Clin Endosc.
2022 Jan;55(1):136-140. 10.5946/ce.2020.232.
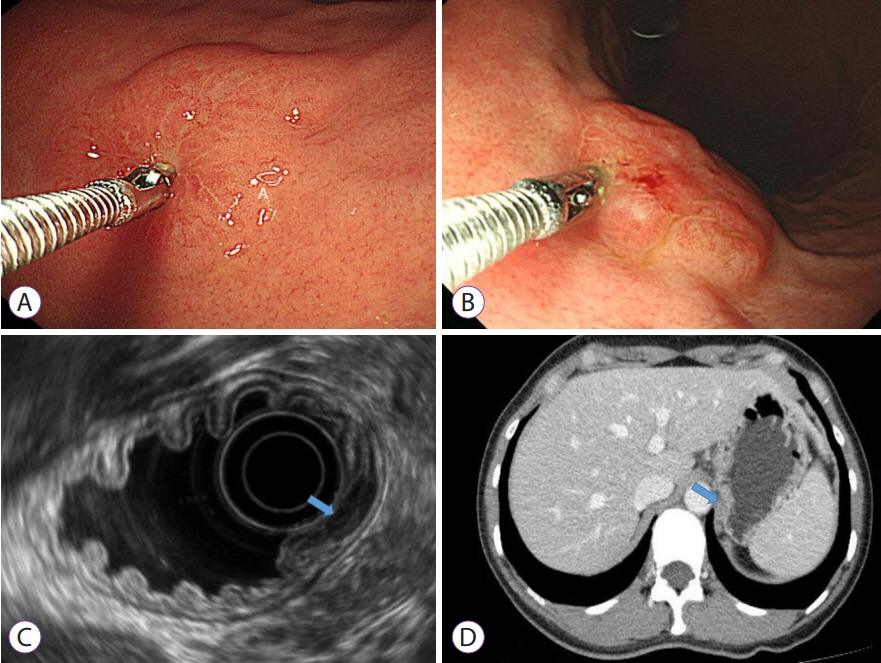
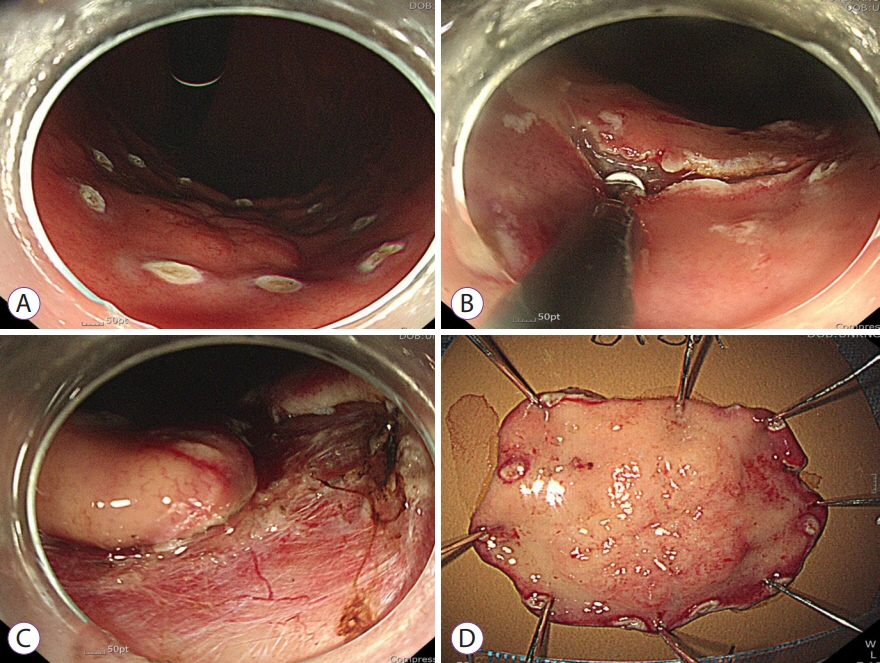
Successful Endoscopic Resection of Gastric Mucosa-Associated Lymphoid Tissue Lymphoma Unresponsive to Helicobacter pylori Eradication Therapy
- Affiliations
-
- 1Department of Internal Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea
- KMID: 2525060
- DOI: http://doi.org/10.5946/ce.2020.232
Abstract
- Eradication of Helicobacter pylori is the first-line treatment for gastric mucosa-associated lymphoid tissue (MALT) lymphomas; however, lesions may persist in 20% of patients after initial treatment, thereby necessitating the use of an additional therapeutic approach. Other treatment options include radiation therapy, chemotherapy, endoscopic resection, rituximab therapy, or watchful waiting. We present a case of localized gastric MALT lymphoma that did not respond to H. pylori eradication therapy. The patient waited for 12 months but the tumor showed no signs of regression endoscopically. Histologic examination revealed residual MALT lymphoma. The tumor was then successfully treated using endoscopic submucosal dissection and the patient remained disease-free for 4 years. To our knowledge, this is the first case in which a gastric MALT lymphoma was treated with endoscopic submucosal dissection. In conclusion, endoscopic resection may be recommended as second-line therapy for properly selected patients with gastric MALT lymphoma as it is effective and minimally invasive.
Keyword
Figure
Cited by 1 articles
-
상피하종양 형태의 식도 MALT 림프종 1예
Ha Eun Lee, Gwang Ha Kim, Min Ji Kim, Kyung Bin Kim, Dong Chan Joo, Hye Kyung Jeon, Moon Won Lee, Bong Eun Lee
Korean J Gastroenterol. 2024;83(4):157-162. doi: 10.4166/kjg.2024.021.
Reference
-
1. Ott G, Balague-Ponz O, de Leval L, de Jong D, Hasserjian RP, Elenitoba-Johnson KS. Commentary on the WHO classification of tumors of lymphoid tissues (2008): indolent B cell lymphomas. J Hematop. 2009; 2:77–81.2. Nakamura S, Sugiyama T, Matsumoto T, et al. Long-term clinical outcome of gastric MALT lymphoma after eradication of Helicobacter pylori: a multicentre cohort follow-up study of 420 patients in Japan. Gut. 2012; 61:507–513.3. Wündisch T, Thiede C, Morgner A, et al. Long-term follow-up of gastric MALT lymphoma after Helicobacter pylori eradication. J Clin Oncol. 2005; 23:8018–8024.4. Cheson BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014; 32:3059–3068.5. Copie-Bergman C, Wotherspoon AC, Capella C, et al. Gela histological scoring system for post-treatment biopsies of patients with gastric MALT lymphoma is feasible and reliable in routine practice. Br J Haematol. 2013; 160:47–52.6. Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection-the Maastricht V/Florence consensus report. Gut. 2017; 66:6–30.7. Zucca E, Arcaini L, Buske C, et al. Marginal zone lymphomas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020; 31:17–29.8. Ruskoné-Fourmestraux A, Fischbach W, Aleman BM, et al. EGILS consensus report. Gastric extranodal marginal zone B-cell lymphoma of MALT. Gut. 2011; 60:747–758.9. Kim GH, Choi BG, Lee JN, et al. 2 cases of gastric mucosa-associated lymphoid tissue lymphoma presenting as a submucosal tumor-like lesion. Korean J Gastroenterol. 2010; 56:103–108.10. Toyoda H, Ono T, Kiyose M, et al. Gastric mucosa-associated lymphoid tissue lymphoma with a focal high-grade component diagnosed by EUS and endoscopic mucosal resection for histologic evaluation. Gastrointest Endosc. 2000; 51:752–755.11. Noda M, Mori N, Nomura K, et al. Regression of idiopathic thrombocytopenic purpura after endoscopic mucosal resection of gastric mucosa associated lymphoid tissue lymphoma. Gut. 2004; 53:1698–1700.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Polypoid Mucosa-Associated Lymphoid Tissue Lymphoma of the Stomach Treated with Endoscopic Polypectomy
- Unusual Treatment of Gastric Mucosa Associated Lymphoid Tissue Lymphoma Unresponsive to Helicobacter pylori Eradication
- Helicobacter pylori-negative Gastric Mucosa-associated Lymphoid Tissue Lymphoma
- Clinical Efficacy of Radiotherapy in Helicobacter pylori Negative or Unresponsive to Eradication Therapy Primary Gastric Mucosa-Associated Lymphoid Tissue Lymphoma
- Two Cases of Gastric MALT Lymphoma Diagnosed at Long Last after Successful Eradication of Helicobacter pylori