J Pathol Transl Med.
2020 Mar;54(2):179-183. 10.4132/jptm.2019.10.15.
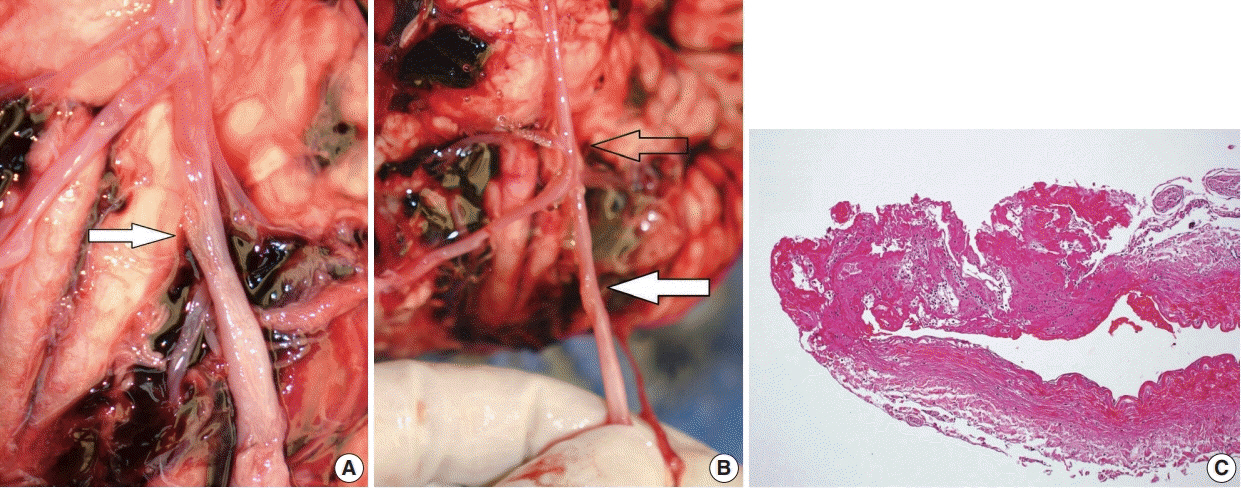
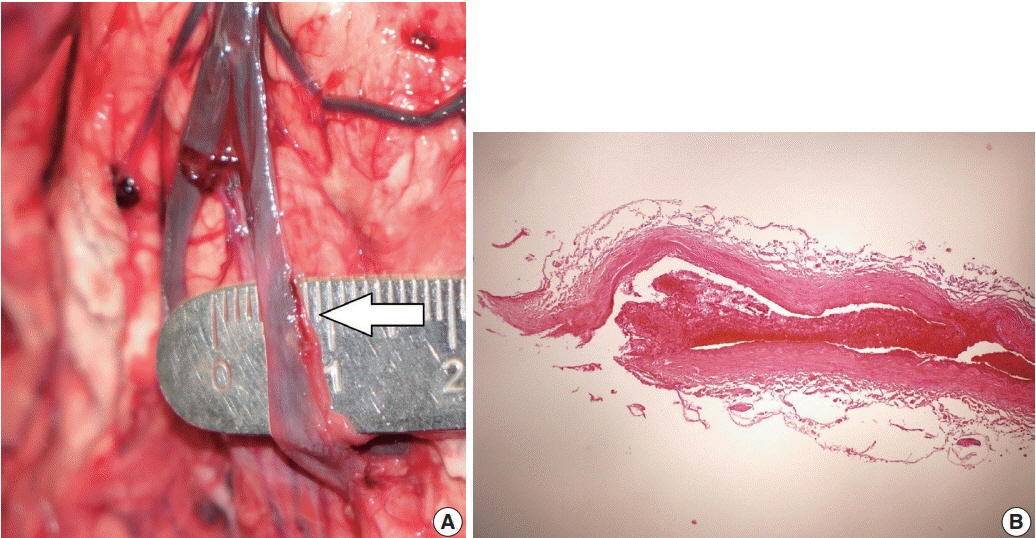
Inconspicuous longitudinal tears of the intracranial vertebral artery in traumatic basal subarachnoid hemorrhage
- Affiliations
-
- 1Central Forensic Medical Center, National Forensic Service, Wonju, Korea
- KMID: 2501608
- DOI: http://doi.org/10.4132/jptm.2019.10.15
Abstract
- Blunt force trauma to the head or neck region can cause traumatic basal subarachnoid hemorrhage (TBSAH), which can result in rapid loss of consciousness and death; however, detecting such a vascular injury is difficult. Posterior neck dissection was performed to investigate the bleeding focus in TBSAH cases 2018 and 2019. In all four cases, autopsies revealed a longitudinal tear in the midsection of the vertebral artery’s intracranial portion. The midportion of the intracranial vertebral artery appears to be most vulnerable to TBSAH. Interestingly, three of the cases showed only a vaguely visible longitudinal fissure in the artery without a grossly apparent tear; rupture was confirmed by microscopic examination. Longitudinal fissures of the intracranial vertebral artery, which are difficult to identify without detailed examination, may be overlooked in some cases of TBSAH. Thus, careful gross and microscopic examination of the vertebral artery is recommended in cases of TBSAH.
Figure
Reference
-
1. Lee CK, Gray L, Maguire J. Traumatic Vertebral Artery Injury: Detailed Clinicopathologic And Morphometric Analysis Of 6 Cases . Am J Forensic Med Pathol. 2009; 30:134–6.2. Wong B, Ong BB, Milne N. The source of haemorrhage in traumatic basal subarachnoid haemorrhage. J Forensic Leg Med. 2015; 29:18–23.
Article3. Kim S, Kim M, Lee BW, Kim YH, Choi YS, Seo JS. Investigation of bleeding focus in the intracranial vertebral artery with the use of posterior neck dissection method in traumatic basal subarachnoid hemorrhage. J Forensic Leg Med. 2015; 34:151–4.
Article4. Kim S, Jun YJ, Na JI, Kim M. Rupture portions in the vertebral artery in traumatic basal subarachnoid hemorrhage. J Forensic Leg Med. 2017; 52:221–2.
Article5. Contostavlos DL. Massive subarachnoid hemorrhage due to laceration of the vertebral artery associated with fracture of the transverse process of the atlas. J Forensic Sci. 1971; 16:40–56.6. Harland WA, Pitts JF, Watson AA. Subarachnoid haemorrhage due to upper cervical trauma. J Clin Pathol. 1983; 36:1335–41.
Article7. Leadbeatter S. Extracranial vertebral artery injury: evolution of a pathological illusion? Forensic Sci Int. 1994; 67:33–40.8. Ong BB, Milne N. Vertebral artery trauma. In : Rutty GN, editor. Essentials of autopsy practice: reviews, updates, and advances. Cham: Springer;2017. p. 23–41.9. McCarthy JH, Sunter JP, Cooper PN. A method for demonstrating the source of bleeding in cases of traumatic subarachnoid haemorrhage. J Pathol. 1999; 187:30A.10. Coast GC, Gee DJ. Traumatic subarachnoid haemorrhage: an alternative source. J Clin Pathol. 1984; 37:1245–8.
Article11. Hiraiwa K, Sato T, Sasaki T, Mizusawa I, Nata M, Kodama N. Medico-legal aspects of traumatic injury of the vertebrobasilar artery. Neurol Med Chir (Tokyo). 2005; 45:549–55.
Article12. Kumar V, Abbas AK, Aster JC. Robbins basic pathology. Philadelphia, PA: Elsevier;2018. p. 101–11.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Intracranial Vertebral Artery Dissecting Aneurysm Improved by Antiplatelets Therapy
- Dissecting Aneurysm of Intracranial Vertebral Artery: Report of Two Autopsy Cases
- Traumatic Aneurysm of the Pericallosal artery
- Subarachnoid Hemorrhage Presenting with Seizure due to Cerebrospinal Fluid Leakage after Spinal Surgery
- Subsequent Subarachnoid Hemorrhage from Clinically Unrelated Vertebral Artery Dissection after Thrombolytic Therapy