Prog Med Phys.
2021 Dec;32(4):159-164. 10.14316/pmp.2021.32.4.159.
Assessing Commercial CLEANBOLUS Based on Silicone for Clinical Use
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea
- 2Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul, Korea
- 3Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea
- 4Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2524163
- DOI: http://doi.org/10.14316/pmp.2021.32.4.159
Abstract
- Purpose
We investigated the properties of CLEANBOLUS based on silicone with suitable characteristics for clinical use.
Methods
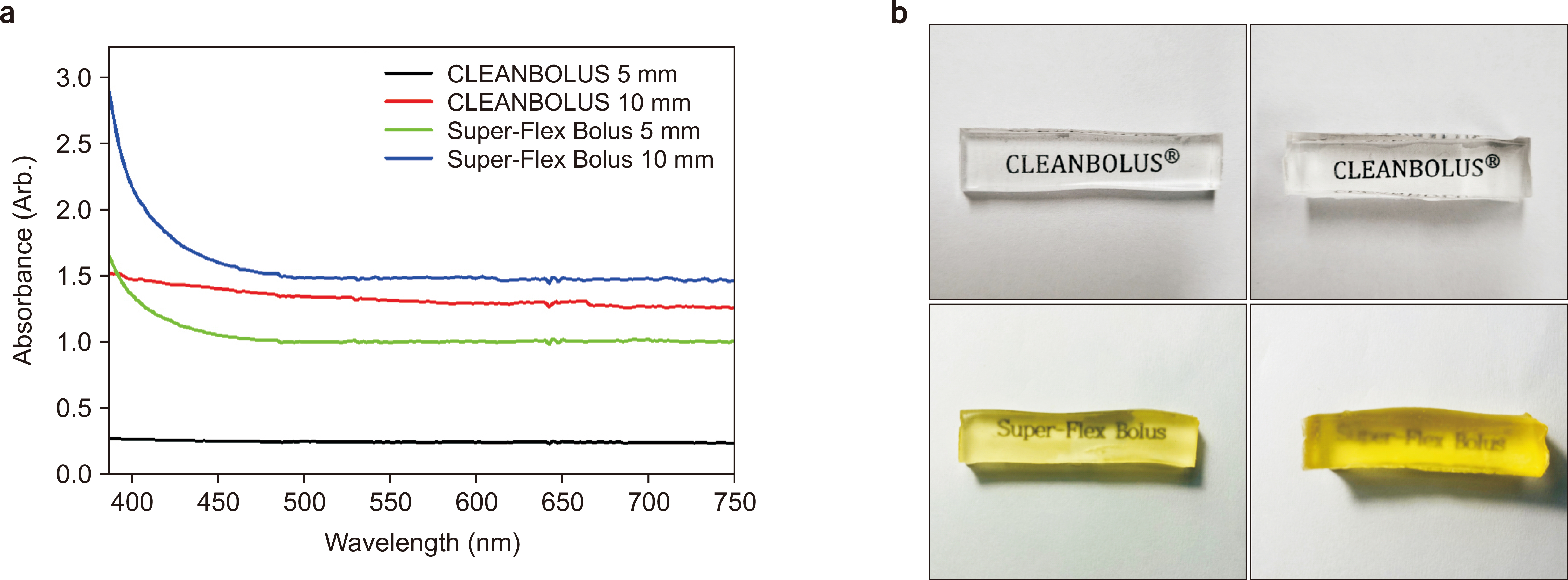
We evaluated the characteristics of CLEANBOLUS and compared the results with the commercial product (Super-Flex bolus). Also, we conducted physical evaluations, including shore hardness, element composition, and elongation break. Transparency was investigated through the measured absorbance within the visible region (400–700 nm). Also, dosimetric characteristics were investigated with surface dose and beam quality. Finally, the volume of unwanted air gap was investigated based on computed tomography images for breast, chin, and nose using Super-Flex bolus and CELANBOLUS.
Results
CLEANBOLUS showed excellent physical properties for a low shore hardness (000–35) and elongation break (>1,000%). Additionally, it was shown that CLEANBOLUS is more transparent than Super-Flex bolus. Dosimetric results obtained through measurement and calculation have an electron density similar to water in CLEANBOLUS. Finally, CLEANBOLUS showed that the volume of unwanted air gap between the phantom and each bolus is smaller than Super-Flex bolus for breast, chin, and nose.
Conclusions
The physical properties of CLEANBOLUS, including excellent adhesive strength and lower shore hardness, reduce unwanted air gaps and ensure accurate dose distribution. Therefore, it would be an alternative to other boluses, thus improving clinical use efficiency.
Keyword
Figure
Cited by 1 articles
-
Evaluations of a Commercial CLEANBOLUS-WHITE for Clinical Application
Geum Bong Yu, Jung-in Kim, Jaeman Son
Prog Med Phys. 2024;35(1):10-15. doi: 10.14316/pmp.2024.35.1.10.
Reference
-
References
1. Fein DA, Mendenhall WM, Parsons JT, Stringer SP, Cassisi NJ, Million RR. 1993; Pharyngeal wall carcinoma treated with radiotherapy: impact of treatment technique and fractionation. Int J Radiat Oncol Biol Phys. 26:751–757. DOI: 10.1016/0360-3016(93)90488-H.
Article2. Pignon JP, Arriagada R, Ihde DC, Johnson DH, Perry MC, Souhami RL, et al. 1992; A meta-analysis of thoracic radiotherapy for small-cell lung cancer. N Engl J Med. 327:1618–1624. DOI: 10.1056/NEJM199212033272302. PMID: 1331787.
Article3. Brenner DJ, Hall EJ. 1999; Fractionation and protraction for radiotherapy of prostate carcinoma. Int J Radiat Oncol Biol Phys. 43:1095–1101. DOI: 10.1016/S0360-3016(98)00438-6.
Article4. Mellenberg DE Jr. 1990; Determination of build-up region over-response corrections for a Markus-type chamber. Med Phys. 17:1041–1044. DOI: 10.1118/1.596579. PMID: 2280733.
Article5. Bilge H, Ozbek N, Okutan M, Cakir A, Acar H. 2010; Surface dose and build-up region measurements with wedge filters for 6 and 18 MV photon beams. Jpn J Radiol. 28:110–116. DOI: 10.1007/s11604-009-0393-5. PMID: 20182845.
Article6. Velkley DE, Manson DJ, Purdy JA, Oliver GD Jr. 1975; Build-up region of megavoltage photon radiation sources. Med Phys. 2:14–19. DOI: 10.1118/1.594158. PMID: 805358.
Article7. Dogan N, Glasgow GP. 2003; Surface and build-up region dosimetry for obliquely incident intensity modulated radiotherapy 6 MV x rays. Med Phys. 30:3091–3096. DOI: 10.1118/1.1625116. PMID: 14713075.
Article8. Ishmael Parsai E, Shvydka D, Pearson D, Gopalakrishnan M, Feldmeier JJ. 2008; Surface and build-up region dose analysis for clinical radiotherapy photon beams. Appl Radiat Isot. 66:1438–1442. DOI: 10.1016/j.apradiso.2008.02.089. PMID: 18434173.
Article9. Price S, Williams M, Butson M, Metcalfe P. 2006; Comparison of skin dose between conventional radiotherapy and IMRT. Australas Phys Eng Sci Med. 29:272–277. DOI: 10.1007/BF03178577. PMID: 17058590.
Article10. Weshler Z, Loewinger E, Loewenthal E, Levinson R, Fuks Z. 1986; Megavoltage radiotherapy using water bolus in the treatment of Kaposi's sarcoma. Int J Radiat Oncol Biol Phys. 12:2029–2032. DOI: 10.1016/0360-3016(86)90142-2.
Article11. Vyas V, Palmer L, Mudge R, Jiang R, Fleck A, Schaly B, et al. 2013; On bolus for megavoltage photon and electron radiation therapy. Med Dosim. 38:268–273. DOI: 10.1016/j.meddos.2013.02.007. PMID: 23582702.
Article12. Moyer RF, McElroy WR, O'Brien JE, Chamberlain CC. 1983; A surface bolus material for high-energy photon and electron therapy. Radiology. 146:531–532. DOI: 10.1148/radiology.146.2.6401364. PMID: 6401364.
Article13. Tieu MT, Graham P, Browne L, Chin YS. 2011; The effect of adjuvant postmastectomy radiotherapy bolus technique on local recurrence. Int J Radiat Oncol Biol Phys. 81:e165–e171. DOI: 10.1016/j.ijrobp.2011.01.002. PMID: 21362579.
Article14. Kawamoto T, Shikama N, Kurokawa C, Hara N, Oshima M, Sasai K. 2021; Dosimetric assessment of bolus for postmastectomy radiotherapy. Med Dosim. 46:e1–e4. DOI: 10.1016/j.meddos.2020.08.001. PMID: 32891467.
Article15. Butson MJ, Cheung T, Yu P, Metcalfe P. 2000; Effects on skin dose from unwanted air gaps under bolus in photon beam radiotherapy. Radiat Meas. 32:201–204. DOI: 10.1016/S1350-4487(99)00276-0.
Article16. Anderson PR, Hanlon AL, Fowble BL, McNeeley SW, Freedman GM. 2004; Low complication rates are achievable after postmastectomy breast reconstruction and radiation therapy. Int J Radiat Oncol Biol Phys. 59:1080–1087. DOI: 10.1016/j.ijrobp.2003.12.036. PMID: 15234042.
Article17. Park JM, Lee J, Kim HS, Ye SJ, Kim JI. 2014; Development of an applicator for eye lens dosimetry during radiotherapy. Br J Radiol. 87:20140311. DOI: 10.1259/bjr.20140311. PMID: 25111733. PMCID: PMC4170865.
Article18. Park JM, Son J, An HJ, Kim JH, Wu HG, Kim JI. 2019; Bio-compatible patient-specific elastic bolus for clinical implementation. Phys Med Biol. 64:105006. DOI: 10.1088/1361-6560/ab1c93. PMID: 31022714.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corrigendum: Assessing Commercial CLEANBOLUS Based on Silicone for Clinical Use
- Evaluations of a Commercial CLEANBOLUS-WHITE for Clinical Application
- A Case of Hyperoleon
- Comparison of Satisfaction Levels between Conventional and Silicone-Adhesive Polyurethane Foam Materials in Patients with Skin Wounds
- A Case of Silicone Rubber-Induced Foreign Body Granuloma with Skin Defect