Arch Hand Microsurg.
2021 Dec;26(4):293-297. 10.12790/ahm.21.0122.
Anterolateral Thigh Free Flap to Cover Diabetic Foot Defect by Using Reverse Flow of Severely Calcified Dorsalis Pedis Artery
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Dongguk University Ilsan Hospital, Dongguk University School of Medicine, Goyang, Korea
- KMID: 2522628
- DOI: http://doi.org/10.12790/ahm.21.0122
Abstract
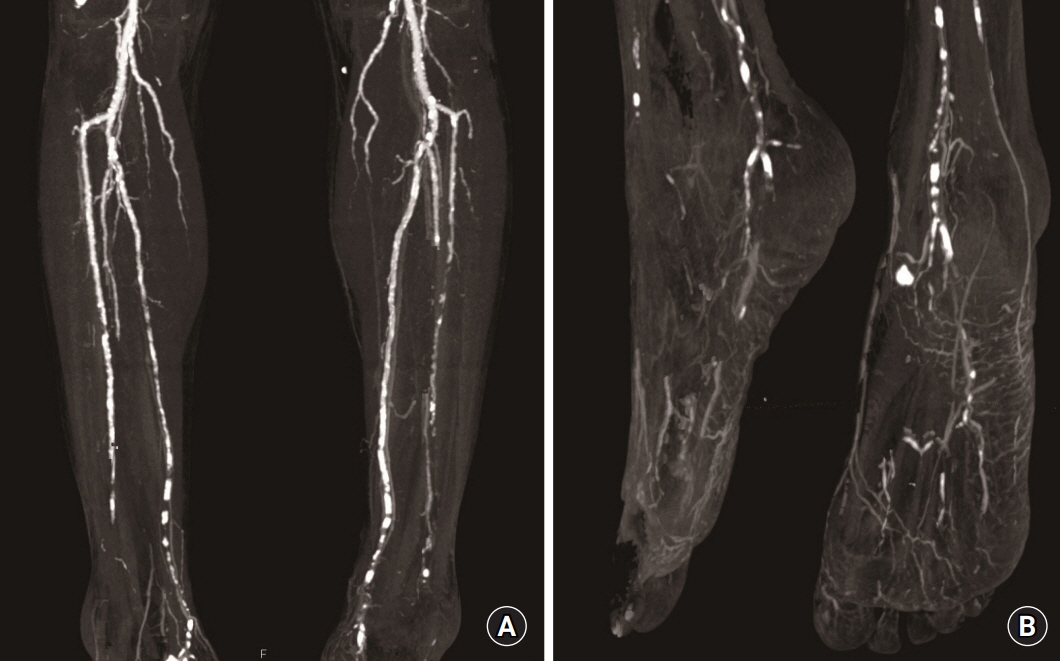
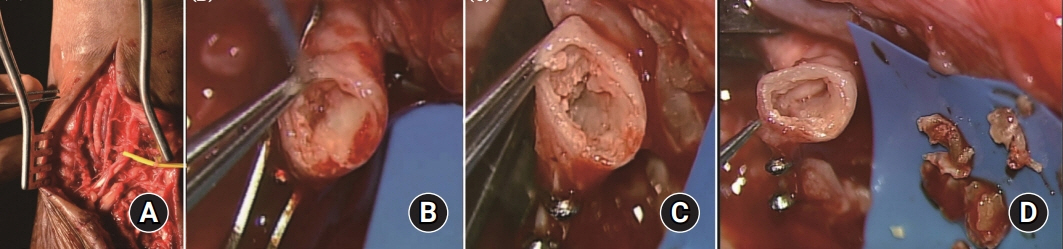
- Low blood flow in the distal part of the diabetic foot aggravates the wound to an ischemic state, which eventually leads to amputation. However, major advancements in microvascular surgery have shown the ability to salvage the limb even in the presence of poor perfusion. Since a foot is constituted of a complex network of angiosomes, each separate territory of the foot is supplied by interconnected vessels. We report the successful salvage of a severe diabetic foot injury of a 72-year-old male patient with a heavily calcified dorsalis pedis artery (DPA). Although the proximal end of the DPA was clogged to prevent the flow of blood and was insufficient to use as a recipient vessel, reverse flow from the distal end was restored after removing multiple calcification fragments. As a result, a large soft-tissue defect on the third and fourth toe region was successfully covered by a contralateral anterolateral thigh free flap.
Keyword
Figure
Reference
-
1. Chang JW, Heo W, Choi M, Lee JH. The appropriate management algorithm for diabetic foot: a single-center retrospective study over 12 years. Medicine (Baltimore). 2018; 97:e11454.2. Bandyk DF. The diabetic foot: Pathophysiology, evaluation, and treatment. Semin Vasc Surg. 2018; 31:43–8.
Article3. Evans KK, Attinger CE, Al-Attar A, et al. The importance of limb preservation in the diabetic population. J Diabetes Complications. 2011; 25:227–31.
Article4. Kolbenschlag J, Hellmich S, Germann G, Megerle K. Free tissue transfer in patients with severe peripheral arterial disease: functional outcome in reconstruction of chronic lower extremity defects. J Reconstr Microsurg. 2013; 29:607–14.
Article5. Randon C, Vermassen F, Jacobs B, De Ryck F, Van Landuyt K, Taes Y. Outcome of arterial reconstruction and free-flap coverage in diabetic foot ulcers: long-term results. World J Surg. 2010; 34:177–84.
Article6. Attinger CE, Brown BJ. Amputation and ambulation in diabetic patients: function is the goal. Diabetes Metab Res Rev. 2012; 28(Suppl 1):93–6.
Article7. Orhan E, Özçağlayan Ö. Collateral circulation between angiosomes in the feet of diabetic patients. Vascular. 2018; 26:432–9.
Article8. Attinger CE, Evans KK, Bulan E, Blume P, Cooper P. Angiosomes of the foot and ankle and clinical implications for limb salvage: reconstruction, incisions, and revascularization. Plast Reconstr Surg. 2006; 117(7 Suppl):261S–293S.
Article9. Ducic I, Rao SS, Attinger CE. Outcomes of microvascular reconstruction of single-vessel lower extremities: limb salvage versus amputation. J Reconstr Microsurg. 2009; 25:475–8.
Article10. Bahk S, Doh G, Hong KY, Lim S, Eo S. Reverse-flow intrinsic fasciocutaneous island flaps in foot reconstruction. Int J Low Extrem Wounds. 2017; 16:296–301.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reverse Dorsalis Pedis Flap Based on the Distal Communicating Artery of the Dorsalis Pedis Artery for the Reconstruction of the Forefoot Defect
- Hinged multiperforator-based extended dorsalis pedis adipofascial flap for dorsal foot defects
- Heel Pad Reconstruction using Doresalis Pedis Free Flap or Rotation Flap
- Distally Based Anterolateral thigh Pedicled Flap in the Reconstruction of Defect Around Knee
- Reconstruction of the Hand Using Fabricated Great Toe Pulp and Anterolateral Thigh Chimeric Free Flap