Cancer Res Treat.
2022 Jan;54(1):150-156. 10.4143/crt.2021.306.
Long-term Survival in Non–Small Cell Lung Cancer Patients with Metachronous Brain-Only Oligorecurrence Who Underwent Definitive Treatment
- Affiliations
-
- 1Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2524596
- DOI: http://doi.org/10.4143/crt.2021.306
Abstract
- Purpose
Metachronous brain-only oligorecurrence in patients with non–small cell lung cancer (NSCLC) is a rare event with favorable prognosis, but the clinical outcome has not been fully determined. We retrospectively analyzed clinical outcomes and prognostic factors in metachronous brain-only oligorecurrence in patients with NSCLC who underwent definitive treatment.
Materials and Methods
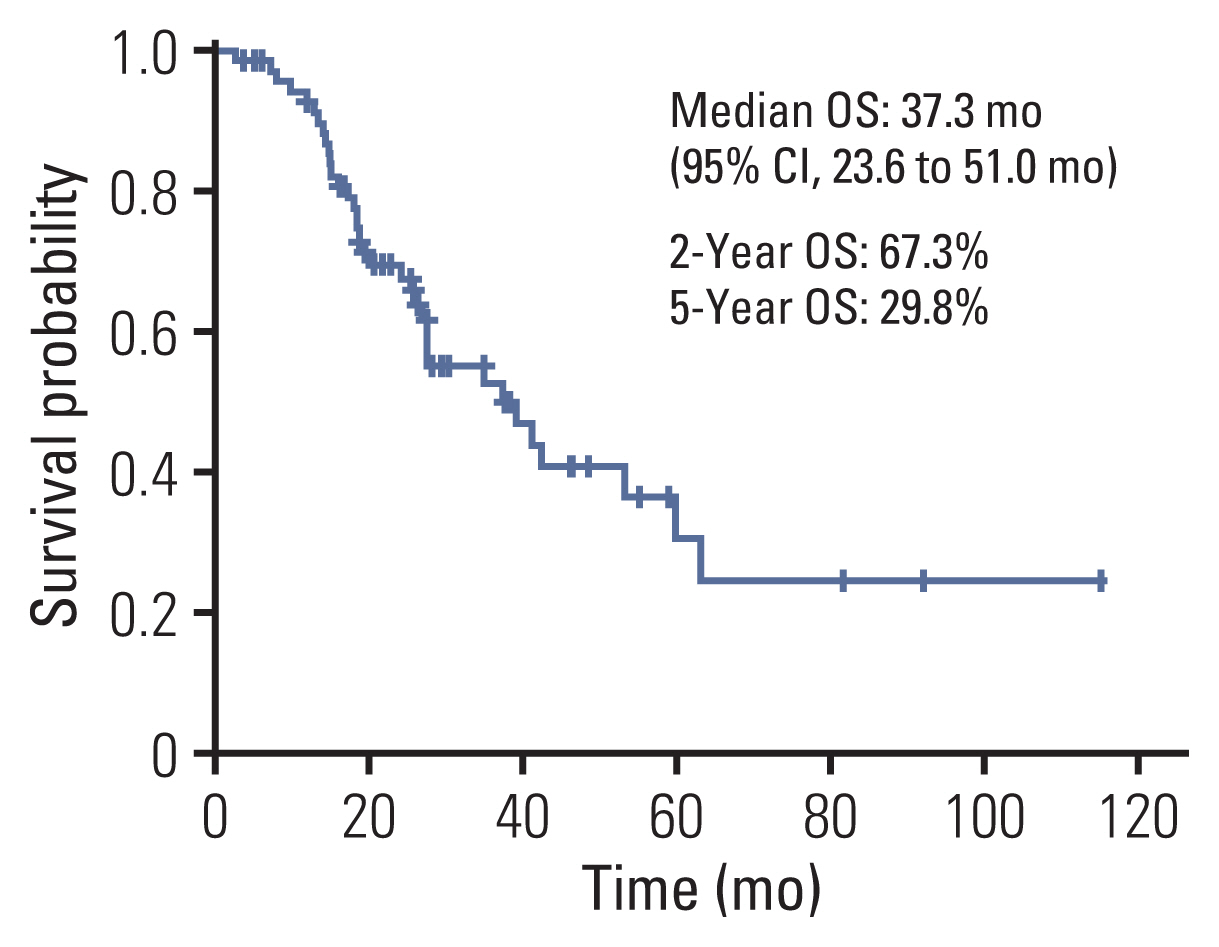
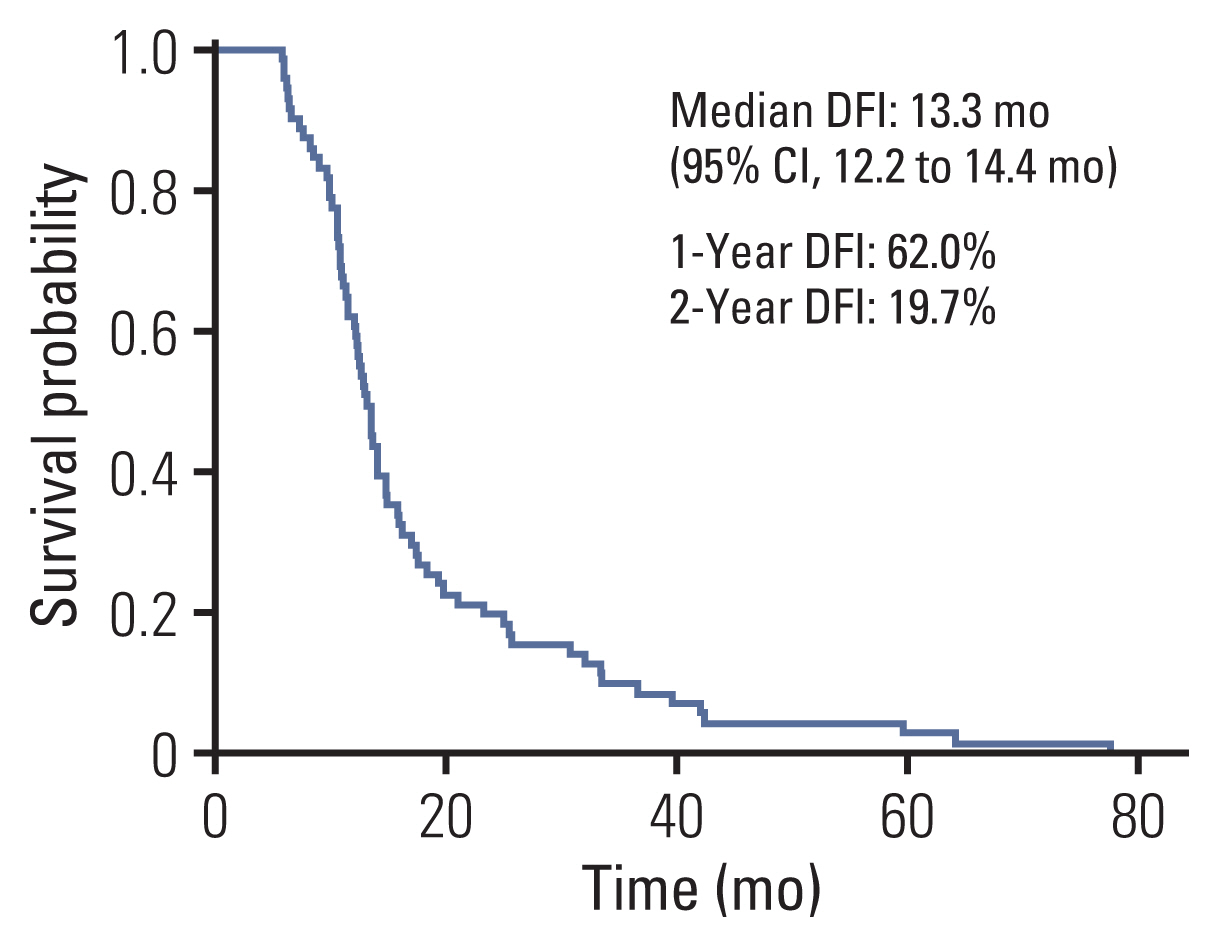
We reviewed 4,437 NSCLC patients without oncogenic driver mutations who underwent definitive treatment between 2008 and 2018. Among them, we identified 327 patients who developed 1 to 5 brain metastases with or without systemic metastasis. Of the 327 patients, 71 had metachronous brain-only oligorecurrence without extracranial progression and were treated with local therapy to the brain. Overall survival (OS), progression-free survival (PFS), and prognostic factors affecting OS were analyzed.
Results
The median OS was 38.9 months (95% confidence interval [CI], 21.8 to 56.1 months) in 71 patients. The 2-year OS rate was 67.8% and the 5-year OS rate was 33.1%. The median PFS was 25.5 months (95% CI, 12.2 to 14.4 months). The longest surviving patient had a survival period of 115 months. Through multivariate analysis, Eastern Cooperative Oncology Group ≥ 1 (hazard ratio, 5.33; p=0.005) was associated with poor survival. There was no significant difference in OS between patients with local therapy and those with local plus systemic therapy (18.5 months vs. 34.7 months, p=0.815).
Conclusion
Metachronous brain-only oligorecurrence NSCLC patients who underwent definitive treatment experienced long-term survival with local therapy, highlighting the unique patient population. The role of systemic chemotherapy in this patient population requires further investigation.
Figure
Reference
-
References
1. National Comprehensive Cancer Network. Non-small cell lung cancer (version 8.2020) [Internet]. Plymouth Meeting, PA: National Comprehensive Cancer Network;2020. [cited 2020 Sep 15]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf .2. O’Dowd EL, Kumaran M, Anwar S, Palomo B, Baldwin DR. Brain metastases following radical surgical treatment of non-small cell lung cancer: is preoperative brain imaging important? Lung Cancer. 2014; 86:185–9.
Article3. Gaspar LE, Chansky K, Albain KS, Vallieres E, Rusch V, Crowley JJ, et al. Time from treatment to subsequent diagnosis of brain metastases in stage III non-small-cell lung cancer: a retrospective review by the Southwest Oncology Group. J Clin Oncol. 2005; 23:2955–61.
Article4. Schouten LJ, Rutten J, Huveneers HA, Twijnstra A. Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer. 2002; 94:2698–705.
Article5. Gavrilovic IT, Posner JB. Brain metastases: epidemiology and pathophysiology. J Neurooncol. 2005; 75:5–14.
Article6. Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep. 2012; 14:48–54.
Article7. Scagliotti GV, De Marinis F, Rinaldi M, Crino L, Gridelli C, Ricci S, et al. Phase III randomized trial comparing three platinum-based doublets in advanced non-small-cell lung cancer. J Clin Oncol. 2002; 20:4285–91.
Article8. Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol. 1995; 13:8–10.
Article9. Niibe Y, Hayakawa K. Oligometastases and oligo-recurrence: the new era of cancer therapy. Jpn J Clin Oncol. 2010; 40:107–11.
Article10. Guckenberger M, Lievens Y, Bouma AB, Collette L, Dekker A, deSouza NM, et al. Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol. 2020; 21:e18–28.
Article11. de Vin T, Engels B, Gevaert T, Storme G, De Ridder M. Stereotactic radiotherapy for oligometastatic cancer: a prognostic model for survival. Ann Oncol. 2014; 25:467–71.
Article12. Ashworth AB, Senan S, Palma DA, Riquet M, Ahn YC, Ricardi U, et al. An individual patient data metaanalysis of outcomes and prognostic factors after treatment of oligometastatic non-small-cell lung cancer. Clin Lung Cancer. 2014; 15:346–55.
Article13. Gomez DR, Tang C, Zhang J, Blumenschein GR Jr, Hernandez M, Lee JJ, et al. Local consolidative therapy vs. maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer: long-term results of a multi-institutional, phase II, randomized study. J Clin Oncol. 2019; 37:1558–65.
Article14. Niibe Y, Nishimura T, Inoue T, Karasawa K, Shioyama Y, Jingu K, et al. Oligo-recurrence predicts favorable prognosis of brain-only oligometastases in patients with non-small cell lung cancer treated with stereotactic radiosurgery or stereotactic radiotherapy: a multi-institutional study of 61 subjects. BMC Cancer. 2016; 16:659.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adjuvant Chemotherapy for Completely Resected Non-Small Cell Lung Cancer
- Radiotherapy of Brain Metastases from Lung Cancer
- Definitive Radiotherapy of Non-Small Cell Lung Cancer
- Chemotherapy for Small Cell Lung Cancer
- A case of leptomeningeal metastasis from adenocarcinoma of the lung improved by treatment with Gefitinib