Anesth Pain Med.
2022 Jan;17(1):75-86. 10.17085/apm.21094.
Analgesic effects of ultrasound-guided fourquadrant transversus abdominis plane in patients with cytoreductive surgery with hyperthermic intraperitoneal chemotherapy: a prospective, randomized, controlled study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Dankook University Hospital, Cheonan, Korea
- 2Department of Surgery, Dankook University Hospital, Cheonan, Korea
- KMID: 2526531
- DOI: http://doi.org/10.17085/apm.21094
Abstract
- Background
Postoperative pain occurring after cytoreductive surgery (CRS) with hyperthermic intraperitoneal chemotherapy (HIPEC) is difficult to control because of extensive surgical injuries and long incisions. We assessed whether the addition of a four-quadrant transabdominal plane (4Q-TAP) block could help in analgesic control.
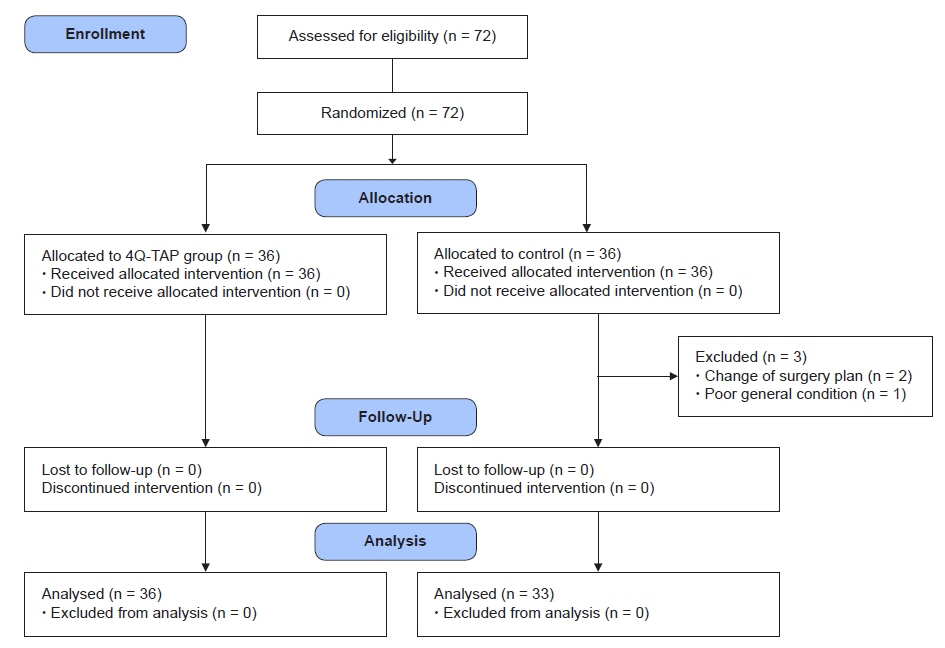
Methods
Seventy-two patients scheduled to undergo elective CRS with HIPEC and intravenous patient-controlled analgesia (IV PCA) were enrolled. The patients received 4Q-TAP blocks in a 10 ml mixture of 2% lidocaine and 0.75% ropivacaine per site (4Q-TAP group, n = 36) or normal saline (control group, n = 33). Oxycodone in the post-anesthesia care unit (PACU) and pethidine or tramadol in the ward were used as rescue analgesics. The primary outcome was less than 3 times of rescue analgesic administration (%) in the ward for 5 postoperative days. Secondary endpoints included oxycodone requirement in PACU, fentanyl doses of IV PCA, morphine milligram equivalent (MME) of total opioid use, hospital stay, and postoperative complications.
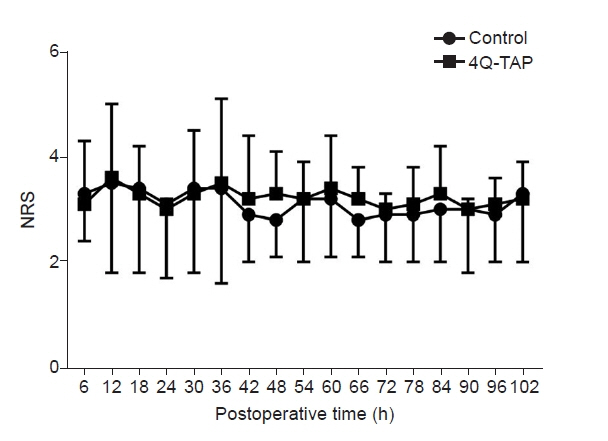
Results
During 5 postoperative days, there was no difference in pain scores and total rescue analgesic administration between two groups. However, the use of oxycodone in PACU (P = 0.011), fentanyl requirement in IV PCA (P = 0.029), and MME/kg of total opioid use (median, 2.35 vs. 3.21 mg/kg, P = 0.009) were significantly smaller in the 4Q-TAP group. Hospital stay and incidence of postoperative morbidity were similar in both groups.
Conclusions
The 4Q-TAP block enhanced multimodal analgesia and decreased opioid requirements in patients with CRS with HIPEC, but did not change postoperative recovery outcomes.
Keyword
Figure
Reference
-
1. Webb C, Day R, Velazco CS, Pockaj BA, Gray RJ, Stucky CC, et al. Implementation of an enhanced recovery after surgery (ERAS) program is associated with improved outcomes in patients undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2020; 27:303–12.2. Hübner M, Kusamura S, Villeneuve L, Al-Niaimi A, Alyami M, Balonov K, et al. Guidelines for perioperative care in cytoreductive surgery (CRS) with or without hyperthermic Intraperitoneal chemotherapy (HIPEC): enhanced recovery after surgery (ERAS®) Society recommendations - part I: preoperative and intraoperative management. Eur J Surg Oncol. 2020; 46:2292–310.3. Hausken J, Fretland ÅA, Edwin B, Andersen MH, Dagenborg VJ, Bjørnelv GMW, et al. Intravenous patient-controlled analgesia versus thoracic epidural analgesia after open liver surgery: a prospective, randomized, controlled, noninferiority trial. Ann Surg. 2019; 270:193–9.4. Abdelrahman I, Steinvall I, Elmasry M, Sjoberg F. Lidocaine infusion has a 25% opioid-sparing effect on background pain after burns: a prospective, randomised, double-blind, controlled trial. Burns. 2020; 46:465–71.5. Zhang B, Wang G, Liu X, Wang TL, Chi P. The opioid-sparing effect of perioperative dexmedetomidine combined with oxycodone infusion during open hepatectomy: a randomized controlled trial. Front Pharmacol. 2018; 8:940.6. Jin HS, Kim YC, Yoo Y, Lee C, Cho CW, Kim WJ. Opioid sparing effect and safety of nefopam in patient controlled analgesia after laparotomy: a randomized, double blind study. J Int Med Res. 2016; 44:844–54.7. Wang X, Li T. Postoperative pain pathophysiology and treatment strategies after CRS + HIPEC for peritoneal cancer. World J Surg Oncol. 2020; 18:62.8. Niraj G, Kelkar A, Hart E, Kaushik V, Fleet D, Jameson J. Four quadrant transversus abdominis plane block and continuous transversus abdominis plane analgesia: a 3-year prospective audit in 124 patients. J Clin Anesth. 2015; 27:579–84.9. Whelton A. Nephrotoxicity of nonsteroidal anti-inflammatory drugs: physiologic foundations and clinical implications. Am J Med. 1999; 106:13S–24S.10. Choi BM. A new therapeutic option for postoperative pain management with oxycodone HCI injection. Korean J Anesthesiol. 2016; 69:211–8.11. Howes TE, Cook TM, Corrigan LJ, Dalton SJ, Richards SK, Peden CJ. Postoperative morbidity survey, mortality and length of stay following emergency laparotomy. Anaesthesia. 2015; 70:1020–7.12. Pierre S, Whelan R. Nausea and vomiting after surgery. Contin Educ Anaesth Crit Care Pain. 2013; 13:28–32.13. Dubé P, Sideris L, Law C, Mack L, Haase E, Giacomantonio C, et al. Guidelines on the use of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in patients with peritoneal surface malignancy arising from colorectal or appendiceal neoplasms. Curr Oncol. 2015; 22:e100–12.14. Lee Y. What repeated measures analysis of variances really tells us. Korean J Anesthesiol. 2015; 68:340–5.15. Park E, Cho M, Ki CS. Correct use of repeated measures analysis of variance. Korean J Lab Med. 2009; 29:1–9.16. Sinatra RS, Jahr JS, Watkins-Pitchford JM. Oral and parenteral opioid analgesics. In: The essence of analgesia and analgesics. Edited by Sinatra RS, Jahr JS, Watkins-Pitchford JM: Cambridge, Cambridge University Press. 2010, pp 73-180.17. Korakianitis O, Daskalou T, Alevizos L, Stamou K, Mavroudis C, Iatrou C, et al. Lack of significant intraoperative coagulopathy in patients undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) indicates that epidural anaesthesia is a safe option. Int J Hyperthermia. 2015; 31:857–62.18. Hurdle H, Bishop G, Walker A, Moazeni A, Paloucci EO, Temple W, et al. Coagulation after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: a retrospective cohort analysis. Can J Anaesth. 2017; 64:1144–52.19. Ioannidis A, Arvanitidis K, Filidou E, Valatas V, Stavrou G, Michalopoulos A, et al. The length of surgical skin incision in postoperative inflammatory reaction. JSLS. 2018; 22:e2018.00045.20. Kim SS, Niu X, Elliott IA, Jiang JP, Dann AM, Damato LM, et al. Epidural analgesia improves postoperative pain control but impedes early discharge in patients undergoing pancreatic surgery. Pancreas. 2019; 48:719–25.21. Børglum J, Maschmann C, Belhage B, Jensen K. Ultrasound-guided bilateral dual transversus abdominis plane block: a new four-point approach. Acta Anaesthesiol Scand. 2011; 55:658–63.22. Cata JP, Fournier K, Corrales G, Owusu-Agyemang P, Soliz J, Bravo M, et al. HIPEC study group. The impact of thoracic epidural analgesia versus four quadrant transversus abdominis plane block on quality of recovery after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy surgery: a single-center, noninferiority, randomized, controlled trial. Ann Surg Oncol. 2021; 28:5297–310.23. Tsai HC, Yoshida T, Chuang TY, Yang SF, Chang CC, Yao HY, et al. Transversus abdominis plane block: an updated review of anatomy and techniques. Biomed Res Int. 2017; 2017:8284363.24. Huang D, Song L, Li Y, Xu Z, Li X, Li C. Posteromedial quadratus lumborum block versus transversus abdominal plane block for postoperative analgesia following laparoscopic colorectal surgery: a randomized controlled trial. J Clin Anesth. 2020; 62:109716.25. Forero M, Heikkila A, Paul JE, Cheng J, Thabane L. Lumbar transversus abdominis plane block: the role of local anesthetic volume and concentration-a pilot, prospective, randomized, controlled trial. Pilot Feasibility Stud. 2015; 1:10.26. Lahlou-Casulli M, Chaize-Avril C, Pouliquen E, Desfourneaux V, Mazoit JX, Malledant Y, et al. The median effective analgesic dose (ED50) of ropivacaine in ultrasound-guided transversus abdominis plane block for analgesia in reversal of ileostomy: a double-blind up-down dose-finding study. Eur J Anaesthesiol. 2015; 32:640–4.27. Cuvillon P, Nouvellon E, Ripart J, Boyer JC, Dehour L, Mahamat A, et al. A comparison of the pharmacodynamics and pharmacokinetics of bupivacaine, ropivacaine (with epinephrine) and their equal volume mixtures with lidocaine used for femoral and sciatic nerve blocks: a double-blind randomized study. Anesth Analg. 2009; 108:641–9.28. Zhao X, Tong Y, Ren H, Ding XB, Wang X, Zong JY, et al. Transversus abdominis plane block for postoperative analgesia after laparoscopic surgery: a systematic review and meta-analysis. Int J Clin Exp Med. 2014; 7:2966–75.29. Song Y, Shim JK, Song JW, Kim EK, Kwak YL. Dexmedetomidine added to an opioid-based analgesic regimen for the prevention of postoperative nausea and vomiting in highly susceptible patients: a randomised controlled trial. Eur J Anaesthesiol. 2016; 33:75–83.30. Foo I, Macfarlane AJR, Srivastava D, Bhaskar A, Barker H, Knaggs R, et al. The use of intravenous lidocaine for postoperative pain and recovery: international consensus statement on efficacy and safety. Anaesthesia. 2021; 76:238–50.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analgesic efficacy of ultrasound-guided transversus abdominis plane block for laparoscopic gynecological surgery: a randomized controlled trial
- Chemotherapy for ovarian cancer
- Effect of addition of buprenorphine or dexamethasone to levobupivacaine on postoperative analgesia in ultrasound guided transversus abdominis plane block in patients undergoing unilateral inguinal hernia repair: a prospective randomized double blind controlled trial
- Comparison of the effectiveness of subcostal transversus abdominis plane and rectus sheath blocks in postoperative analgesia in major open gynecological cancer surgeries: a prospective randomized study
- Transversus abdominis plane block as a sole anesthetic technique for evacuation of rectus abdominis muscle hematoma - A case report -