J Korean Med Sci.
2022 Jan;37(4):e27. 10.3346/jkms.2022.37.e27.
Relationship Between Appendectomy Incidence and Computed Tomography Scans Based on Korean Nationwide Data, 2003–2017
- Affiliations
-
- 1Department of Surgery, St. Vincent’s Hospital, College of Medicine, the Catholic University of Korea, Seoul, Korea
- 2Artificial Intelligence and Big-Data Convergence Center, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 3Center for Public Healthcare, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 4Departement of Preventive Medicine, Gachon University College of Medicine, Incheon, Korea
- 5Department of Surgery, Seoul St. Mary’s Hospital, College of Medicine, the Catholic University of Korea, Seoul, Korea
- KMID: 2525008
- DOI: http://doi.org/10.3346/jkms.2022.37.e27
Abstract
- Background
Advances in medicine and changes in the medical environment can affect the diagnosis and treatment of diseases. The main purpose of the present study was to investigate whether the difference in accessibility to diagnosis and treatment facilities influenced the occurrence of appendectomy in Korea.
Methods
We collected data on 183,531 appendectomy patients between 2003 and 2017 using the National Health Insurance Services claims. Retrospective analysis of relationship between the age-standardized rate (ASR) of appendectomy and clinical variables affecting medical accessibility was performed. Pearson’s correlation analyses were used.
Results
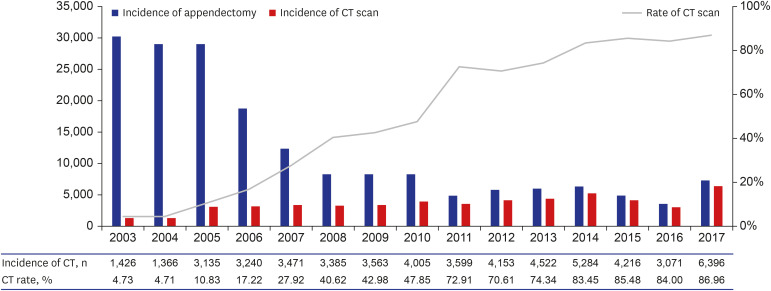
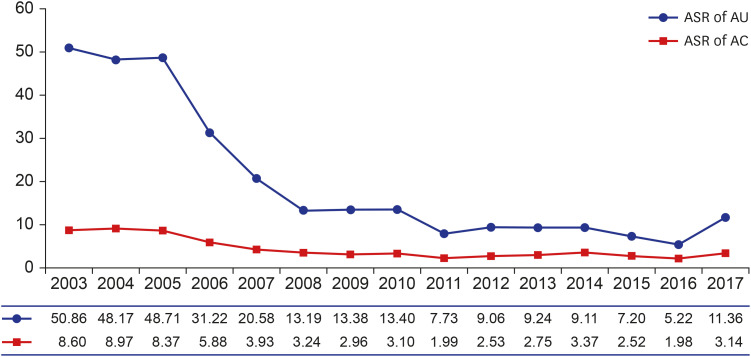
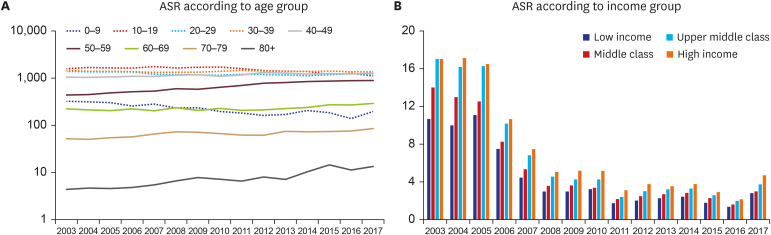
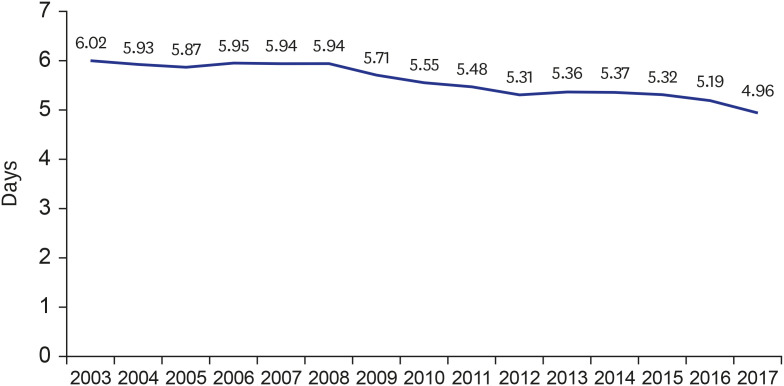
The incidence of appendectomy decreased from 30,164 cases in 2003 to 7,355 cases in 2017. The rate of computerized tomography (CT) scans for diagnosis of appendicitis increased from 4.73% in 2003 to 86.96% in 2017. The ASR of appendectomy in uncomplicated and complicated appendicitis decreased from 48.71 in 2005 to 13.40 in 2010 and 8.37 in 2005 to 2.96 in 2009, respectively. The ASR of appendectomy was higher in the high-income group. The proportion and ASR of appendectomy in older age group increased steadily with years. The total admission days continued to decrease from 6.02 days in 2003 to 4.96 days in 2017.
Conclusion
The incidence of appendectomy was seemingly associated with the rate of CT scan. In particular, the incidence of appendectomy in uncomplicated appendicitis was markedly reduced. Through enhanced accessibility to CT scans, accurate diagnosis and treatment of appendicitis can be facilitated.
Figure
Reference
-
1. Nishi M, Ishihara S, Nakajima T, Ohta K, Ohyama S, Ohta H. Chronological changes of characteristics of early gastric cancer and therapy: experience in the Cancer Institute Hospital of Tokyo, 1950-1994. J Cancer Res Clin Oncol. 1995; 121(9-10):535–541. PMID: 7559733.
Article2. Kim HH, Ahn SH. The current status and future perspectives of laparoscopic surgery for gastric cancer. J Korean Surg Soc. 2011; 81(3):151–162. PMID: 22066116.
Article3. Kim YI, Kim YW, Choi IJ, Kim CG, Lee JY, Cho SJ, et al. Long-term survival after endoscopic resection versus surgery in early gastric cancers. Endoscopy. 2015; 47(4):293–301. PMID: 25625697.
Article4. World Health Organization. Republic of Korea Health System Review. Manila, Philippines: WHO Regional Office for the Western Pacific;2015.5. Colson M, Skinner KA, Dunnington G. High negative appendectomy rates are no longer acceptable. Am J Surg. 1997; 174(6):723–726. PMID: 9409605.
Article6. Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S, et al. US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology. 2006; 241(1):83–94. PMID: 16928974.
Article7. Tseng J, Cohen T, Melo N, Alban RF. Imaging utilization affects negative appendectomy rates in appendicitis: an ACS-NSQIP study. Am J Surg. 2019; 217(6):1094–1098. PMID: 30635205.
Article8. Korean Statistical Information Service. Updated 2020. Accessed April 15, 2021. http://kosis.kr/index/index.do .9. Raman SS, Osuagwu FC, Kadell B, Cryer H, Sayre J, Lu DS. Effect of CT on false positive diagnosis of appendicitis and perforation. N Engl J Med. 2008; 358(9):972–973. PMID: 18305278.
Article10. Braveman P, Schaaf VM, Egerter S, Bennett T, Schecter W. Insurance-related differences in the risk of ruptured appendix. N Engl J Med. 1994; 331(7):444–449. PMID: 7880234.
Article11. Bagger JP, Zindrou D, Taylor KM. Postoperative infection with meticillin-resistant Staphylococcus aureus and socioeconomic background. Lancet. 2004; 363(9410):706–708. PMID: 15001331.
Article12. Na BJ, Hong JY, Kim KY, Lee MS, Nam HS, Im JS, et al. The relation between type of insurance and acute appendicitis rupture rate. J Prev Med Public Health. 2004; 37(3):267–273. PMID: 25175473.13. Putnam LR, Tsao K, Nguyen HT, Kellagher CM, Lally KP, Austin MT. The impact of socioeconomic status on appendiceal perforation in pediatric appendicitis. J Pediatr. 2016; 170:156–160.e1. PMID: 26922766.14. Sutton TL, Pracht EE, Ciesla DJ. Acute appendicitis: variation in outcomes by insurance status. J Surg Res. 2016; 201(1):118–125. PMID: 26850192.
Article15. Drake FT, Mottey NE, Farrokhi ET, Florence MG, Johnson MG, Mock C, et al. Time to appendectomy and risk of perforation in acute appendicitis. JAMA Surg. 2014; 149(8):837–844. PMID: 24990687.
Article16. Sauvain MO, Slankamenac K, Muller MK, Wildi S, Metzger U, Schmid W, et al. Delaying surgery to perform CT scans for suspected appendicitis decreases the rate of negative appendectomies without increasing the rate of perforation nor postoperative complications. Langenbecks Arch Surg. 2016; 401(5):643–649. PMID: 27146319.
Article17. Kim JH, Kim HY, Park SK, Lee JS, Heo DS, Park SW, et al. Single-incision laparoscopic appendectomy versus conventional laparoscopic appendectomy: experiences from 1208 cases of single-incision laparoscopic appendectomy. Ann Surg. 2015; 262(6):1054–1058. PMID: 26559780.18. Talha A, El-Haddad H, Ghazal AE, Shehata G. Laparoscopic versus open appendectomy for perforated appendicitis in adults: randomized clinical trial. Surg Endosc. 2020; 34(2):907–914. PMID: 31139982.
Article19. Kim WJ, Mun JY, Kim HJ, Yoon SH, Han SR, Bae JH, et al. Surgical rectus sheath block combined with multimodal pain management reduces postoperative pain and analgesic requirement after single-incision laparoscopic appendectomy: a retrospective study. Int J Colorectal Dis. 2021; 36(1):75–82. PMID: 32875376.
Article20. Seo JW, Kim MJ, Yoon SH, Paik KY, Park SM, Kang WK, et al. The effects of preoperative pain education on the decision to discharge patients following single-incision laparoscopic appendectomy. Ann Coloproctol. 2020; 36(6):398–402. PMID: 32054252.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- National Trends in Pediatric CT Scans in South Korea: A Nationwide Cohort Study
- Usefulness of Preoperative Computed Tomography in Children with Clinically Suspected Appendicitis
- Utility of Abdominal Computerized Tomography in Diagnosis of Acute Appendicitis
- Comparison between an Interval Appendectomy and an Urgent Appendectomy for Patients of Periappendiceal Abscess
- Chronological trends in patients undergoing cholecystectomy in Korea: a nationwide health insurance claims study