Ann Rehabil Med.
2021 Dec;45(6):450-458. 10.5535/arm.21161.
Utilizing Pulmonary Function Parameters to Predict Dysphagia in Individuals With Cervical Spinal Cord Injuries
- Affiliations
-
- 1Department of Rehabilitation Medicine, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- KMID: 2523842
- DOI: http://doi.org/10.5535/arm.21161
Abstract
Objective
To utilize pulmonary function parameters as predictive factors for dysphagia in individuals with cervical spinal cord injuries (CSCIs).
Methods
Medical records of 78 individuals with CSCIs were retrospectively reviewed. The pulmonary function was evaluated using spirometry and peak flow meter, whereas the swallowing function was assessed using a videofluoroscopic swallowing study. Participants were divided into the non-penetration-aspiration group (score 1 on the Penetration-Aspiration Scale [PAS]) and penetration-aspiration group (scores 2–8 on the PAS). Individuals with pharyngeal residue grade scores >1 were included in the pharyngeal residue group.
Results
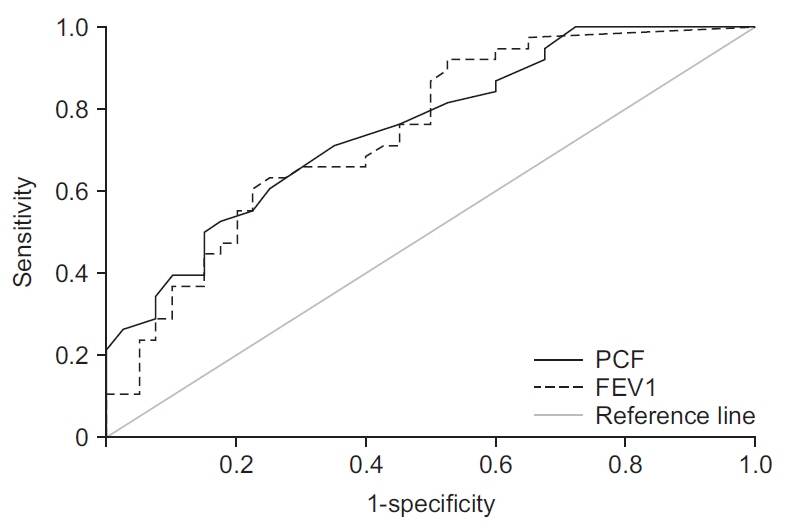
The mean age was significantly higher in the penetration-aspiration and pharyngeal residue groups. In this study, individuals with clinical features, such as advanced age, history of tracheostomy, anterior surgical approach, and higher neurological level of injury, had significantly more penetration-aspiration or pharyngeal residue. Individuals in the penetration-aspiration group had significantly lower peak cough flow (PCF) levels. Individuals in the pharyngeal residue group had a significantly lower forced expiratory volume in 1 second (FEV1). According to the receiver operating characteristic curve analysis of PCF and FEV1 on the PAS, the cutoff value was 140 L/min and 37.5% of the predicted value, respectively.
Conclusion
Low PCF and FEV1 values may predict the risk of dysphagia in individuals with CSCIs. In these individuals, active evaluation of swallowing is recommended to confirm dysphagia.
Figure
Reference
-
1. Kirshblum S, Johnston MV, Brown J, O’Connor KC, Jarosz P. Predictors of dysphagia after spinal cord injury. Arch Phys Med Rehabil. 1999; 80:1101–5.
Article2. Wolf C, Meiners TH. Dysphagia in patients with acute cervical spinal cord injury. Spinal Cord. 2003; 41:347–53.
Article3. Brady S, Miserendino R, Statkus D, Springer T, Hakel M, Stambolis V. Predictors to dysphagia and recovery after cervical spinal cord injury during acute rehabilitation. J Appl Res Clin Exp Ther. 2004; 4:1–11.4. Abel R, Ruf S, Spahn B. Cervical spinal cord injury and deglutition disorders. Dysphagia. 2004; 19:87–94.
Article5. Chaw E, Shem K, Castillo K, Wong SL, Chang J. Dysphagia and associated respiratory considerations in cervical spinal cord injury. Top Spinal Cord Inj Rehabil. 2012; 18:291–9.
Article6. Zakrasek EC, Nielson JL, Kosarchuk JJ, Crew JD, Ferguson AR, McKenna SL. Pulmonary outcomes following specialized respiratory management for acute cervical spinal cord injury: a retrospective analysis. Spinal Cord. 2017; 55:559–65.
Article7. DiBardino DM, Wunderink RG. Aspiration pneumonia: a review of modern trends. J Crit Care. 2015; 30:40–8.
Article8. Shin JC, Yoo JH, Lee YS, Goo HR, Kim DH. Dysphagia in cervical spinal cord injury. Spinal Cord. 2011; 49:1008–13.
Article9. Iruthayarajah J, McIntyre A, Mirkowski M, Welch-West P, Loh E, Teasell R. Risk factors for dysphagia after a spinal cord injury: a systematic review and meta-analysis. Spinal Cord. 2018; 56:1116–23.
Article10. Hayashi T, Fujiwara Y, Sakai H, Kubota K, Kawano O, Mori E, et al. The time course of dysphagia following traumatic cervical spinal cord injury: a prospective cohort study. Spinal Cord. 2020; 58:53–7.
Article11. Park JW, Sim GJ, Yang DC, Lee KH, Chang JH, Nam KY, et al. Increased bolus volume effect on delayed pharyngeal swallowing response in post-stroke oropharyngeal dysphagia: a pilot study. Ann Rehabil Med. 2016; 40:1018–23.
Article12. Grossman RG, Frankowski RF, Burau KD, Toups EG, Crommett JW, Johnson MM, et al. Incidence and severity of acute complications after spinal cord injury. J Neurosurg Spine. 2012; 17(1 Suppl):119–28.
Article13. DeVivo MJ, Krause JS, Lammertse DP. Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil. 1999; 80:1411–9.14. Ghannouchi I, Speyer R, Doma K, Cordier R, Verin E. Swallowing function and chronic respiratory diseases: systematic review. Respir Med. 2016; 117:54–64.
Article15. Matsuo K, Palmer JB. Coordination of mastication, swallowing and breathing. Jpn Dent Sci Rev. 2009; 45:31–40.
Article16. Klahn MS, Perlman AL. Temporal and durational patterns associating respiration and swallowing. Dysphagia. 1999; 14:131–8.
Article17. Martin-Harris B, Brodsky MB, Michel Y, Ford CL, Walters B, Heffner J. Breathing and swallowing dynamics across the adult lifespan. Arch Otolaryngol Head Neck Surg. 2005; 131:762–70.
Article18. Min SW, Oh SH, Kim GC, Sim YJ, Kim DK, Jeong HJ. Clinical importance of peak cough flow in dysphagia evaluation of patients diagnosed with ischemic stroke. Ann Rehabil Med. 2018; 42:798–803.
Article19. Lee SJ, Lee KW, Kim SB, Lee JH, Park MK. Voluntary cough and swallowing function characteristics of acute stroke patients based on lesion type. Arch Phys Med Rehabil. 2015; 96:1866–72.
Article20. Palmer JB, Kuhlemeier KV, Tippett DC, Lynch C. A protocol for the videofluorographic swallowing study. Dysphagia. 1993; 8:209–14.
Article21. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–8.
Article22. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–82.
Article23. Cosortium for Spinal Cord Medicine. Respiratory management following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2005; 28:259–93.24. Gassert RB, Pearson WG Jr. Evaluating muscles underlying tongue base retraction in deglutition using muscular functional magnetic resonance imaging (mfMRI). Magn Reson Imaging. 2016; 34:204–8.
Article25. Nguyen JD, Duong H. Anatomy, head and neck, sternohyoid muscle [Internet]. Treasure Island, FL: StatPearls;2021. [cited 2021 Nov 25]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547693/.26. Berlowitz DJ, Wadsworth B, Ross J. Respiratory problems and management in people with spinal cord injury. Breathe (Sheff). 2016; 12:328–40.
Article27. Shem K, Castillo K, Wong S, Chang J. Dysphagia in individuals with tetraplegia: incidence and risk factors. J Spinal Cord Med. 2011; 34:85–92.
Article28. Widdicombe JG, Addington WR, Fontana GA, Stephens RE. Voluntary and reflex cough and the expiration reflex; implications for aspiration after stroke. Pulm Pharmacol Ther. 2011; 24:312–7.
Article29. Smith Hammond CA, Goldstein LB, Zajac DJ, Gray L, Davenport PW, Bolser DC. Assessment of aspiration risk in stroke patients with quantification of voluntary cough. Neurology. 2001; 56:502–6.
Article30. Pitts T, Bolser D, Rosenbek J, Troche M, Sapienza C. Voluntary cough production and swallow dysfunction in Parkinson’s disease. Dysphagia. 2008; 23:297–301.
Article31. Plowman EK, Watts SA, Robison R, Tabor L, Dion C, Gaziano J, et al. Voluntary cough airflow differentiates safe versus unsafe swallowing in amyotrophic lateral sclerosis. Dysphagia. 2016; 31:383–90.
Article32. Kimura Y, Takahashi M, Wada F, Hachisuka K. Differences in the peak cough flow among stroke patients with and without dysphagia. J UOEH. 2013; 35:9–16.
Article33. Hadjikoutis S, Pickersgill TP, Dawson K, Wiles CM. Abnormal patterns of breathing during swallowing in neurological disorders. Brain. 2000; 123(Pt 9):1863–73.
Article34. Park JS, Oh DH, Chang MY, Kim KM. Effects of expiratory muscle strength training on oropharyngeal dysphagia in subacute stroke patients: a randomised controlled trial. J Oral Rehabil. 2016; 43:364–72.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Improvement of Dysphagia after Anterior Cervical Screw Removal: Case Report
- Pulmonary Function in Cervical Spinal Cord Injured Men: Influence of Age and Height
- The Influence of Cervical Spondylosis to Acute Cervical Spinal Cord Injury
- The Significance of Posture on Assessment of Pulmonary Function after Pulmonary Rehabilitation in Tetraplegia
- The Relationship between Spinal Stenosis and Neurological Outcome in Traumatic Cervical Spine Injury: An Analysis using Pavlov's Ratio, Spinal Cord Area, and Spinal Canal Area