J Korean Neurosurg Soc.
2022 Jan;65(1):49-56. 10.3340/jkns.2021.0005.
Spinal Angiolipomas : Clinical Characteristics, Surgical Strategies and Prognosis
- Affiliations
-
- 1Department of Neurosurgery, Beijing Tsinghua Changgung Hospital, School of Clinical Medicine, Tsinghua University, Beijing, China
- KMID: 2523913
- DOI: http://doi.org/10.3340/jkns.2021.0005
Abstract
Objective
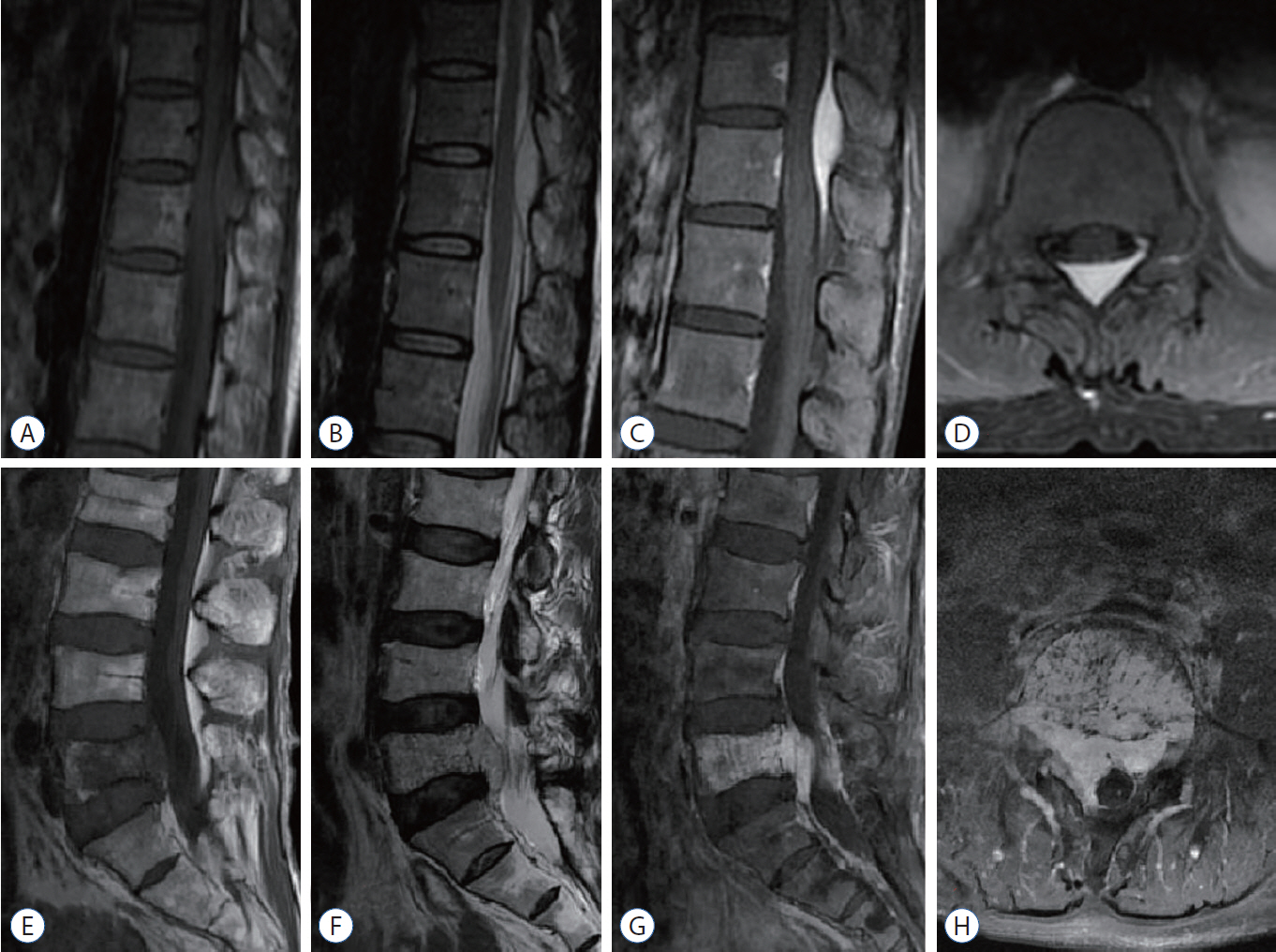
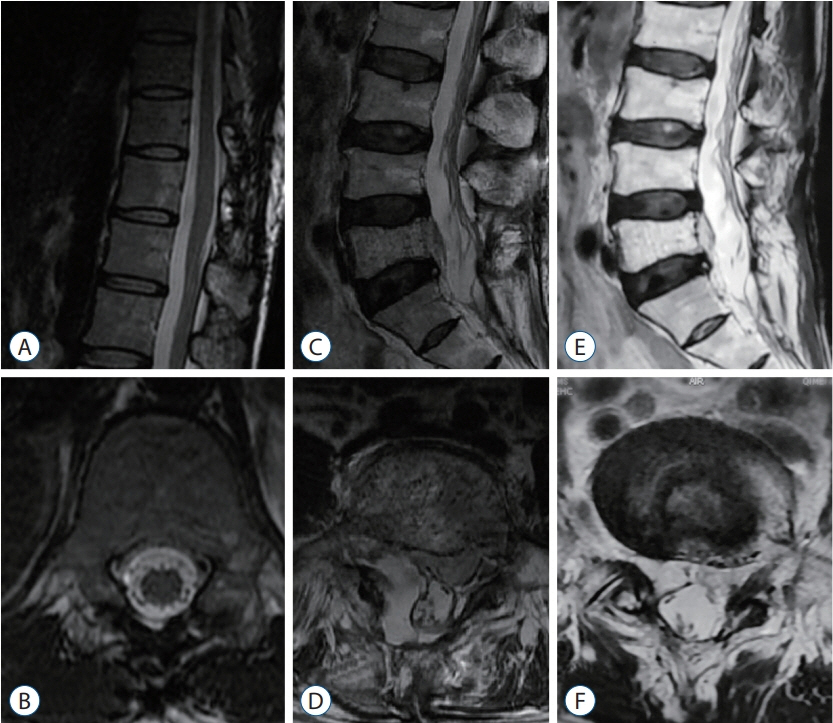
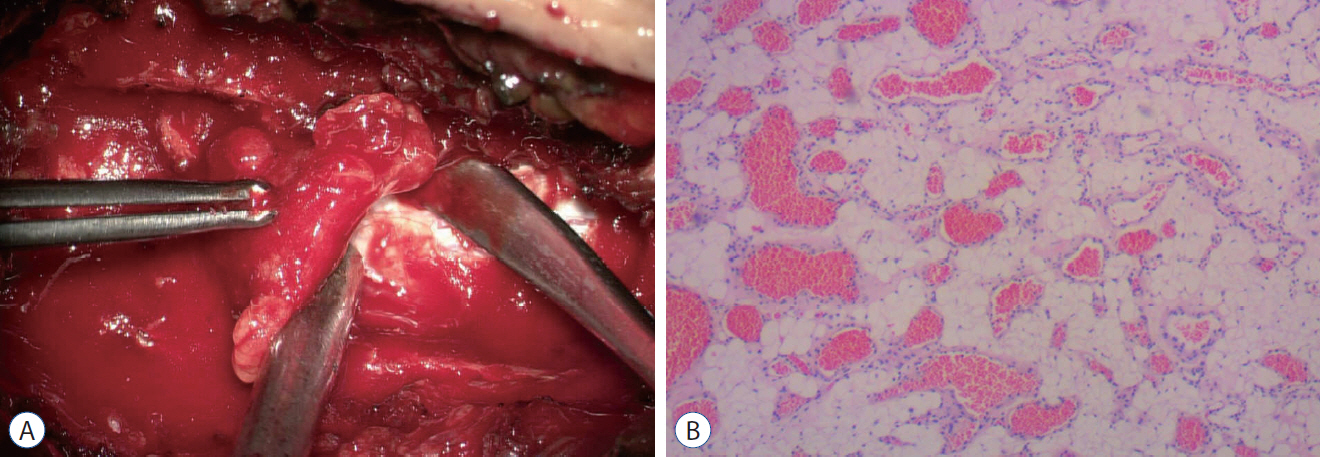
: Angiolipomas are usually found in the subcutaneous tissue of the trunk and limbs. Spinal angiolipomas (SALs) are uncommon and have rarely been reported. We report a series of nine SALs patients who received surgical treatment in our department. To summarize the clinical characteristics of SALs, propose our surgical strategies, and evaluate the effects of the operation.
Methods
: This was a retrospective review of nine SALs patients who received surgical treatment from August 2015 to March 2020. Total or subtotal resection was determined by the axial localization (dorsal or ventral) and the extent of intervertebral foramen involvement. The outcomes were assessed based on the modified Japanese Orthopaedic Association (mJOA) scoring system utilized before surgery and at various follow-up points.
Results
: Among the nine patients, the mean mJOA score before surgery was 6.6±2.3, compared with 10.1±1.1 at the last follow-up time point (33.4±11.8 months). All patients achieved good outcomes, even in cases of subtotal resection.
Conclusion
: Early surgical resection of SALs is recommended, and the specific procedures should be determined by the axial localization (dorsal or ventral) and the extent of intervertebral foramen involvement. Most of the patients had a good prognosis, even in cases of subtotal resection.
Keyword
Figure
Reference
-
References
1. Anson JA, Cybulski GR, Reyes M. Spinal extradural angiolipoma: a report of two cases and review of the literature. Surg Neurol. 34:173–178. 1990.
Article2. Bender JL, Van Landingham JH, Manno NJ. Epidural lipoma producing spinal cord compression. Report of two cases. J Neurosurg. 41:100–103. 1974.3. Bouali S, Maatar N, Bouhoula A, Abderrahmen K, Said IB, Boubaker A, et al. Spinal epidural angiolipomas: clinical characteristics, management and outcomes. Asian J Neurosurg. 11:348–351. 2016.
Article4. Fourney DR, Tong KA, Macaulay RJ, Griebel RW. Spinal angiolipoma. Can J Neurol Sci. 28:82–88. 2001.
Article5. Garg A, Gupta V, Gaikwad S, Deol P, Mishra NK, Sharma MC, et al. Spinal angiolipoma: report of three cases and review of MRI features. Australas Radiol. 46:84–90. 2002.
Article6. Gelabert-González M, García-Allut A. Spinal extradural angiolipoma: report of two cases and review of the literature. Eur Spine J. 18:324–335. 2009.
Article7. Groen RJ. Non-operative treatment of spontaneous spinal epidural hematomas: a review of the literature and a comparison with operative cases. Acta Neurochir (Wien). 146:103–110. 2004.
Article8. Guegan Y, Fardoun R, Launois B, Pecker J. Spinal cord compression by extradural fat after prolonged corticosteroid therapy. J Neurosurg. 56:267–269. 1982.
Article9. Han SR, Yee GT, Choi CY, Lee CH. Infiltrating spinal angiolipoma. J Korean Neurosurg Soc. 52:161–163. 2012.
Article10. Howard WR, Helwig EB. Angiolipoma. Arch Dermatol. 82:924–931. 1960.
Article11. Hu S, Hu CH, Hu XY, Wang XM, Dai H, Fang XM, et al. MRI features of spinal epidural angiolipomas. Korean J Radiol. 14:810–817. 2013.
Article12. Kujas M, Lopes M, Lalam TF, Fohanno D, Poirier J. Infiltrating extradural spinal angiolipoma. Clin Neuropathol. 18:93–98. 1999.13. Labram EK, el-Shunnar K, Hilton DA, Robertson NJ. Revisited: spinal angiolipoma--three additional cases. Br J Neurosurg. 13:25–9. 1999.
Article14. Leu NH, Chen CY, Shy CG, Lu CY, Wu CS, Chen DC, et al. MR imaging of an infiltrating spinal epidural angiolipoma. AJNR Am J Neuroradiol. 24:1008–1011. 2003.15. Lin JJ, Lin F. Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma. Cancer. 34:720–727. 1974.
Article16. Nadi MM, Nadi AM, Zabara MY, Ahmad TM. Management of infiltrating spinal epidural angiolipoma. Neurosciences (Riyadh). 20:159–163. 2015.
Article17. O’Donovan NA, Naik K, Maloney WJ, Llewellyn CG. Spinal angiolipoma mimicking extradural lipomatosis. Can Assoc Radiol J. 47:51–53. 1996.18. Pagni CA, Canavero S. Spinal epidural angiolipoma: rare or unreported? Neurosurgery. 31:758–764. discussion 764. 1992.19. Preul MC, Leblanc R, Tampieri D, Robitaille Y, Pokrupa R. Spinal angiolipomas. Report of three cases. J Neurosurg. 78:280–286. 1993.20. Provenzale JM, McLendon RE. Spinal angiolipomas: MR features. AJNR Am J Neuroradiol. 17:713–719. 1996.21. Reyes D, Candocia FJ. Thoracolumbar spinal angiolipoma demonstrating high signal on STIR imaging: a case report and review of the literature. Spine J. 13:e1–e5. 2013.
Article22. Rocchi G, Caroli E, Frati A, Cimatti M, Savlati M. Lumbar spinal angiolipomas: report of two cases and review of the literature. Spinal Cord. 42:313–316. 2004.
Article23. Samdani AF, Garonzik IM, Jallo G, Eberhart CG, Zahos P. Spinal angiolipoma: case report and review of the literature. Acta Neurochir (Wien). 146:299–302. discussion 302. 2004.
Article24. Si Y, Wang Z, Pan Y, Lin G, Yu T. Spinal angiolipoma: etiology, imaging findings, classification, treatment, and prognosis. Eur Spine J. 23:417–425. 2014.
Article25. Sim K, Tsui A, Paldor I, Kaye AH, Gaillard F. Four cases of spinal epidural angiolipoma. J Clin Neurosci. 25:134–139. 2016.
Article26. Trabulo A, Cerqueira L, Monteiro J, Roque P, Reis FC, Coelho MR. Spinal angiolipomas revisited: two case reports. Acta Neurochir (Wien). 138:1311–1319. 1996.
Article27. Tsutsumi S, Nonaka Y, Abe Y, Yasumoto Y, Ito M. Spinal angiolipoma in a pregnant woman presenting with acute epidural hemorrhage. J Clin Neurosci. 18:849–851. 2011.
Article28. Turgut M. Spinal angiolipomas: report of a case and review of the cases published since the discovery of the tumour in 1890. Br J Neurosurg. 13:30–40. 1999.
Article29. Wang B, Yang Z, Yang J, Wang G, Xu Y, Liu P. Spinal angiolipoma: experience of twelve patients and literature. Neurol India. 62:367–370. 2014.
Article30. Zhang X, Wang JJ, Guo Y, Dong S, Shi W, Wang G, et al. Sudden aggravated radicular pain caused by hemorrhagic spinal angiolipomas after back massage. World Neurosurg. 134:383–387. 2020.
Article