J Cerebrovasc Endovasc Neurosurg.
2021 Dec;23(4):365-371. 10.7461/jcen.2021.E2020.12.004.
Isolated clival subdural haemorrhage from a dolicoectactic vertebrobasilar aneurysm: Case report and overview of endovascular treatment strategies
- Affiliations
-
- 1Interventional Neuroradiology, Queens Medical Centre, Nottingham University Hospitals NHS Trust, Nottingham, United Kingdom
- KMID: 2523896
- DOI: http://doi.org/10.7461/jcen.2021.E2020.12.004
Abstract
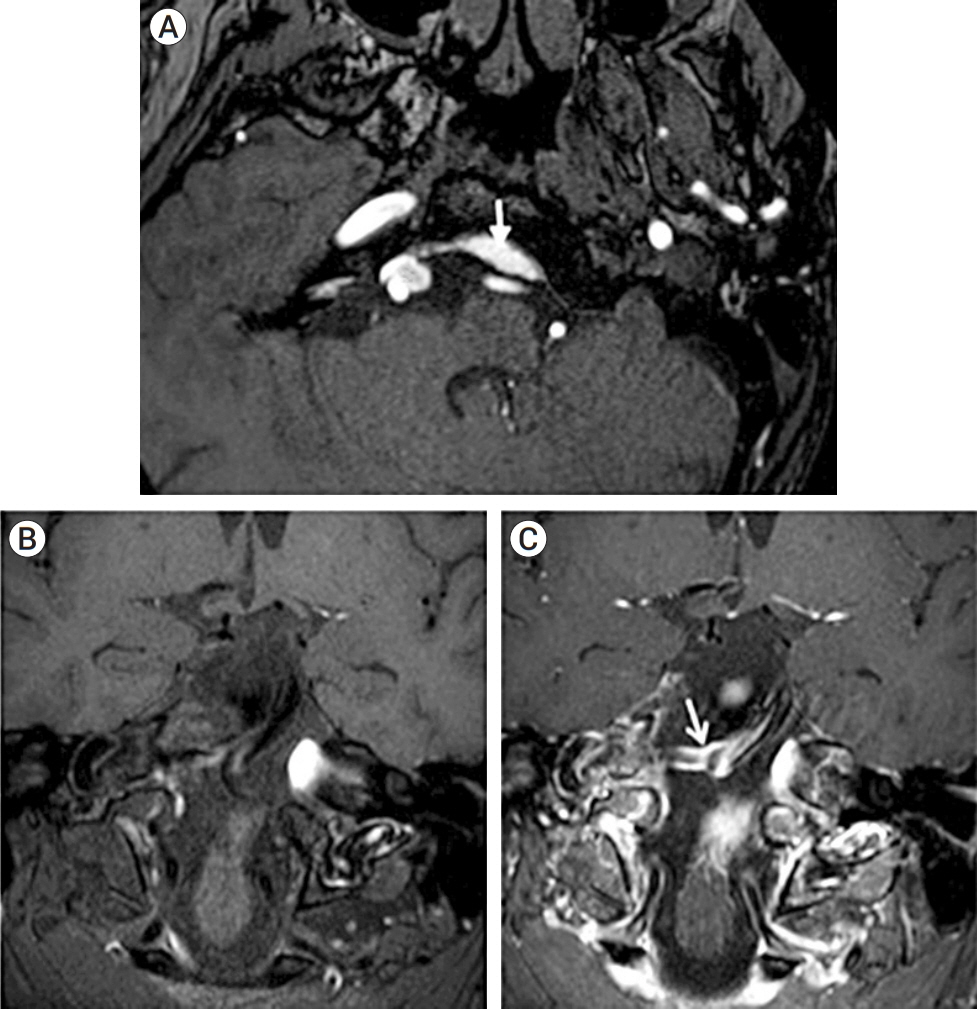
- Posterior fossa aneurysms presenting with isolated subdural haemorrhage (SDH) have scarcely been described with no cases attributed to a vertebrobasilar (VB) location. Non-saccular VB aneurysms are a distinct sub-group and in this report we also discuss the pathophysiology and treatment options for these difficult-to-manage lesions. We present a case of a 49 year-old man who presented with a 7-day history of severe headaches who was found to have an isolated acute clival SDH. Vascular imaging revealed a VB dolicoectatic segment with superimposed fusiform dilatations that contacted the dura adjacent to the SDH. A staged treatment was performed with initial parental vessel occlusion of the ruptured vertebral artery segment and subsequent insertion of a braided stent (LEO) with flow diverting properties into the progressively dilating basilar artery. A third procedure was performed to occlude a recurrent pouch at the lower basilar dilatation. Complete angiographic occlusion was achieved and the patient is under continued surveillance. To our knowledge, this is the first case of a ruptured non-saccular VB aneurysm presenting with radiologically isolated clival SDH. Clinical history will often inform the need for vascular imaging in such atypical presentations. Managing these lesions remains an endovascular challenge and requires a specialist multi-disciplinary approach.
Figure
Reference
-
1. Anik I, Ceylan S, Koc K, Tugasaygi M, Sirin G, Gazioglu N, Sam B. Microsurgical and endoscopic anatomy of Liliequist’s membrane and the prepontine membranes: cadaveric study and clinical implications. Acta Neurochir (Wien). 2011; Aug. 153(8):1701–11.
Article2. Awad AJ, Mascitelli JR, Haroun RR, De Leacy RA, Fifi JT, Mocco J. Endovascular management of fusiform aneurysms in the posterior circulation: the era of flow diversion. Neurosurg Focus. 2017; Jun. 42(6):E14.
Article3. Biesbroek JM, Rinkel GJE, Algra A, van der Sprenkel JWB. Risk factors for acute subdural hematoma from intracranial aneurysm rupture. Neurosurgery. 2012; Aug. 71(2):264–8. discussion 268.
Article4. Cagnazzo F, di Carlo DT, Cappucci M, Lefevre PH, Costalat V, Perrini P. Acutely ruptured intracranial aneurysms treated with flow-diverter stents: a systematic review and meta-analysis. Am J Neuroradiol. 2018; Sep. 39(9):1669–75.
Article5. Caton MT, Wiggins WF, Nuñez D. Non-traumatic subdural hemorrhage: beware of ruptured intracranial aneurysm. Emergency Radiology. 2019; Oct. 26(5):567–71.
Article6. Flemming KD, Wiebers DO, Brown RD Jr, Link MJ, Huston J 3rd, McClelland RL, et al. The natural history of radiographically defined vertebrobasilar nonsaccular intracranial aneurysms. Cerebrovasc Dis. 2005; 20(4):270–9.
Article7. He X, Duan C, Zhang J, Li X, Zhang X, Li Z. The safety and efficacy of using large woven stents to treat vertebrobasilar dolichoectasia. J Neurointerv Surg. 2019; Nov. 11(11):1162–6.
Article8. Kiyofuji S, Graffeo CS, Perry A, Murad MH, Flemming KD, Lanzino G, et al. Meta-analysis of treatment outcomes of posterior circulation non-saccular aneurysms by flow diverters. J Neurointerv Surg. 2018; May. 10(5):493–9.
Article9. Kocak A, Ates O, Durak A, Alkan A, Cayli S, Sarac K. Acute subdural hematomas caused by ruptured aneurysms: experience from a single Turkish center. Turk Neurosurg. 2009; Oct. 19(4):333–7.10. Nasr DM, Flemming KD, Lanzino G, Cloft HJ, Kallmes DF, Murad MH, et al. Natural history of vertebrobasilar dolichoectatic and fusiform aneurysms: a systematic review and meta-analysis. Cerebrovascular Diseases. 2018; 45(1-2):68–77.
Article11. San Millan Ruiz D, Yilmaz H, Dehdashti AR, Alimenti A, de Tribolet N, Rufenacht DA. The perianeurysmal environment: influence on saccular aneurysm shape and rupture. Am J Neuroradiol. 2006; 27(3):504–12.12. Shapiro M, Becske T, Riina HA, Raz E, Zumofen D, Nelson PK. Non-saccular vertebrobasilar aneurysms and dolichoectasia: a systematic literature review. J Neurointerv Surg. 2014; Jun. 6(5):389–93.
Article13. Sonmez O, Brinjikji W, Murad MH, Lanzino G. Deconstructive and reconstructive techniques in treatment of vertebrobasilar dissecting aneurysms: a systematic review and meta-analysis. Am J Neuroradiol. 2015; Jul. 36(7):1293–8.
Article14. Verhey LH, Wang W, Adel JG. True cortical saccular aneurysm presenting as an acute subdural hematoma. World Neurosurgery. 2018; May. 113:58–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Traumatic Entrapment of the Vertebrobasilar Junction Due to a Longitudinal Clival Fracture: A Case Report
- Treatment of a Ruptured Vertebrobasilar Fusiform Aneurysm Using Pipeline Embolization Device
- Subdural Hematoma Due to Ruptured Intracerebral Aneurysm
- Delayed Aneurysm Rupture Following Endovascular Treatment with Contour Device: A Case Report
- Endovascular Coiling of Fenestrated Vertebrobasilar Cerebral Aneurysms