J Rheum Dis.
2022 Jan;29(1):46-51. 10.4078/jrd.2022.29.1.46.
Mendelian Randomization Research on the Relationship Between Rheumatoid Arthritis and Systemic Lupus Erythematosus and the Risk of Autistic Spectrum Disorder
- Affiliations
-
- 1Department of Rheumatology, Korea University College of Medicine, Seoul, Korea
- KMID: 2523459
- DOI: http://doi.org/10.4078/jrd.2022.29.1.46
Abstract
Objective
The purpose of this study was to examine whether there is a causal link between rheumatoid arthritis (RA) or systemic lupus erythematosus (SLE) and autism spectrum disorder (ASD).
Methods
We used inverse variance weighted (IVW), weighted median, and MR-Egger regression methods to perform two-sample Mendelian randomization (MR) study using publicly available summary statistics datasets. In addition, we employed genome-wide association studies (GWASs) for RA and SLE as exposure and an ASD GWAS as an outcome.
Results
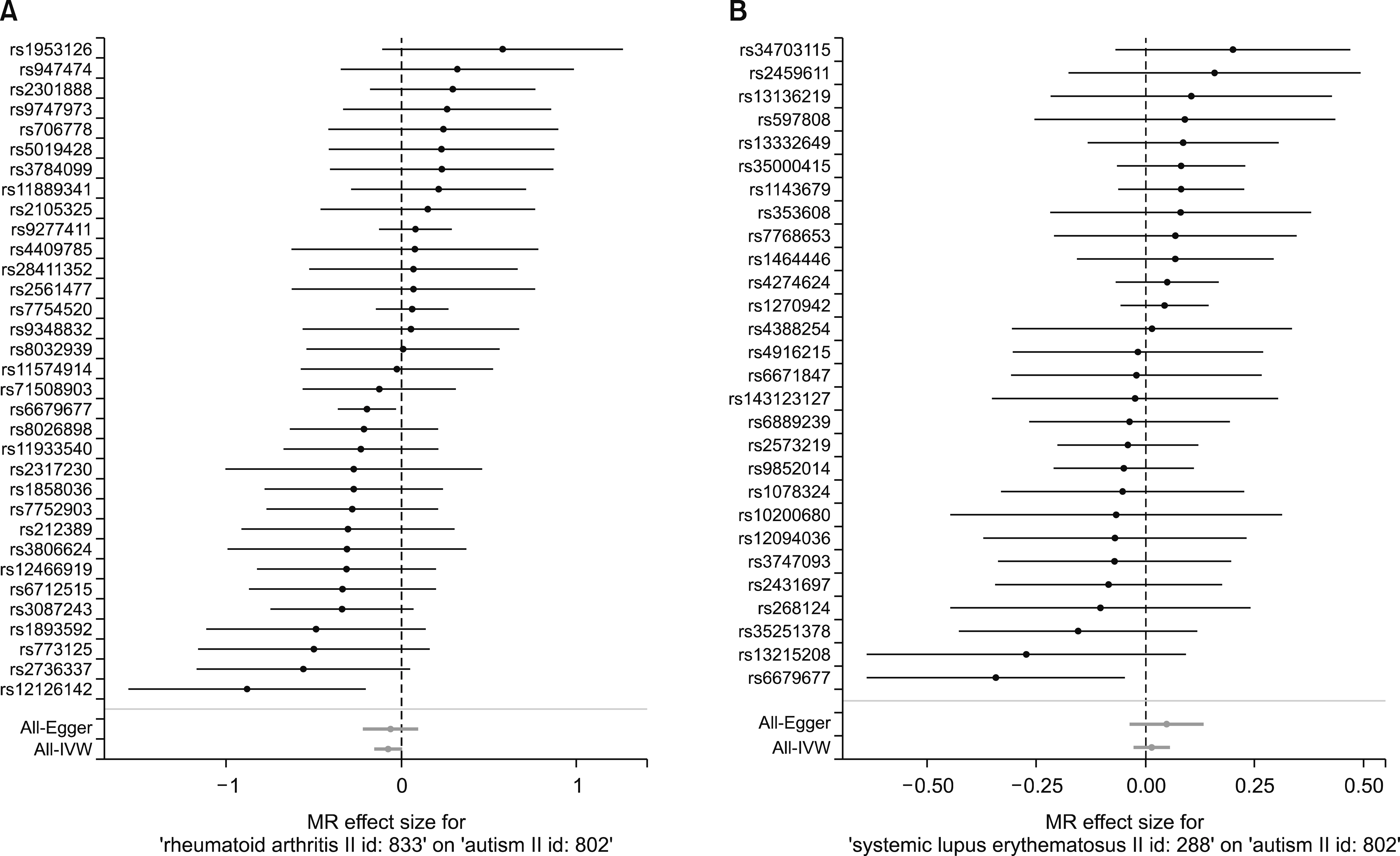
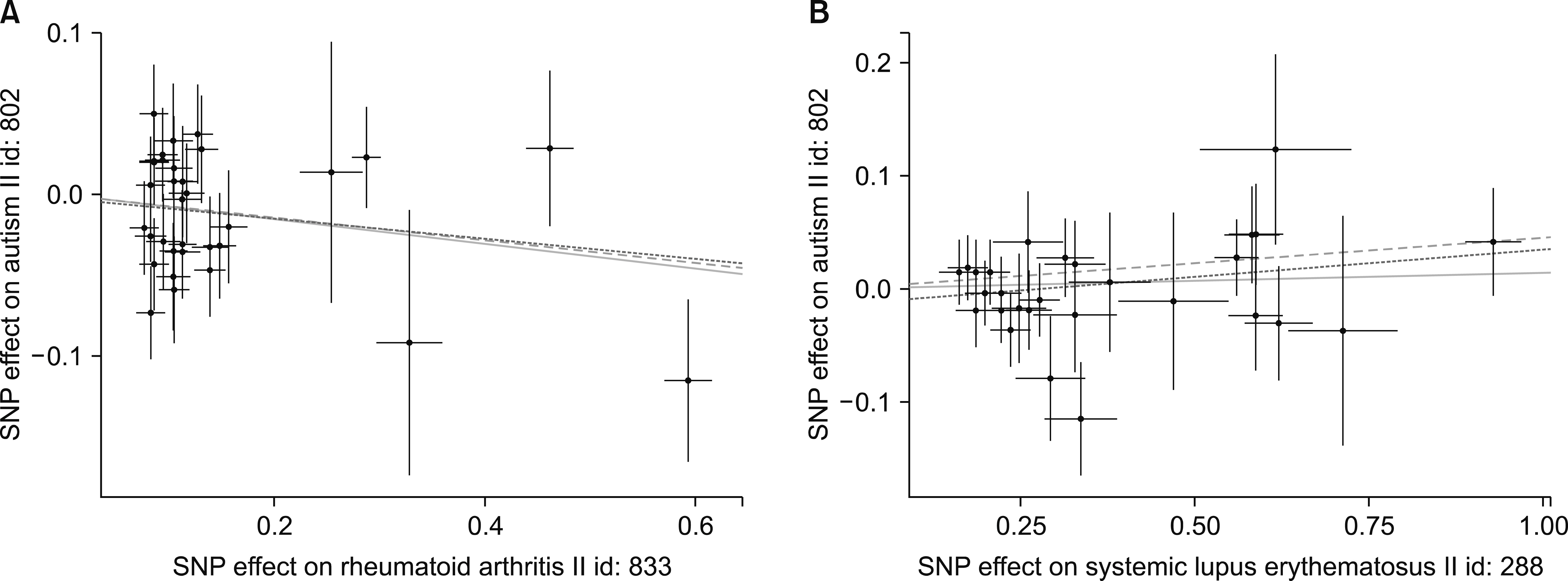
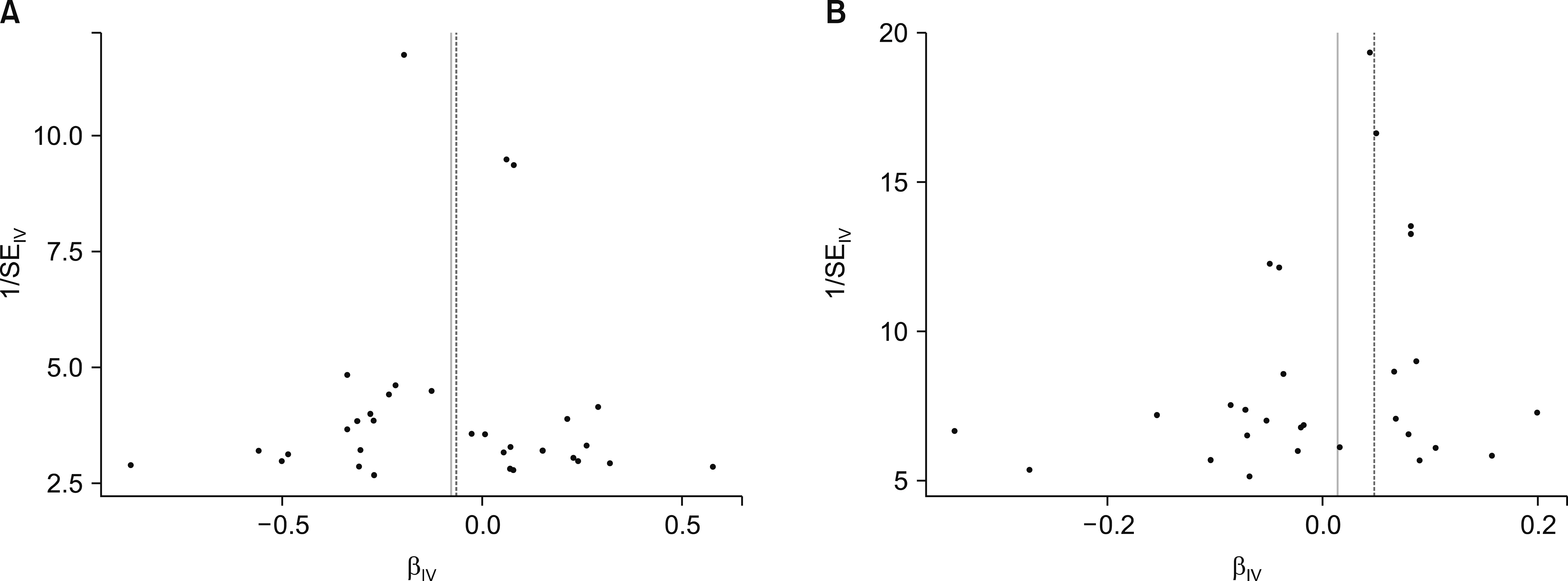
Thirty-three and 28 single-nucleotide polymorphisms from RA and SLE GWASs were selected as instrumental variables for ASD. The IVW method revealed no evidence supporting a causal association between RA and SLE and risk for ASD (beta=−0.077, standard error [SE]=0.041, p=0.062; beta=0.014, SE=0.021, p=0.493). The weighted median approach yielded no evidence of any causal association between RA and SLE and risk for ASD (beta=−0.071, SE=0.058, p=0.223; beta=0.045, SE=0.030, p=0.130). MR-Egger analysis demonstrated no causal association between RA and SLE and risk for ASD (beta=−0.062, SE=0.079, p=0.434; beta=0.048, SE=0.043, p=0.273). The MR results calculated using IVW, the median weighted and the MR-Egger regression approaches were consistent.
Conclusion
The findings of the MR analysis did not support a causal relationship between RA or SLE and the risk of ASD.
Keyword
Figure
Reference
-
1. Lai MC, Lombardo MV, Baron-Cohen S. 2014; Autism. Lancet. 383:896–910. DOI: 10.1016/S0140-6736(13)61539-1.2. Rom AL, Wu CS, Olsen J, Jawaheer D, Hetland ML, Mørch LS. 2018; Parental rheumatoid arthritis and autism spectrum disorders in offspring: a Danish nationwide cohort study. J Am Acad Child Adolesc Psychiatry. 57:28–32.e1. DOI: 10.1016/j.jaac.2017.10.002. PMID: 29301665.3. Keil A, Daniels JL, Forssen U, Hultman C, Cnattingius S, Söderberg KC, et al. 2010; Parental autoimmune diseases associated with autism spectrum disorders in offspring. Epidemiology. 21:805–8. DOI: 10.1097/EDE.0b013e3181f26e3f. PMID: 20798635. PMCID: PMC3115699.4. Wojcik S, Bernatsky S, Platt RW, Pineau CA, Clarke AE, Fombonne É, et al. 2017; Risk of autism spectrum disorders in children born to mothers with rheumatoid arthritis: a systematic literature review. Arthritis Care Res (Hoboken). 69:1926–31. DOI: 10.1002/acr.23235. PMID: 28319657.5. Tsai PH, Yu KH, Chou IJ, Luo SF, Tseng WY, Huang LH, et al. 2018; Risk of autism spectrum disorder in children born to mothers with systemic lupus erythematosus and rheumatoid arthritis in Taiwan. Joint Bone Spine. 85:599–603. DOI: 10.1016/j.jbspin.2017.11.005. PMID: 29183859.6. Zhu Z, Tang S, Deng X, Wang Y. 2020; Maternal systemic lupus erythematosus, rheumatoid arthritis, and risk for autism spectrum disorders in offspring: a meta-analysis. J Autism Dev Disord. 50:2852–9. DOI: 10.1007/s10803-020-04400-y. PMID: 32034648.7. Hill HA, Kleinbaum DG. Armitage P, Colton T, editors. 2000. Bias in observational studies. Encyclopedia of biostatistics. Chichester, John Wiley & Sons.8. Burgess S, Daniel RM, Butterworth AS, Thompson SG. 2015; Network Mendelian randomization: using genetic variants as instrumental variables to investigate mediation in causal pathways. Int J Epidemiol. 44:484–95. DOI: 10.1093/ije/dyu176. PMID: 25150977. PMCID: PMC4469795.9. Lee YH, Song GG. 2019; Causal association between rheumatoid arthritis with the increased risk of type 2 diabetes: a Mendelian randomization analysis. J Rheum Dis. 6:131–6. DOI: 10.4078/jrd.2019.26.2.131.10. Okada Y, Wu D, Trynka G, Raj T, Terao C, Ikari K, et al. 2014; Genetics of rheumatoid arthritis contributes to biology and drug discovery. Nature. 506:376–81. DOI: 10.1038/nature12873. PMID: 24390342. PMCID: PMC3944098.11. Bentham J, Morris DL, Graham DSC, Pinder CL, Tombleson P, Behrens TW, et al. 2015; Genetic association analyses implicate aberrant regulation of innate and adaptive immunity genes in the pathogenesis of systemic lupus erythematosus. Nat Genet. 47:1457–64. DOI: 10.1038/ng.3434. PMID: 26502338. PMCID: PMC4668589.12. Cross-Disorder Group of the Psychiatric Genomics Consortium. 2013; Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 381:1371–9. DOI: 10.1016/S0140-6736(12)62129-1.13. Hartwig FP, Davies NM, Hemani G, Davey Smith G. 2016; Two-sample Mendelian randomization: avoiding the downsides of a powerful, widely applicable but potentially fallible technique. Int J Epidemiol. 45:1717–26. DOI: 10.1093/ije/dyx028. PMID: 28338968. PMCID: PMC5722032.14. Pierce BL, Burgess S. 2013; Efficient design for Mendelian randomization studies: subsample and 2-sample instrumental variable estimators. Am J Epidemiol. 178:1177–84. DOI: 10.1093/aje/kwt084. PMID: 23863760. PMCID: PMC3783091.15. Bowden J, Davey Smith G, Burgess S. 2015; Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 44:512–25. DOI: 10.1093/ije/dyv080. PMID: 26050253. PMCID: PMC4469799.16. Bowden J, Davey Smith G, Haycock PC, Burgess S. 2016; Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 40:304–14. DOI: 10.1002/gepi.21965. PMID: 27061298. PMCID: PMC4849733.17. Hemani G, Zheng J, Wade KH, Laurin C, Elsworth B, Burgess S, et al. 2018. MR-Base: a platform for systematic causal inference across the phenome using billions of genetic associations. BioRxiv. 078972 [Preprint]. https://doi.org/10.1101/78972. cited 2018 May 30.18. Egger M, Smith GD, Phillips AN. 1997; Meta-analysis: principles and procedures. BMJ. 315:1533–7. DOI: 10.1136/bmj.315.7121.1533. PMID: 9432252. PMCID: PMC2127925.19. Chen SW, Zhong XS, Jiang LN, Zheng XY, Xiong YQ, Ma SJ, et al. 2016; Maternal autoimmune diseases and the risk of autism spectrum disorders in offspring: a systematic review and meta-analysis. Behav Brain Res. 296:61–9. DOI: 10.1016/j.bbr.2015.08.035. PMID: 26327239.20. Smith SE, Li J, Garbett K, Mirnics K, Patterson PH. 2007; Maternal immune activation alters fetal brain development through interleukin-6. J Neurosci. 27:10695–702. DOI: 10.1523/JNEUROSCI.2178-07.2007. PMID: 17913903. PMCID: PMC2387067.21. Gata-Garcia A, Diamond B. 2019; Maternal antibody and ASD: clinical data and animal models. Front Immunol. 10:1129. DOI: 10.3389/fimmu.2019.01129. PMID: 31191521. PMCID: PMC6547809.22. Johnson WG, Buyske S, Mars AE, Sreenath M, Stenroos ES, Williams TA, et al. 2009; HLA-DR4 as a risk allele for autism acting in mothers of probands possibly during pregnancy. Arch Pediatr Adolesc Med. 163:542–6. DOI: 10.1001/archpediatrics.2009.74. PMID: 19487610.23. Swerdlow DI, Kuchenbaecker KB, Shah S, Sofat R, Holmes MV, White J, et al. 2016; Selecting instruments for Mendelian randomization in the wake of genome-wide association studies. Int J Epidemiol. 45:1600–16. DOI: 10.1093/ije/dyw088. PMID: 27342221. PMCID: PMC5100611.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adalimumab-induced Lupus Erythematosus Profundus in a Rheumatoid Arthritis Patient
- A Case of Rheumatoid Nodule in a Systemic Lupus Erythematosus Patient
- Sequential Development of Systemic Lupus Erythematosus in a Patient with Juvenile Rheumatoid Arthritis
- H1N1 Influenza Vaccination Response in Rheumatoid Arthritis and Systemic Lupus Erythematosus Patients
- Multiple Eruptive Dermatofibromas in a Patient with Systemic Lupus Erythematosus and Juvenile Rheumatoid Arthritis