Clin Endosc.
2022 Jan;55(1):86-94. 10.5946/ce.2021.084.
Clinical Impact of Different Reconstruction Methods on Remnant Gastric Cancer at the Anastomotic Site after Distal Gastrectomy
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Graduate School of Medicine, Kobe University, Kobe, Japan
- 2Division of Pathology, Department of Pathology, Kobe University Graduate School of Medicine, Kobe, Japan
- 3Department of Gastroenterology, Kishiwada Tokushukai Hospital, Kishiwada, Japan
- KMID: 2525054
- DOI: http://doi.org/10.5946/ce.2021.084
Abstract
- Background/Aims
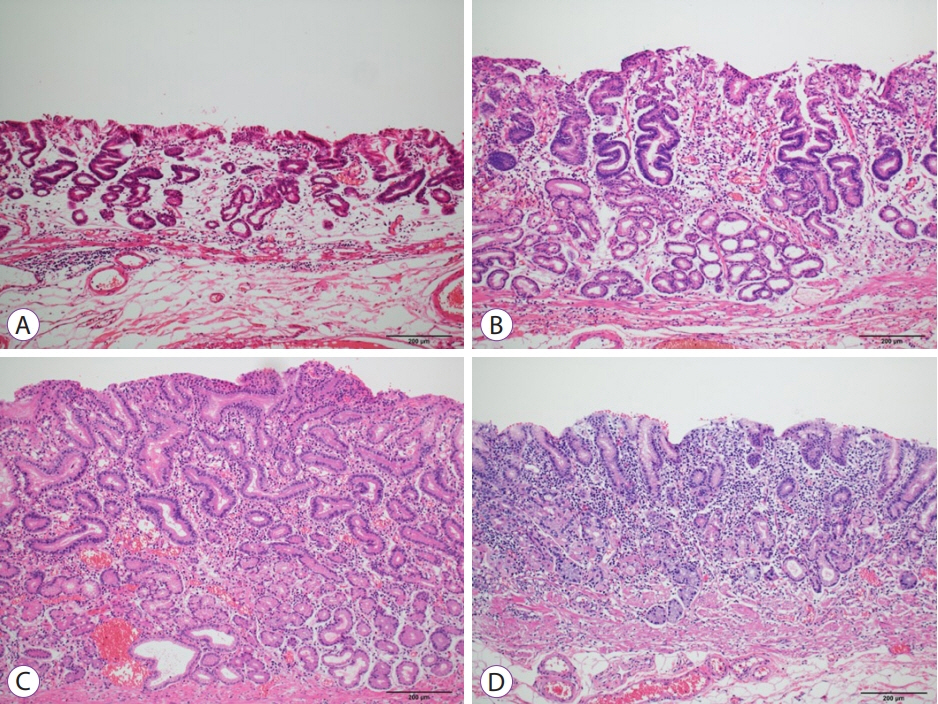
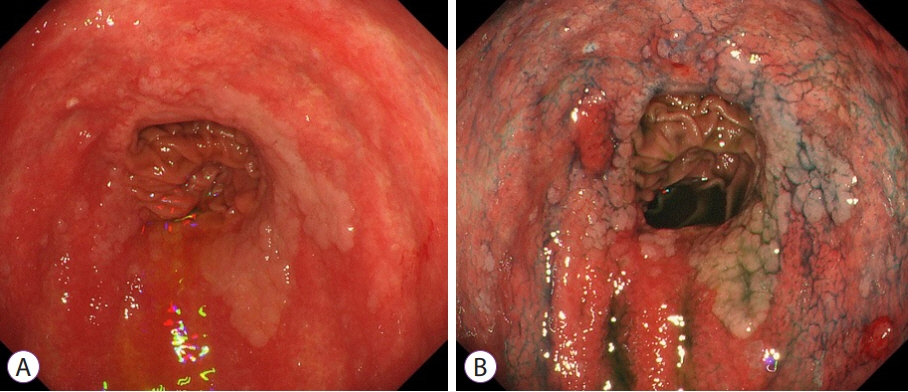
The anastomotic site after distal gastrectomy is the area most affected by duodenogastric reflux. Different reconstruction methods may affect the lesion characteristics and treatment outcomes of remnant gastric cancers at the anastomotic site. We retrospectively investigated the clinicopathologic and endoscopic submucosal dissection outcomes of remnant gastric cancers at the anastomotic site.
Methods
We recruited 34 consecutive patients who underwent endoscopic submucosal dissection for remnant gastric cancer at the anastomotic site after distal gastrectomy. Clinicopathology and treatment outcomes were compared between the Billroth II and non-Billroth II groups.
Results
The tumor size in the Billroth II group was significantly larger than that in the non-Billroth II group (22 vs. 19 mm; p=0.048). More severe gastritis was detected endoscopically in the Billroth II group (2 vs. 1.33; p=0.0075). Moreover, operation time was longer (238 vs. 121 min; p=0.004) and the frequency of bleeding episodes was higher (7.5 vs. 3.1; p=0.014) in the Billroth II group.
Conclusions
Compared to remnant gastric cancers in non-Billroth II patients, those in the Billroth II group had larger lesions with a background of severe remnant gastritis. Endoscopic submucosal dissection for remnant gastric cancers in Billroth II patients involved longer operative times and more frequent bleeding episodes than that in patients without Billroth II.
Keyword
Figure
Reference
-
1. Toyonaga T, Man-i M, East JE, et al. 1,635 endoscopic submucosal dissection cases in the esophagus, stomach, and colorectum: complication rates and long-term outcomes. Surg Endosc. 2013; 27:1000–1008.2. Ohashi M, Katai H, Fukagawa T, Gotoda T, Sano T, Sasako M. Cancer of the gastric stump following distal gastrectomy for cancer. Br J Surg. 2007; 94:92–95.3. Mezhir JJ, Gonen M, Ammori JB, Strong VE, Brennan MF, Coit DG. Treatment and outcome of patients with gastric remnant cancer after resection for peptic ulcer disease. Ann Surg Oncol. 2011; 18:670–676.4. Kaneko K, Kondo H, Saito D, et al. Early gastric stump cancer following distal gastrectomy. Gut. 1998; 43:342–344.5. Sinning C, Schaefer N, Standop J, Hirner A, Wolff M. Gastric stump carcinoma - epidemiology and current concepts in pathogenesis and treatment. Eur J Surg Oncol. 2007; 33:133–139.6. Ohira M, Toyokawa T, Sakurai K, et al. Current status in remnant gastric cancer after distal gastrectomy. World J Gastroenterol. 2016; 22:2424–2433.7. Lee JY, Choi IJ, Cho SJ, et al. Endoscopic submucosal dissection for metachronous tumor in the remnant stomach after distal gastrectomy. Surg Endosc. 2010; 24:1360–1366.8. Hoteya S, Iizuka T, Kikuchi D, Yahagi N. Clinical advantages of endoscopic submucosal dissection for gastric cancers in remnant stomach surpass conventional endoscopic mucosal resection. Dig Endosc. 2010; 22:17–20.9. Hirasaki S, Kanzaki H, Matsubara M, Fujita K, Matsumura S, Suzuki S. Treatment of gastric remnant cancer post distal gastrectomy by endoscopic submucosal dissection using an insulation-tipped diathermic knife. World J Gastroenterol. 2008; 14:2550–2555.10. Nishide N, Ono H, Kakushima N, et al. Clinical outcomes of endoscopic submucosal dissection for early gastric cancer in remnant stomach or gastric tube. Endoscopy. 2012; 44:577–583.11. Osumi W, Fujita Y, Hiramatsu M, et al. Endoscopic submucosal dissection allows less-invasive curative resection for gastric tube cancer after esophagectomy - a case series. Endoscopy. 2009; 41:777–780.12. Tanaka S, Toyonaga T, Morita Y, et al. Endoscopic submucosal dissection for early gastric cancer in anastomosis site after distal gastrectomy. Gastric Cancer. 2014; 17:371–376.13. Katai H, Nunobe S, Saka M, Fukagawa T, Sano T. [Reconstruction after distal gastrectomy]. Nihon Geka Gakkai Zasshi. 2008; 109:264–268.14. Kobori O, Shimizu T, Maeda M, et al. Enhancing effect of bile and bile acid on stomach tumorigenesis induced by N-methyl-N’-nitro-N-nitrosoguanidine in Wistar rats. J Natl Cancer Inst. 1984; 73:853–861.15. Kim MC, Kim W, Kim HH, et al. Risk factors associated with complication following laparoscopy-assisted gastrectomy for gastric cancer: a large-scale korean multicenter study. Ann Surg Oncol. 2008; 15:2692–2700.16. Zong L, Chen P. Billroth I vs. Billroth II vs. Roux-en-Y following distal gastrectomy: a meta-analysis based on 15 studies. Hepatogastroenterology. 2011; 58:1413–1424.17. Lee MS, Ahn SH, Lee JH, et al. What is the best reconstruction method after distal gastrectomy for gastric cancer? Surg Endosc. 2012; 26:1539–1547.18. Japanese Society of Gastric Cancer Eds. Gastric cancer treatment guidelines. Tokyo, Japan: Kanehara Shuppan;2018.19. Kubo M, Sasako M, Gotoda T, et al. Endoscopic evaluation of the remnant stomach after gastrectomy: proposal for a new classification. Gastric Cancer. 2002; 5:83–89.20. Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996; 20:1161–1181.21. Yano T, Hasuike N, Ono H, et al. Factors associated with technical difficulty of endoscopic submucosal dissection for early gastric cancer that met the expanded indication criteria: post hoc analysis of a multi-institutional prospective confirmatory trial (JCOG0607). Gastric Cancer. 2020; 23:168–174.22. Tajiri H, Kitano S. Complications associated with endoscopic mucosal resection: definition of bleeding that can be viewed as accidental. Dig Endosc. 2004; 16:S134–S136.23. Nomura K, Hoteya S, Kikuchi D, Inoshita N, Iizuka T. Utility of endoscopic submucosal dissection in the remnant stomach and clinical outcomes for different reconstruction methods. Digestion. 2019; 100:254–261.24. Takamaru H, Saito Y, Yamada M, et al. Clinical impact of endoscopic clip closure of perforations during endoscopic submucosal dissection for colorectal tumors. Gastrointest Endosc. 2016; 84:494–502.e1.25. Kato M, Takeuchi Y, Yamasaki Y, et al. Technical feasibility of line-assisted complete closure technique for large mucosal defects after colorectal endoscopic submucosal dissection. Endosc Int Open. 2017; 5:E11–E16.26. Dohi O, Yoshida N, Naito Y, et al. Efficacy and safety of endoscopic submucosal dissection using a scissors-type knife with prophylactic over-the-scope clip closure for superficial non-ampullary duodenal epithelial tumors. Dig Endosc. 2020; 32:904–913.27. Takimoto K, Hagiwara A. Filling and shielding for postoperative gastric perforations of endoscopic submucosal dissection using polyglycolic acid sheets and fibrin glue. Endosc Int Open. 2016; 4:E661–E664.28. Sakaguchi H, Takao T, Takegawa Y, et al. Efficacy of the envelope method in applying polyglycolic acid sheets to post-endoscopic submucosal dissection ulcers in living pigs. Clin Endosc. 2021; 54:64–72.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Laparoscopic Approach Also Safe for the Treatment of Remnant Gastric Cancer?
- Entirely Laparoscopic Gastrectomy and Colectomy for Remnant Gastric Cancer with Gastric Outlet Obstruction and Transverse Colon Invasion
- Surgery for Cancer Arising at an Anastomotic Site after Radical Total Gastrctomy
- Omental Free-Shaped Flap Reinforcement on the Anastomosis and Dissected Area (OFFROAD) Following Reconstruction after Gastrectomy: A Retrospective Case-Control Study
- Proximal Gastrectomy for Upper-third Early Gastric Cancer