Pediatr Emerg Med J.
2021 Dec;8(2):81-86. 10.22470/pemj.2021.00360.
Point-of-care lactate: a predictor of emergency medicine resource use and outcomes in infants with diarrhea
- Affiliations
-
- 1Department of Emergency Medicine, Soonchunhyang University College of Medicine, Cheonan, Korea
- KMID: 2523999
- DOI: http://doi.org/10.22470/pemj.2021.00360
Abstract
- Purpose
Fluid therapy for diarrhea-induced dehydration inadvertently increases emergency department length of stay (EDLOS). To prevent this delay, we investigated the usefulness of triage using point-of-care (POC) lactate in infants with diarrhea.
Methods
This study was performed on infants with diarrhea who visited the emergency department from January 2019 through December 2020. According to the POC lactate concentration and the Korean Triage and Acuity Scale (KTAS) level, the infants were separately divided into the low (< 2 mmol/L), moderate (2-3.9), and high (≥ 4) lactate groups and the mild (KTAS 4-5) and severe (1-3) groups, respectively. Using these 2 group designations, we compared variables regarding the emergency medicine resource use and outcomes. To predict the prolonged EDLOS (≥ median value) we performed logistic regression and receiver operating characteristic analyses.
Results
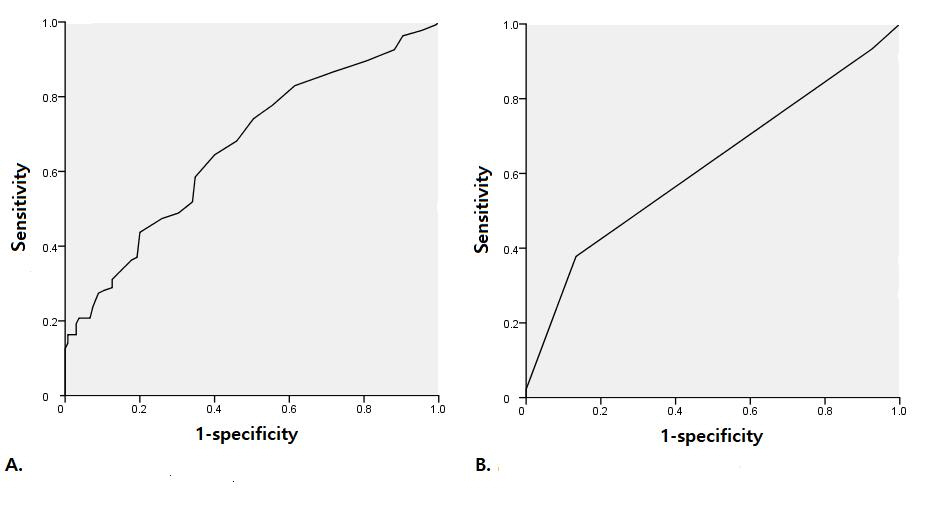
A total of 540 infants were included. The median of EDLOS was 169 minutes (interquartile range, 103-220). Fluid therapy was more frequently performed in the high lactate group than in the low-moderate lactate groups (85.0% vs. 60.4%-73.6%; P = 0.025). The high lactate and severe groups respectively showed higher rates of hospitalization (40.0% vs. 3.8%-7.6% [P < 0.001] and 10.9% vs. 1.4% [P = 0.015]), and longer median EDLOS (259 minutes vs. 147-178 [P < 0.001] and 185 vs. 131 [P = 0.001]) compared to the low-moderate lactate and mild groups. Compared to the KTAS, lactate is more strongly associated with the prolonged EDLOS (lactate, adjusted odds ratio, 4.80 [95% confidence interval, 1.87-15.34] vs. KTAS, 3.52 [1.90-6.54]). The areas under curve for lactate and for the KTAS were 0.66 (0.60-0.73) and 0.62 (0.55-0.69), respectively (P = 0.058).
Conclusion
In infants with diarrhea, POC lactate can be a predictor of emergency medicine resource use and outcomes.
Keyword
Figure
Reference
-
References
1. Dekate P, Jayashree M, Singhi SC. Management of acute diarrhea in emergency room. Indian J Pediatr. 2013; 80:235–46.
Article2. Denno DM, Shaikh N, Stapp JR, Qin X, Hutter CM, Hoffman V, et al. Diarrhea etiology in a pediatric emergency department: a case control study. Clin Infect Dis. 2012; 55:897–904.
Article3. Doan Q, Wong H, Meckler G, Johnson D, Stang A, Dixon A. The impact of pediatric emergency department crowding on patient and health care system outcomes: a multicentre cohort study. CMAJ. 2019; 191:E627–35.
Article4. Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ. 2011; 342:d2983.
Article5. Park J, Lim T. Korean Triage and Acuity Scale (KTAS). J Korean Soc Emerg Med. 2017; 28:547–51. Korean.6. Fukumoto Y, Inoue Y, Takeuchi Y, Hoshino T, Nakamura Y, Ishikawa K, et al. Utility of blood lactate level in triage. Acute Med Surg. 2015; 3:101–6.
Article7. Goyal M, Pines JM, Drumheller BC, Gaieski DF. Point-of-care testing at triage decreases time to lactate level in septic patients. J Emerg Med. 2010; 38:578–81.
Article8. Consoli A, Nurjhan N, Reilly JJ Jr, Bier DM, Gerich JE. Contribution of liver and skeletal muscle to alanine and lactate metabolism in humans. Am J Physiol. 1990; 259(5 Pt 1):E677–84.
Article9. van Hall G. Lactate kinetics in human tissues at rest and during exercise. Acta Physiol (Oxf). 2010; 199:499–508.
Article10. Connor H, Woods HF, Ledingham JG, Murray JD. A model of L(+)-lactate metabolism in normal man. Ann Nutr Metab. 1982; 26:254–63.
Article11. Fu YQ, Bai K, Liu CJ. The impact of admission serum lactate on children with moderate to severe traumatic brain injury. PLoS One. 2019; 14:e0222591.
Article12. Miescier MJ, Lane RD, Sheng X, Larsen GY. Association between initial emergency department lactate and use of vasoactive medication in children with septic shock. Pediatr Emerg Care. 2019; 35:455–60.
Article13. Shah A, Guyette F, Suffoletto B, Schultz B, Quintero J, Predis E, et al. Diagnostic accuracy of a single point-of-care prehospital serum lactate for predicting outcomes in pediatric trauma patients. Pediatr Emerg Care. 2013; 29:715–9.
Article14. Huh Y, Ko Y, Hwang K, Jung K, Cha YH, Choi YJ, et al. Admission lactate and base deficit in predicting outcomes of pediatric trauma. Shock. 2021; 55:495–500.
Article15. Green NA, Durani Y, Brecher D, DePiero A, Loiselle J, Attia M. Emergency Severity Index version 4: a valid and reliable tool in pediatric emergency department triage. Pediatr Emerg Care. 2012; 28:753–7.16. Kraut JA, Madias NE. Lactic acidosis. N Engl J Med. 2014; 371:2309–19.
Article17. Levy B, Desebbe O, Montemont C, Gibot S. Increased aerobic glycolysis through beta2 stimulation is a common mechanism involved in lactate formation during shock states. Shock. 2008; 30:417–21.18. Atherly-John YC, Cunningham SJ, Crain EF. A randomized trial of oral vs intravenous rehydration in a pediatric emergency department. Arch Pediatr Adolesc Med. 2002; 156:1240–3.
Article19. Guru V, Dubinsky I. The patient vs. caregiver perception of acute pain in the emergency department. J Emerg Med. 2000; 18:7–12.
Article20. Lee JH, Park YS, Park IC, Lee HS, Kim JH, Park JM, et al. Over-triage occurs when considering the patient's pain in Korean Triage and Acuity Scale (KTAS). PLoS One. 2019; 14:e0216519.
Article21. Singer AJ, Taylor M, LeBlanc D, Meyers K, Perez K, Thode HC Jr, et al. Early point-of-care testing at triage reduces care time in stable adult emergency department patients. J Emerg Med. 2018; 55:172–8.
Article22. Ma C, Gunaratnam LC, Ericson A, Conroy AL, Namasopo S, Opoka RO, et al. Handheld point-of-care lactate measurement at admission predicts mortality in Ugandan children hospitalized with pneumonia: a prospective cohort study. Am J Trop Med Hyg. 2019; 100:37–42.
Article23. Kim JA, Son MH, Park M. Effect of coronavirus disease 2019 on febrile children’s visits to the emergency department of a tertiary hospital. Pediatr Emerg Med J. 2021; 8:8–15.
Article24. Bellini T, Piccotti E. A potential impact of the donning and doffing policy on emergency department length of stay during the coronavirus disease 2019 pandemic. Pediatr Emerg Med J. 2021 Apr 19 [Epub]. https://doi.org/10.22470/pemj.2021.00227.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of ethylene glycol poisoning accompanied by a lactate gap between analyzing methods
- Association of lactate clearance with outcomes of patients with gastrointestinal bleeding visiting the emergency department
- Health Problems and Health Services Utilization of Infants Born Prematurely in the U.S.
- The usefulness of lactate as an early predictor of the severity of emergency department patients with postpartum hemorrhage
- Utility of lactate measurement in the diagnosis of serious bacterial infection in young infants