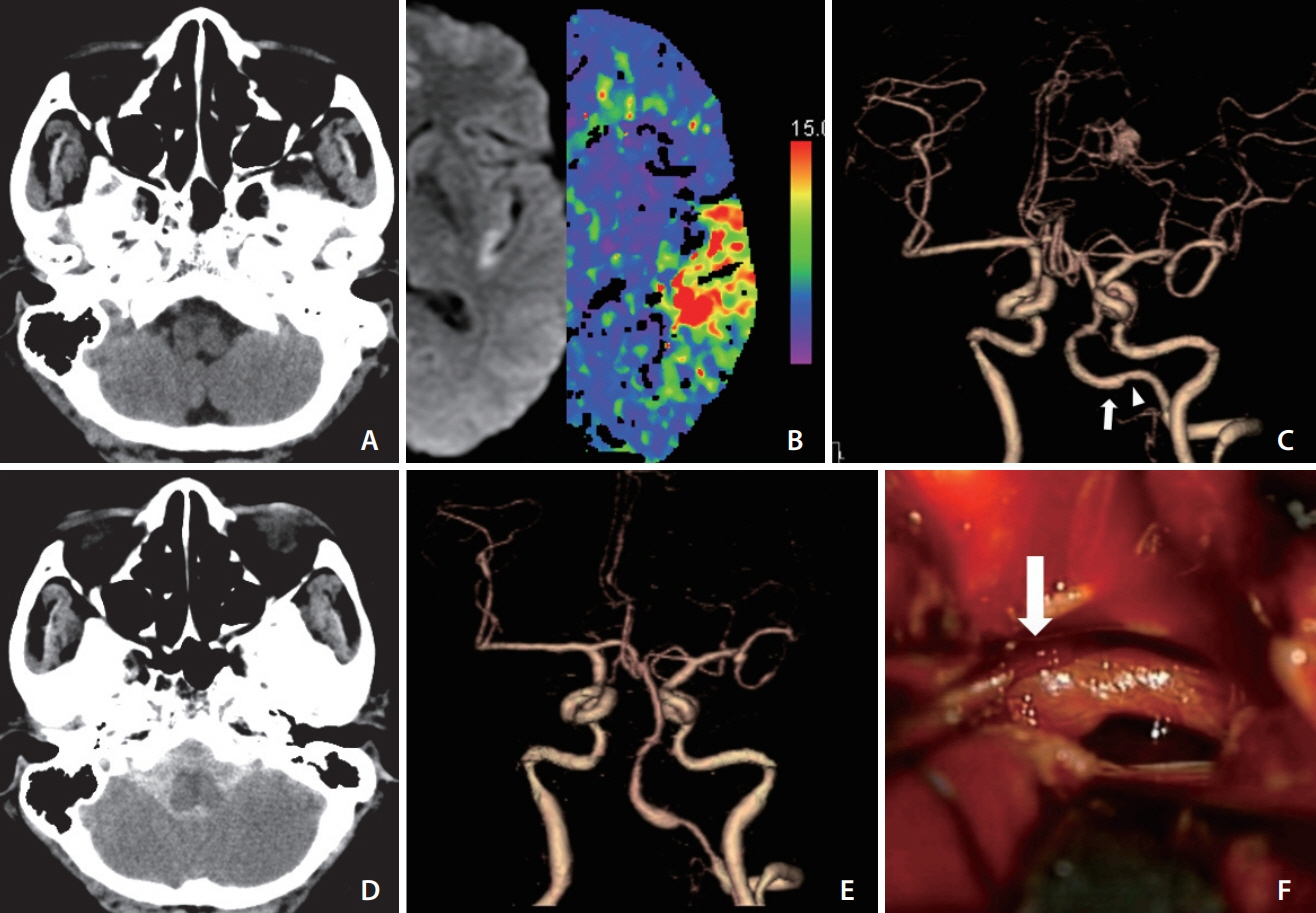
- Thrombolysis administration poses certain safety issues in ischemic stroke patients with cerebrovascular changes that are vulnerable to hemorrhage. Furthermore, the lack of related studies has resulted in an unclear understanding of thrombolysis safety in ischemic stroke patients with intracranial dissection, including those involving the vertebral artery. This study describes a case of a 59-year-old female who developed subarachnoid hemorrhage from clinically unrelated vertebral artery dissection after thrombolysis. Histories of severe headache with posterior fossa involvement in patients receiving thrombolytic therapy may indicate careful assessment for intracranial vertebral artery dissection, even if the clinical picture of the patient suggests another arterial syndrome.
Figure
Reference
-
1. Goyal N, Tsivgoulis G, Zand R, Sharma VK, Barlinn K, Male S, et al. Systemic thrombolysis in acute ischemic stroke patients with unruptured intracranial aneurysms. Neurology. 2015; 85:1452–1458.
Article2. Lin J, Sun Y, Zhao S, Xu J, Zhao C. Safety and efficacy of thrombolysis in cervical artery dissection-related ischemic stroke: a meta-analysis of observational studies. Cerebrovasc Dis. 2016; 42:272–279.
Article3. Moon Y, Lee JH, Cho HJ, Roh HG, Choi JW, Chun YI, et al. Intravenous thrombolysis in a patient with acute ischemic stroke attributable to intracranial dissection. Neurologist. 2012; 18:136–138.
Article4. Yoshioka K, Mori T. Clinical and radiological difficulties to detect isolated MCA dissection before intravenous tPA therapy. J Stroke Cerebrovasc Dis. 2019; 28:104365.
Article5. Bernardo F, Nannoni S, Strambo D, Bartolini B, Michel P, Sirimarco G. Intravenous thrombolysis in acute ischemic stroke due to intracranial artery dissection: a single-center case series and a review of literature. J Thromb Thrombolysis. 2019; 48:679–684.
Article6. Ma H, Campbell BCV, Parsons MW, Churilov L, Levi CR, Hsu C, EXTEND Investigators, et al. Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke. N Engl J Med. 2019; 380:1795–1803.
Article7. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, American Heart Association Stroke Council, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46–e110. Erratum in: Stroke 2018;49:e138, 2018;49:e233-e234.
Article8. von Babo M, De Marchis GM, Sarikaya H, Stapf C, Buffon F, Fischer U, et al. Differences and similarities between spontaneous dissections of the internal carotid artery and the vertebral artery. Stroke. 2013; 44:1537–1542.
Article9. Shin JH, Suh DC, Choi CG, Leei HK. Vertebral artery dissection: spectrum of imaging findings with emphasis on angiography and correlation with clinical presentation. Radiographics. 2000; 20:1687–1696.
Article10. Park KW, Park JS, Hwang SC, Im SB, Shin WH, Kim BT. Vertebral artery dissection: natural history, clinical features and therapeutic considerations. J Korean Neurosurg Soc. 2008; 44:109–115.
Article11. Zinkstok SM, Vergouwen MD, Engelter ST, Lyrer PA, Bonati LH, Arnold M, et al. Safety and functional outcome of thrombolysis in dissection-related ischemic stroke: a meta-analysis of individual patient data. Stroke. 2011; 42:2515–2520.
Article12. Harriott AM, Karakaya F, Ayata C. Headache after ischemic stroke: a systematic review and meta-analysis. Neurology. 2020; 94:e75–e86.13. Chaudhry SA, Kwon SY, Kneale H, Al Jajeh A, Hussain S, Razak A. Post-IV thrombolytic headache and hemorrhagic transformation risk in acute ischemic stroke. Neurol Clin Pract. 2016; 6:22–28.
Article14. James B, Chang AD, McTaggart RA, Hemendinger M, Mac Grory B, Cutting SM, et al. Predictors of symptomatic intracranial haemorrhage in patients with an ischaemic stroke with neurological deterioration after intravenous thrombolysis. J Neurol Neurosurg Psychiatry. 2018; 89:866–869.
Article15. Kim JG, Choi JY, Kim SU, Jung JM, Kwon DY, Park MH, et al. Headache characteristics of uncomplicated intracranial vertebral artery dissection and validation of ICHD-3 beta diagnostic criteria for headache attributed to intracranial artery dissection. Cephalalgia. 2015; 35:516–526.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Experiences of Unruptured Vertebral Artery Dissection
- Two Cases of Intracranial Vertebral Artery Dissecting Aneurysm Improved by Antiplatelets Therapy
- Inconspicuous longitudinal tears of the intracranial vertebral artery in traumatic basal subarachnoid hemorrhage
- Diagnosis and Management of the Spontaneous Intracranial Vertebral Artery Dissection
- Dissecting Aneurysm of Intracranial Vertebral Artery: Report of Two Autopsy Cases