Ann Hepatobiliary Pancreat Surg.
2021 Nov;25(4):517-522. 10.14701/ahbps.2021.25.4.517.
Rescue fibrin glue-infiltrating hemostasis combined with hepatorrhaphy to control intractable postoperative bleeding from the liver cut surface
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2523056
- DOI: http://doi.org/10.14701/ahbps.2021.25.4.517
Abstract
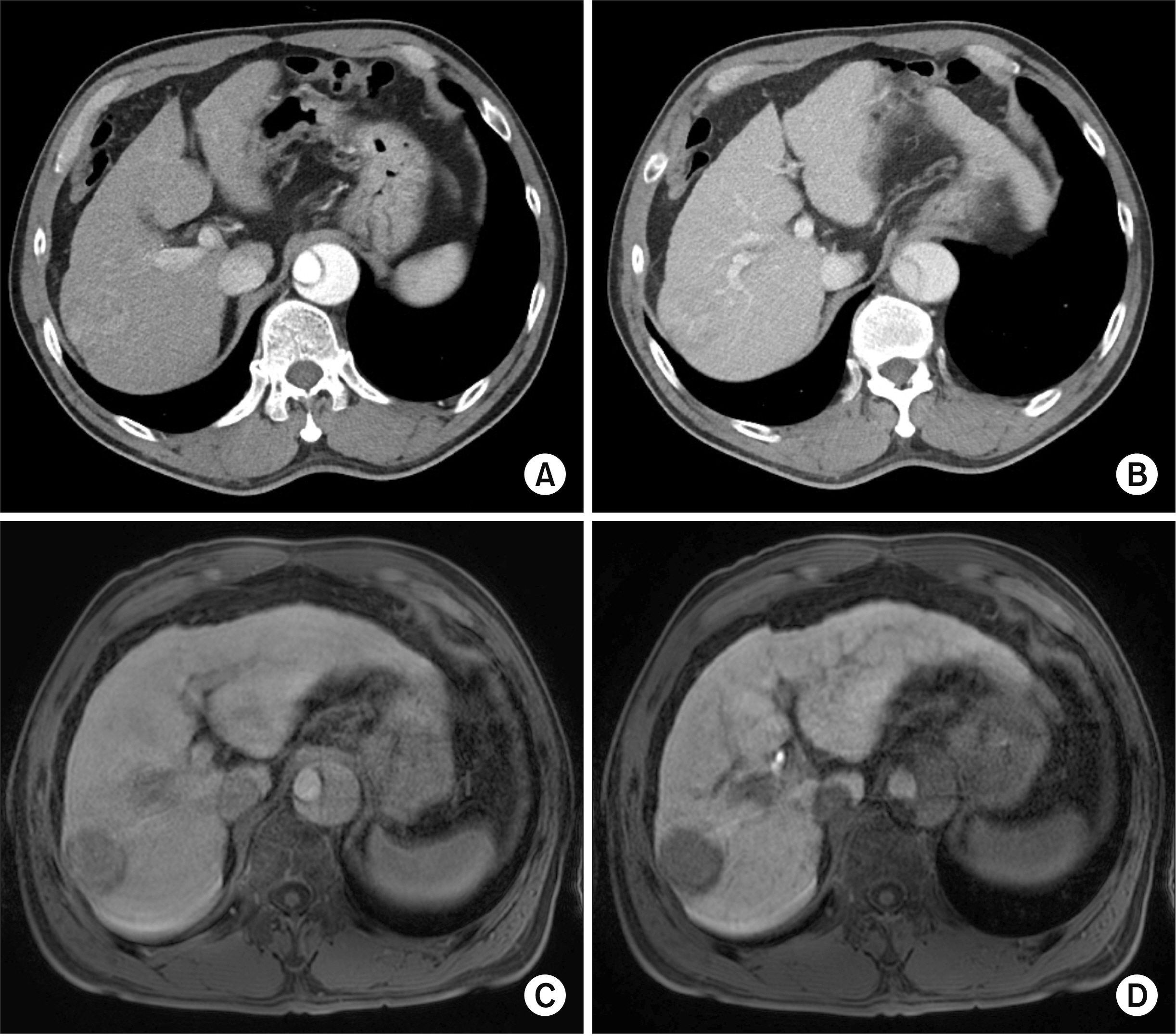
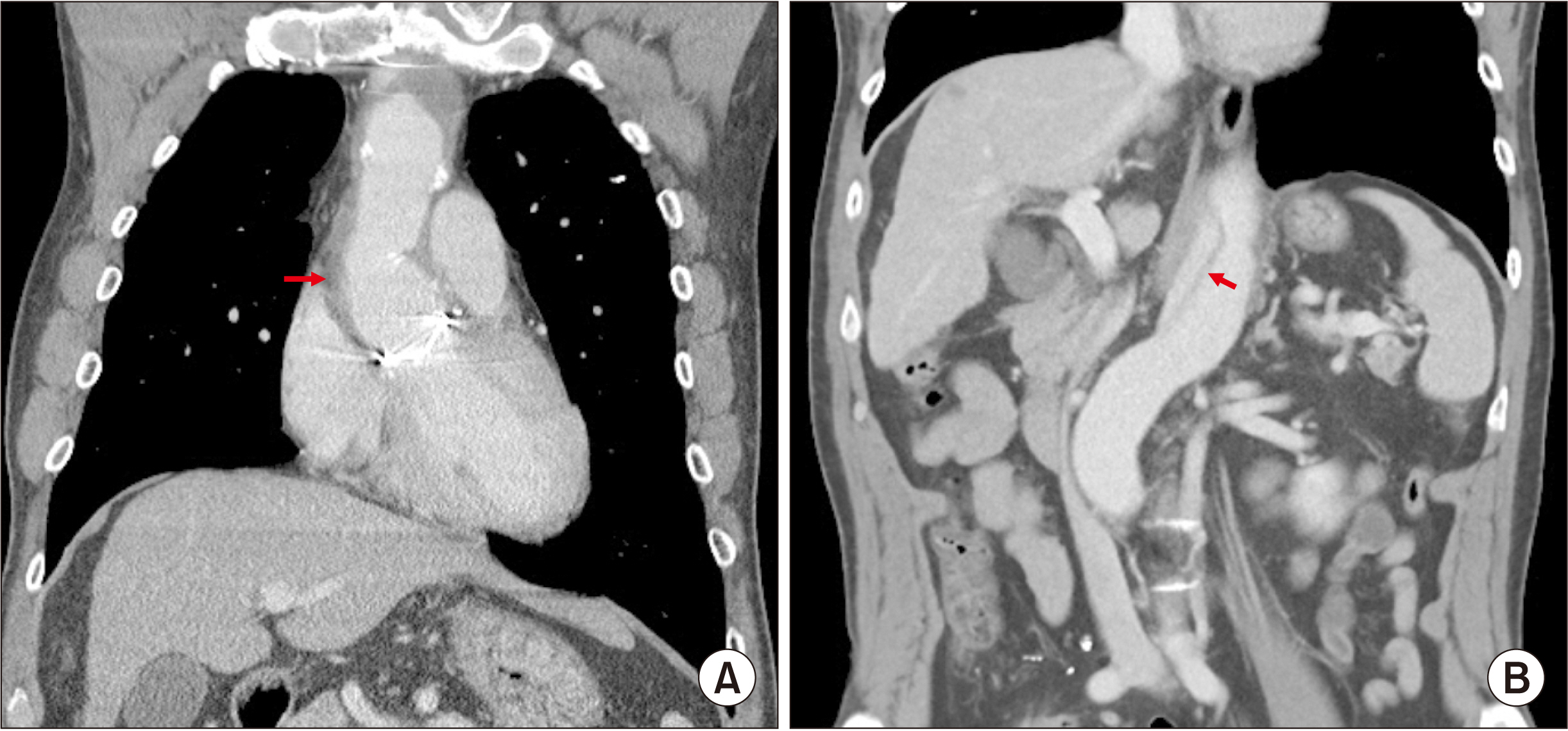
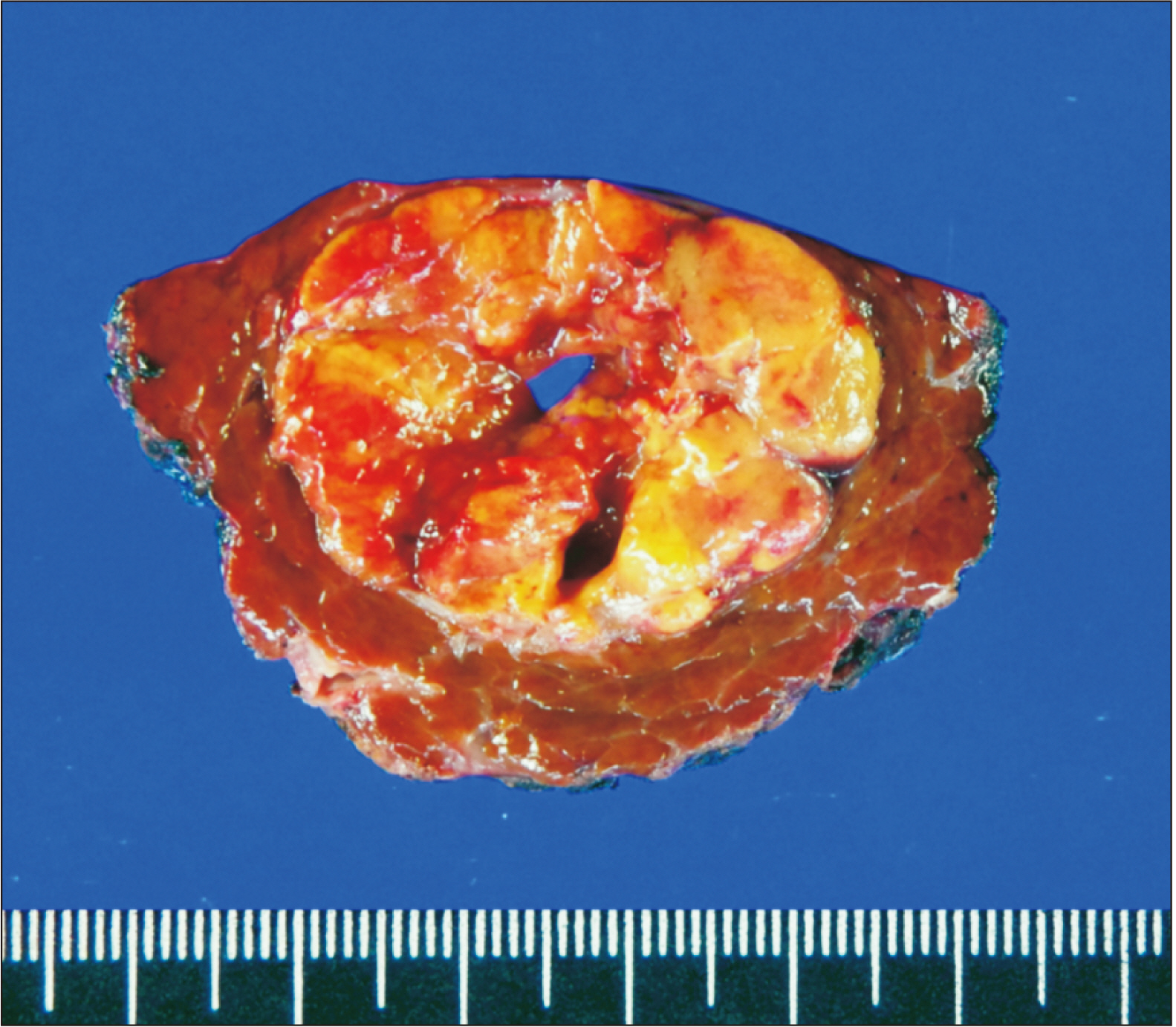
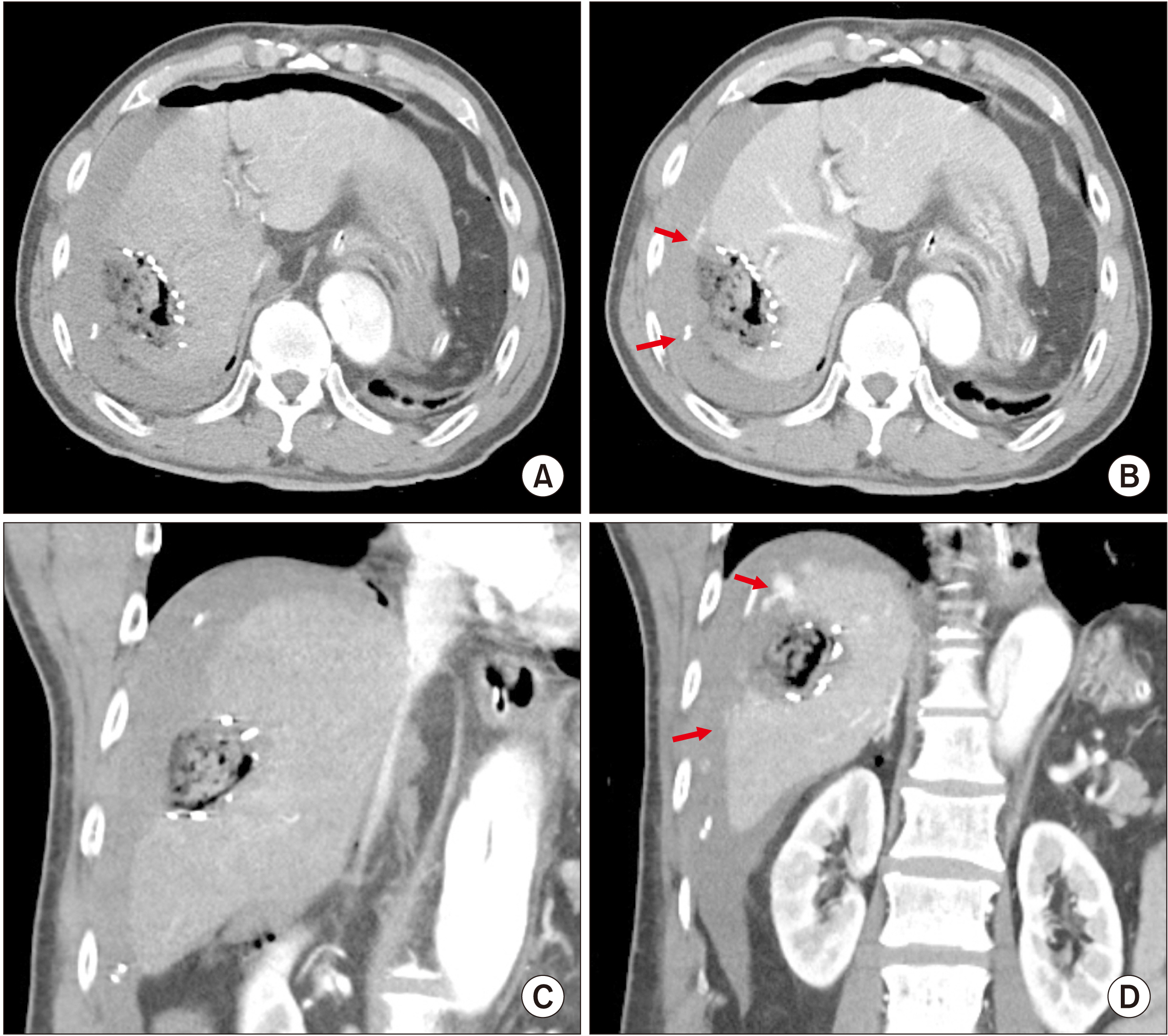
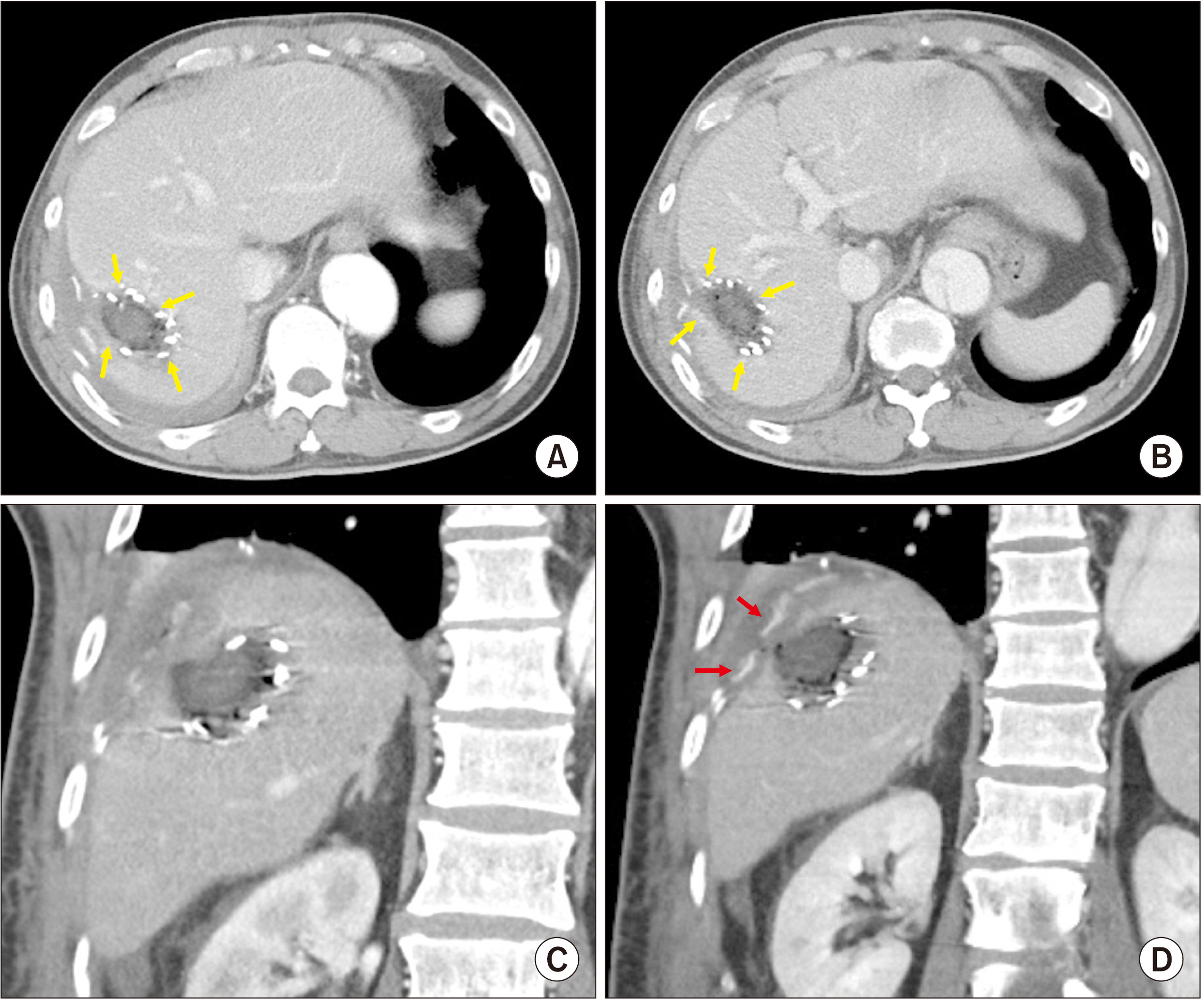
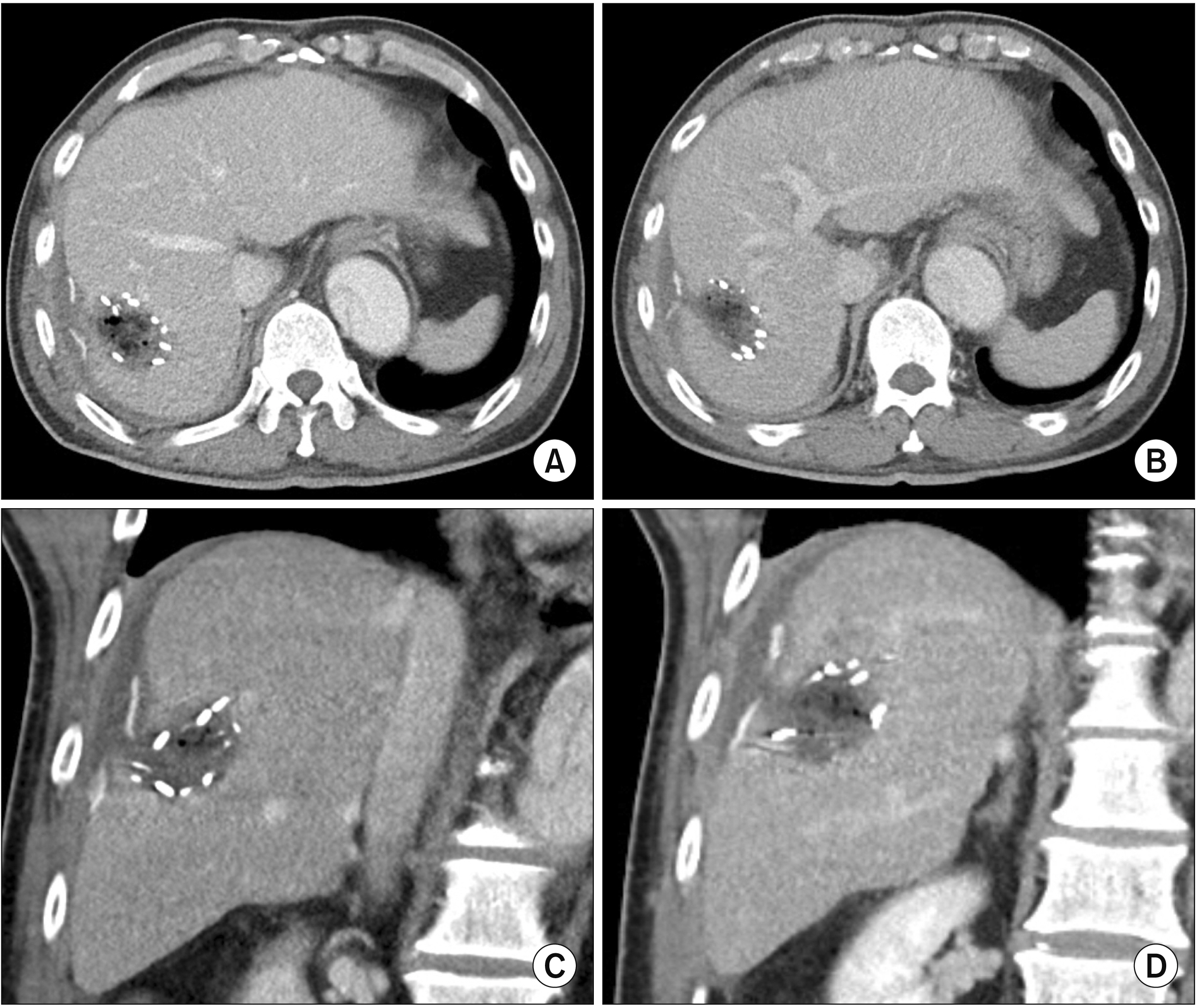
- Various topical hemostatic agents can help induce coagulation at the liver cut surface. However, hemostasis is usually ineffective in controlling bleeding. We present a case of rescue fibrin glue-infiltrating hemostasis combined with hepatorrhaphy to manage intractable postoperative bleeding from the liver cut surface. The case was a 56-year-old male patient with hepatocellular carcinoma in hepatitis B virus-associated cirrhotic liver. The patient was administered warfarin because of graft replacement of the ascending aorta and hemi-arch one year earlier. After warfarin was discontinued, segment VII partial hepatectomy was performed according to standard procedures. However, considerable bleeding occurred during and after hepatectomy. Bleeding from the liver cut surface was controlled over one hour using surface coagulation and topical application of four kinds of hemostatic agents. However, active abdominal bleeding led to reoperation soon after the hepatectomy. During the reoperation, we identified diffuse oozing from the edge of the liver cut surface which was difficult to control. Thus, we performed direct parenchymal injection of fibrin glue at the bleeding points using 12 fibrin glue kits which induced complete hemostasis. Because the patient would undergo anticoagulation again soon after the operation, we also performed hepatorrhaphy. The patient recovered uneventfully after the reoperation. He has been doing well for six months without complications. In conclusion, fibrin glue-infiltrating hemostasis effectively controlled intractable bleeding from the hepatic cut surface in our case. Thus, it can be considered as an optional method for rescue hemostasis.
Keyword
Figure
Reference
-
1. Fonouni H, Kashfi A, Majlesara A, Stahlheber O, Konstantinidis L, Gharabaghi N, et al. 2018; Hemostatic efficiency of modern topical sealants: comparative evaluation after liver resection and splenic laceration in a swine model. J Biomed Mater Res B Appl Biomater. 106:1307–1316. DOI: 10.1002/jbm.b.33937. PMID: 28644516.
Article2. Sanjay P, Watt DG, Wigmore SJ. 2013; Systematic review and meta-analysis of haemostatic and biliostatic efficacy of fibrin sealants in elective liver surgery. J Gastrointest Surg. 17:829–836. DOI: 10.1007/s11605-012-2055-7. PMID: 23086450.
Article3. Berrevoet F, de Hemptinne B. 2007; Use of topical hemostatic agents during liver resection. Dig Surg. 24:288–293. DOI: 10.1159/000103660. PMID: 17657154.
Article4. Mosesson MW. 1990; Fibrin polymerization and its regulatory role in hemostasis. J Lab Clin Med. 116:8–17. DOI: 10.1007/978-3-642-84318-1_3. PMID: 2198321.5. de Boer MT, Boonstra EA, Lisman T, Porte RJ. 2012; Role of fibrin sealants in liver surgery. Dig Surg. 29:54–61. DOI: 10.1159/000335735. PMID: 22441621.
Article6. Hwang S, Jung DH, Song GW, Ha TY, Jwa EK, Lee SG. 2016; Fibrin glue-infiltrating hemostasis for intractable bleeding from the liver or spleen during liver transplantation. Ann Hepatobiliary Pancreat Surg. 20:197–200. DOI: 10.14701/ahbps.2016.20.4.197. PMID: 28261700. PMCID: PMC5325153.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fibrin glue-infiltrating hemostasis for intractable bleeding from the liver or spleen during liver transplantation
- Fibrin Glue for Bleeding after Total Knee Arthroplasty
- Comparison of Hemostatic Effect of Endoscopic Injection with Fibrin Glue (FG) and Hypertonic Saline - epinephrine (HSE) for Peptic Ulcer Bleeding: A prospective randomized trial
- The Efficiency of Fibrin Glue at Bicoronary Approach in Facial Surgery
- The Use of Fibrin Tissue Glue in Thyroid Surgery; A Randomized-Prospective Trial