Obstet Gynecol Sci.
2022 Jan;65(1):29-36. 10.5468/ogs.21135.
Clinical manifestations and pregnancy outcomes of COVID-19 in indonesian referral hospital in central pandemic area
- Affiliations
-
- 1Department of Obstetrics and Gynaecology, Airlangga University Hospital, Universitas Airlangga Faculty of Medicine, Surabaya, Indonesia
- 2Department of Obstetrics and Gynaecology, Faculty of Medicine Dr. Soetomo General Academic Hospital, Surabaya, Indonesia
- 3Department of Obstetrics and Gynaecology, Lyell McEwin Hospital, University of Adelaide, Adelaide, Australia
- KMID: 2524682
- DOI: http://doi.org/10.5468/ogs.21135
Abstract
Objectives
Data on the clinical manifestations and pregnancy outcomes of pregnant women with COVID-19 are limited, particularly in developing countries. The aim of this study was to analyze the clinical manifestations and pregnancy outcomes in COVID-19 maternal cases in a large referral hospital in Indonesia.
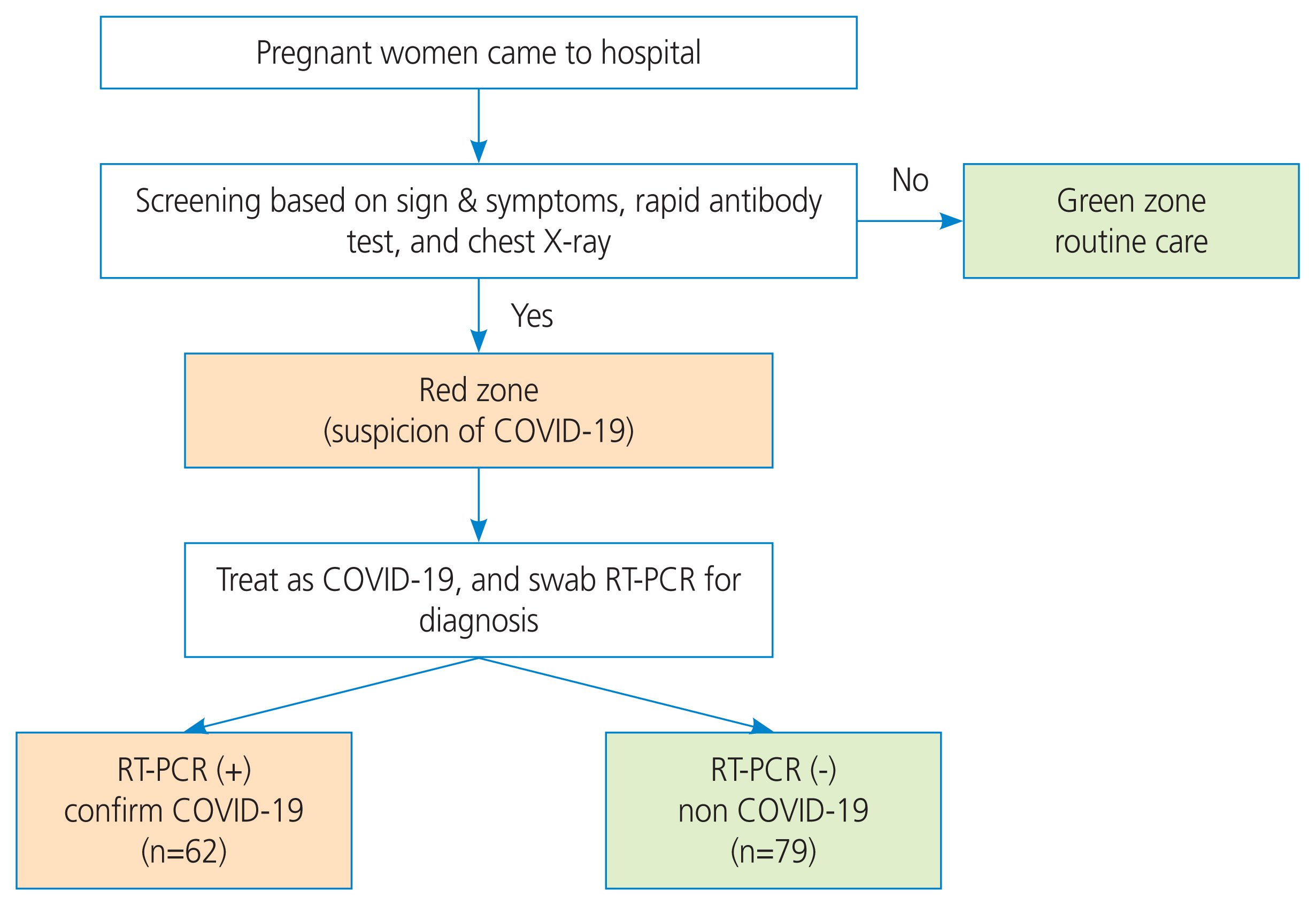
Methods
This study used a prospective cohort design and included all pregnant women with suspected COVID-19. Subjects were divided into COVID-19 and non-COVID-19 groups based on the results of real-time polymerase chain reaction (RT-PCR) for severe acute respiratory syndrome coronavirus 2. Clinical characteristics, laboratory results, and pregnancy outcomes were compared between the two groups.
Results
Of the 141 suspected maternal cases, 62 cases were COVID-19-confirmed (43.9%), while 79 suspected cases were negative (56.1%). The clinical manifestations and laboratory findings between the two groups were not significantly different (P>0.05). However, the maternal mortality directly caused by COVID-19 was significantly higher than that in the non-COVID-19 group (8.3% vs. 1.3%; P=0.044; odd ratio, 6.91; 95% confidence interval, 0.79-60.81).
Conclusion
The clinical manifestations and laboratory results of suspected pregnant women with positive and negative RT-PCR COVID-19 results were similar. However, within the Indonesian setting, COVID-19 significantly increases the risk of maternal death through both direct and indirect factors.
Keyword
Figure
Cited by 1 articles
-
The introduction to air pollution on pregnancy outcome (APPO) study: a multicenter cohort study
Young Min Hur, Sunwha Park, Eunjin Kwon, Young-Ah You, AbuZar Ansari, Soo Min Kim, Gain Lee, Mi Hye Park, Kyung A Lee, Soo Jung Kim, Young-Han Kim, Yeon-Sung Jung, Geum Joon Cho, Min-Jeong Oh, Sung Hun Na, Se Jin Lee, Tae Gyu An, Jin-Gon Bae, Yu-Hwan Kim, Soo-Jeong Lee, Na Kyung Kim, Eun-Hee Ha, Young Ju Kim
Obstet Gynecol Sci. 2023;66(3):169-180. doi: 10.5468/ogs.22278.
Reference
-
References
1. Ardian M, Laksana C, Habibie PH, Wardhana MP, Erza K. Situation report: maternal health management during COVID-19 pandemic at soetomo general hospital and universitas airlangga academic hospital, surabaya indonesia. Sys Rev Pharm. 2020; 11:467–71.2. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020; 395:809–15.
Article3. Zaigham M, Andersson O. Maternal and perinatal outcomes with COVID-19: a systematic review of 108 pregnancies. Acta Obstet Gynecol Scand. 2020; 99:823–9.
Article4. Smith V, Seo D, Warty R, Payne O, Salih M, Chin KL, et al. Maternal and neonatal outcomes associated with COVID-19 infection: a systematic review. PLoS One. 2020; 15:e0234187.
Article5. Ashraf MA, Keshavarz P, Hosseinpour P, Erfani A, Roshanshad A, Pourdast A, et al. Coronavirus disease 2019 (COVID-19): a systematic review of pregnancy and the possibility of vertical transmission. J Reprod Infertil. 2020; 21:157–68.6. Panahi L, Amiri M, Pouy S. Risks of novel coronavirus disease (COVID-19) in pregnancy; a narrative review. Arch Acad Emerg Med. 2020; 8:e34.7. Anggraini NWP, Sulistyowati S. Low neutrophil-to-lmphocyte ratio decreases risk of coronavirus disease in pregnant women. Universa Med. 2020; 39:88–96.
Article8. Sutton D, Fuchs K, D’Alton M, Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020; 382:2163–4.
Article9. Aziz MA, Chalid MT, Saroyo YB, Budayasa R, Irwinda R, Akbar MIA. Rekomendasi penanganan virus corona (COVID-19) pada maternal (Hamil, Bersalin, dan Nifas) [Internet]. Jakarta (IND): POGI;c2020. [cited 2020 Oct 1]. Available from: https://pogi.or.id/publish/wp-content/uploads/2020/10/Rekomendasi-COVID-Maternal-POGI.pdf .10. Poon LC, Yang H, Kapur A, Melamed N, Dao B, Divakar H, et al. Global interim guidance on coronavirus disease 2019 (COVID-19) during pregnancy and puerperium from FIGO and allied partners: information for healthcare professionals. Int J Gynaecol Obstet. 2020; 149:273–86.
Article11. Donders F, Lonnée-Hoffmann R, Tsiakalos A, Mendling W, Martinez de Oliveira J, Judlin P, et al. ISIDOG recommendations concerning COVID-19 and pregnancy. Diagnostics (Basel). 2020; 10:243.
Article12. IoOaG RCPI. COVID-19 infection guidance for maternity services [Internet]. Dublin (IRL): Institute of Obstetricians and Gynaecologists;c2020. [cited 2020 Oct 2]. Available from: https://rcpi-live-cdn.s3.amazonaws.com/wp-content/uploads/2020/04/COVID19-Infection-Guidance-for-Maternity-Services-03_04_2020.pdf .13. Poon LC, Yang H, Dumont S, Lee JCS, Copel JA, Danneels L, et al. ISUOG interim guidance on coronavirus disease 2019 (COVID-19) during pregnancy and puerperium: information for healthcare professionals - an update. Ultrasound Obstet Gynecol. 2020; 55:848–62.14. Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020; 370:m3320.
Article15. Lopes de Sousa ÁF, Carvalho HEF, Oliveira LB, Schneider G, Camargo ELS, Watanabe E, et al. Effects of COVID-19 infection during pregnancy and neonatal prognosis: what is the evidence? Int J Environ Res Public Health. 2020; 17:4176.
Article16. Narang K, Enninga EAL, Gunaratne MDSK, Ibirogba ER, Trad ATA, Elrefaei A, et al. SARS-CoV-2 infection and COVID-19 during pregnancy: a multidisciplinary review. Mayo Clin Proc. 2020; 95:1750–65.
Article17. COVID-RANZCOG 19 and pregnancy in resource-limited environments [Internet]. Melbourneo (AUS): RANZCOG;c2020. [cited 2020 Oct 3]. Available from: https://ranzcog.edu.au/statements-guidelines/covid-19-statement/resource-limited-environments .18. Spanish Obstetric Emergency Group, Oscar Martínez Pérez. The association between COVID-19 and preterm delivery: a cohort study with a multivariate analysis. medRxiv. 2020. Sep. 07. [Epub]. https://doi.org/10.1101/2020.09.05.20188458 .19. Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol. 2004; 191:292–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Management of Thyroid Disease in COVID-19 Pandemic
- COVID-19 and Cancer: Questions to Be Answered
- Assessment and Management of Dysphagia during the COVID-19 Pandemic
- Skin Manifestations Following COVID-19 Vaccination: A Multicenter Case Series Study in Korea
- Neurological Manifestations in Patients with COVID-19: Experiences from the Central Infectious Diseases Hospital in South Korea