J Dent Rehabil Appl Sci.
2021 Mar;37(1):16-22. 10.14368/jdras.2021.37.1.16.
Comparative study of flexural strength of temporary restorative resin according to surface polishing and fabrication methods
- Affiliations
-
- 1Department of Prosthodontics, College of Dentistry, Wonkwang University, Iksan, Republic of Korea
- KMID: 2525973
- DOI: http://doi.org/10.14368/jdras.2021.37.1.16
Abstract
- Purpose
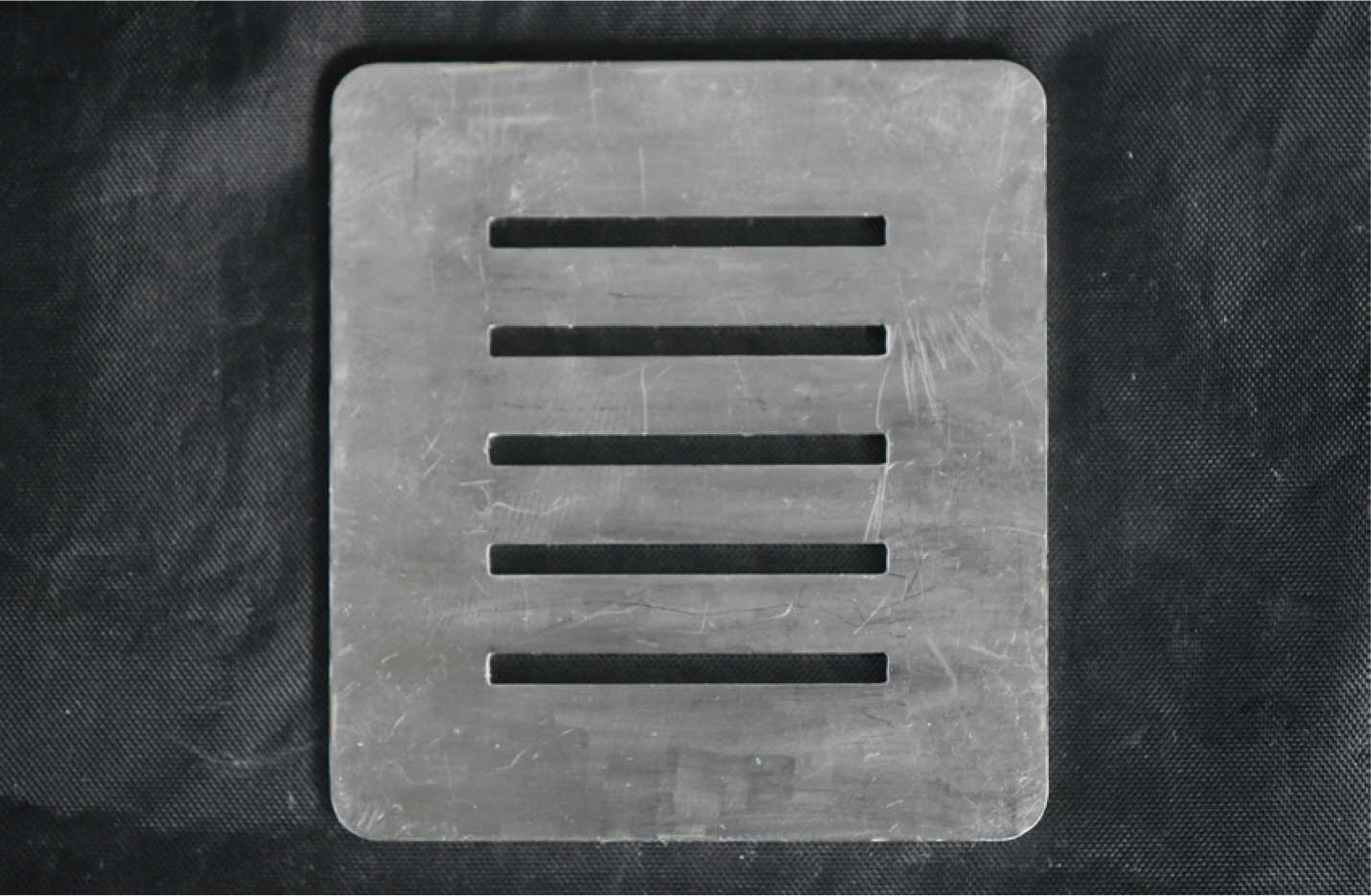
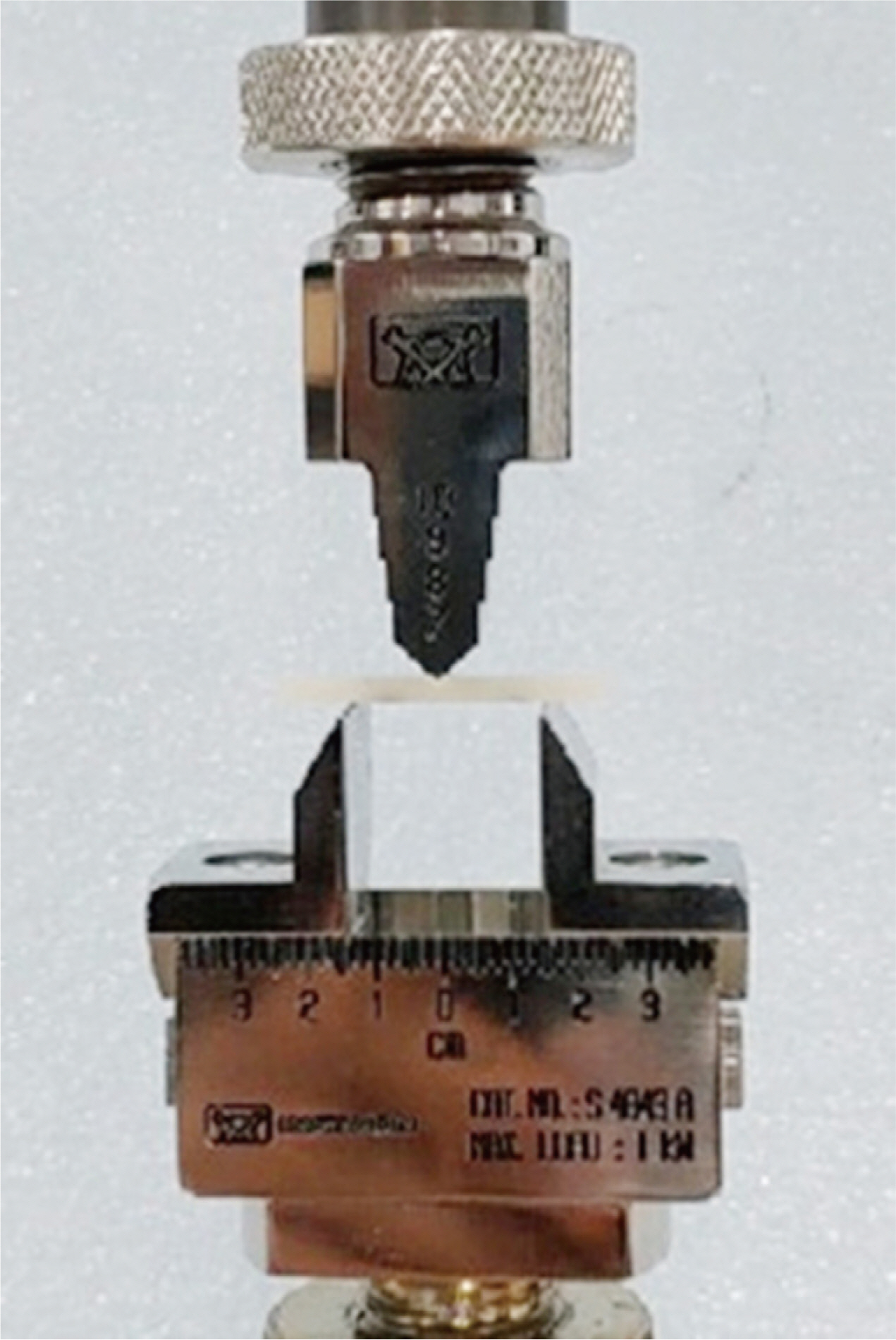
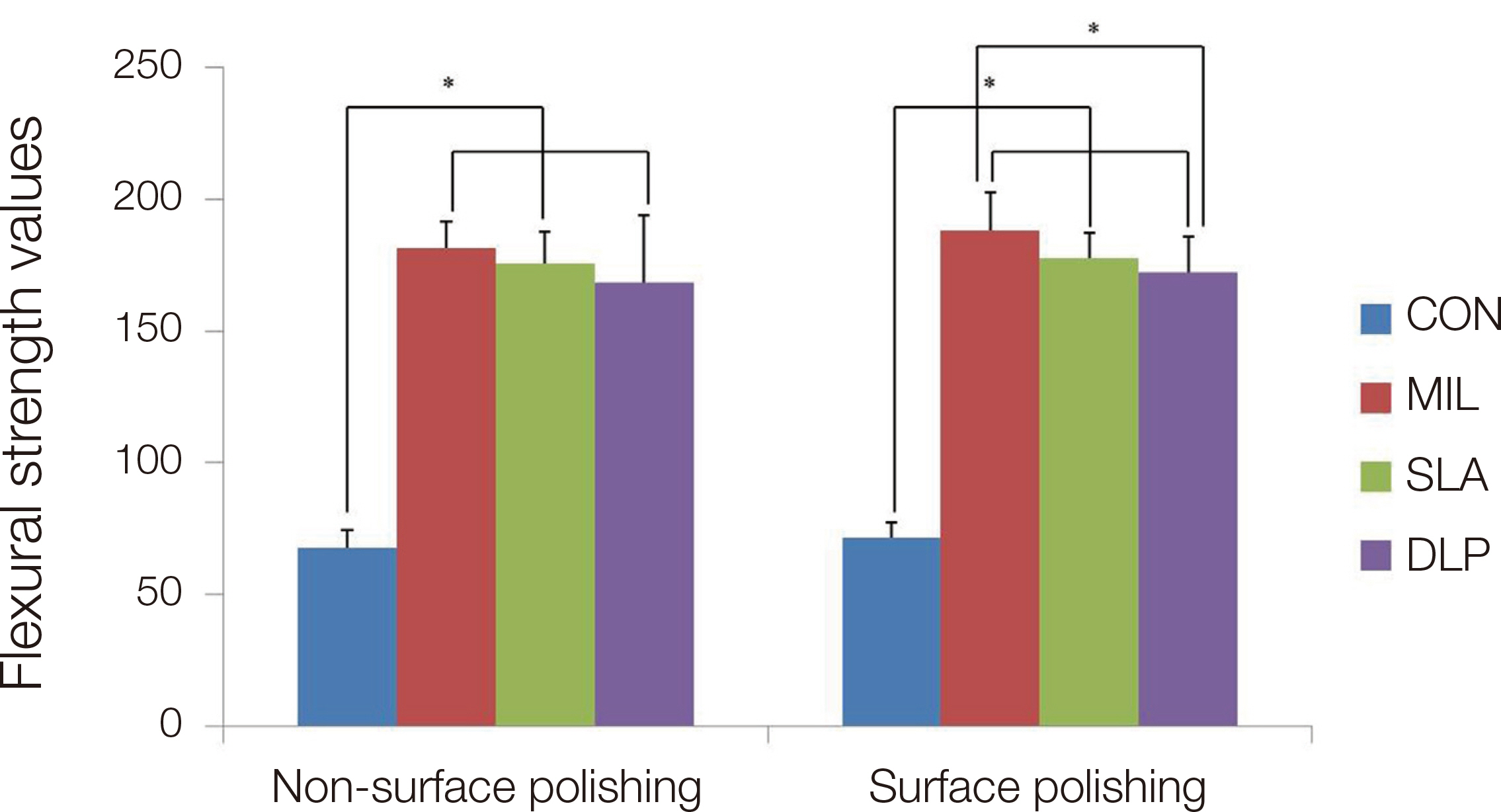
The purpose of this study is to investigate the effect of surface polishing and fabrication method on the flexural strength of temporary restorative resin. Materials and Methods: Each of four fabrication methods was used to make 30 temporary restorative resin specimens and the specimens were divided into two groups depending on whether they were polished by mechanical polishing. Specimens were stored in 37°C thermostat for 24 hours. Flexural strength was measured using a universal testing machine (UTM). The data obtained through the experiment were analyzed with Two-way ANOVA, Tukey’s HSD test and Paired t-test. Results: CAD/CAM milling group showed the highest flexural strength regardless of surface polishing. In decreasing order, the flexural strength of the other fabrication method group was as follows SLA 3D printing, DLP 3D printing, and Conventional method group. Conclusion: Surface polishing did not affect flexural strength of the temporary restorative resin (P > 0.05). However, there were statistically significant differences in flexural strength depending on fabrication method (P < 0.05).
Figure
Reference
-
References
1. Koumjian JH, Holmes JB. 1990; Marginal accuracy of provisional restorative materials. J Prosthet Dent. 63:639–42. DOI: 10.1016/0022-3913(90)90320-C. PMID: 2362244.2. Burns DR, Beck DA, Nelson SK. 2003; A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J Prosthet Dent. 90:474–97. DOI: 10.1016/S0022-3913(03)00259-2. PMID: 14586312.3. Haselton DR, Diaz-Arnold AM, Vargas MA. 2002; Flexural Strength of Provisional Crown and Fixed Partial Denture Resins. J Prosthet Dent. 87:225–8. DOI: 10.1067/mpr.2002.121406. PMID: 11854681.4. Ireland MF, Dixon DL, Breeding LC, Ramp MH. 1998; In Vitro Mechanical Property Comparison of Four Resins Used for Fabrication of Provisional Fixed Restorations. J Prosthet Dent. 80:158–62. DOI: 10.1016/S0022-3913(98)70104-0. PMID: 9710816.5. Diaz-Arnold AM, Dunne JT, Jones AH. 1999; Microhardness of provisional fixed prosthodontics materials. J Prosthet Dent. 82:525–8. DOI: 10.1016/S0022-3913(99)70050-8.6. Park JY, Jeong ID, Lee JJ, Bae SY, Kim JH, Kim WC. 2016; In vitro assessment of the marginal and internal fits of interim implant restorations fabricated with different methods. J Prosthet Dent. 116:536–42. DOI: 10.1016/j.prosdent.2016.03.012. PMID: 27174406.7. Kim KB, Kim JH, Kim WC, Kim JH. 2014; Three-dimensional evaluation of gaps associated with fixed dental prostheses fabricated with new technologies. J Prosthet Dent. 112:1432–6. DOI: 10.1016/j.prosdent.2014.07.002. PMID: 25218032.8. Park SM, Kim SK, Park JM, Kim KH, Jeon YT, Koak JY. 2017; Flexural strength of various kinds of the resin bridges fabricated with 3D printing. J Dent Rehabil Appl Sci. 33:260–8. DOI: 10.14368/jdras.2017.33.4.260.9. Karaokutan I, Sayin G, Kara O. 2015; In vitro study of fracture strength of provisional crown materials. J Adv Prosthodont. 7:27–31. DOI: 10.4047/jap.2015.7.1.27. PMID: 25722834. PMCID: PMC4341183.10. Cho WT, Choi JW. 2019; Comparison analysis of fracture load and flexural strength of provisional restorative resins fabricated by different methods. J Korean Acad Prosthodont. 57:225–31. DOI: 10.4047/jkap.2019.57.3.225.11. Gonçalves TS, de Menezes LM, Silva LEA. 2008; Residual monomer of autopolymerized acrylic resin according to different manipulation and polishing methods. An in situ evaluation. Angle Orthod. 78:722–7. DOI: 10.2319/0003-3219(2008)078[0722:RMOAAR]2.0.CO;2. PMID: 18302474.12. Palitsch A, Hannig M, Ferger P, Balkenhol M. 2012; Bonding of acrylic denture teeth to MMA/PMMA and light-curing denture base materials: the role of conditioning liquids. J Dent. 40:210–21. DOI: 10.1016/j.jdent.2011.12.010. PMID: 22207164.13. Wang X, Huyang G, Palagummi SV, Liu X, Skrtic D, Beauchamp C, Bowen R, Sun J. 2018; High performance dental resin composites with hydrolytically stable monomers. Dent Mater. 34:228–37. DOI: 10.1016/j.dental.2017.10.007. PMID: 29113700.14. Donovan TE, Hurst RG, Campagni WV. 1985; Physical properties of acrylic resin polymerized by four different techniques. J Prosthet Dent. 54:522–4. DOI: 10.1016/0022-3913(85)90425-1. PMID: 3862809.15. Chee WW, Donovan TE, Daftary F, Siu TM. 1988; The effect of vacuum-mixed autopolymerizing acrylic resins on porosity and transverse strength. J Prosthet Dent. 60:517–9. DOI: 10.1016/0022-3913(88)90261-2. PMID: 3183991.16. Yao J, Li J, Wang Y, Huang H. 2014; Comparison of the flexural strength and marginal accuracy of traditional and CAD/CAM interim materials before and after thermal cycling. J Prosthet Dent. 112:649–57. DOI: 10.1016/j.prosdent.2014.01.012. PMID: 24721504.17. Reeponmaha T, Angwaravong O, Angwarawong T. 2020; Comparison of fracture strength after thermomechanical aging between provisional crowns made with CAD/CAM and conventional method. J Adv Prosthodont. 12:218–24. DOI: 10.4047/jap.2020.12.4.218. PMID: 32879712. PMCID: PMC7449821.18. Ayman AD. 2017; The residual monomer content and mechanical properties of CAD/CAM resins used in the fabrication of complete dentures as compared to heat cured resins. Electron Physician. 9:4766–72. DOI: 10.19082/4766. PMID: 28894533. PMCID: PMC5586991.19. Matsumura H, Leinfelder KF. 1994; Three-body wear of four types of light-activated composite resin veneering materials. Quintessence Int. 25:425–30. PMID: 7938432.20. Peutzfeldt A. 1997; Resin composites in dentistry: the monomer systems. Eur J Oral Sci. 105:97–116. DOI: 10.1111/j.1600-0722.1997.tb00188.x. PMID: 9151062.21. Lee S. 2016; Prospect for 3D Printing Technology in Medical, Dental, and Pediatric Dental Field. J Korean Acad Pediatr Dent. 43:93–108. DOI: 10.5933/JKAPD.2016.43.1.93.22. Dikova T, Dzhendov DA, Ivanov D, Bliznakova K. 2018; Dimensional accuracy and surface roughness of polymeric dental bridges produced by different 3D printing processes. Arch Mater Sci Eng. 94:65–75. DOI: 10.5604/01.3001.0012.8660.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of surface finishes on flexural strength, fracture toughness of feldspathic dental porcelain
- Effect of fabrication method and surface polishing on the surface roughness and microbial adhesion of provisional restoration
- A study of the antifungal properties and flexural strength of 3D printed denture base resin containing titanium dioxide nanoparticles
- The effect of different fiber reinforcements on flexural strength of provisional restorative resins: an in-vitro study
- The effects of surface grinding and polishing on the phase transformation and flexural strength of zirconia