Arch Hand Microsurg.
2021 Dec;26(4):254-264. 10.12790/ahm.21.0123.
Treatment of Phalangeal Joint Stiffness Related to Proximal Phalangeal Bone Fractures: Therapeutic Effects on the Range of Motion and Finger Pain
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Konkuk University School of Medicine, Seoul, Korea
- KMID: 2522623
- DOI: http://doi.org/10.12790/ahm.21.0123
Abstract
- Purpose
Proximal phalangeal bone fractures with displacement are treated using operative procedures. These fractures can cause stiffness of the interphalangeal or metacarpophalangeal joints, which can be relieved using various operative and nonoperative techniques. This study analyzed the range of motion (ROM) and pain after a combination therapy to treat finger stiffness following proximal phalangeal fractures.
Methods
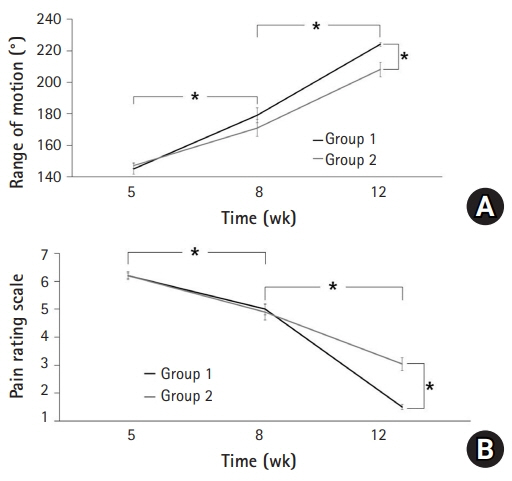
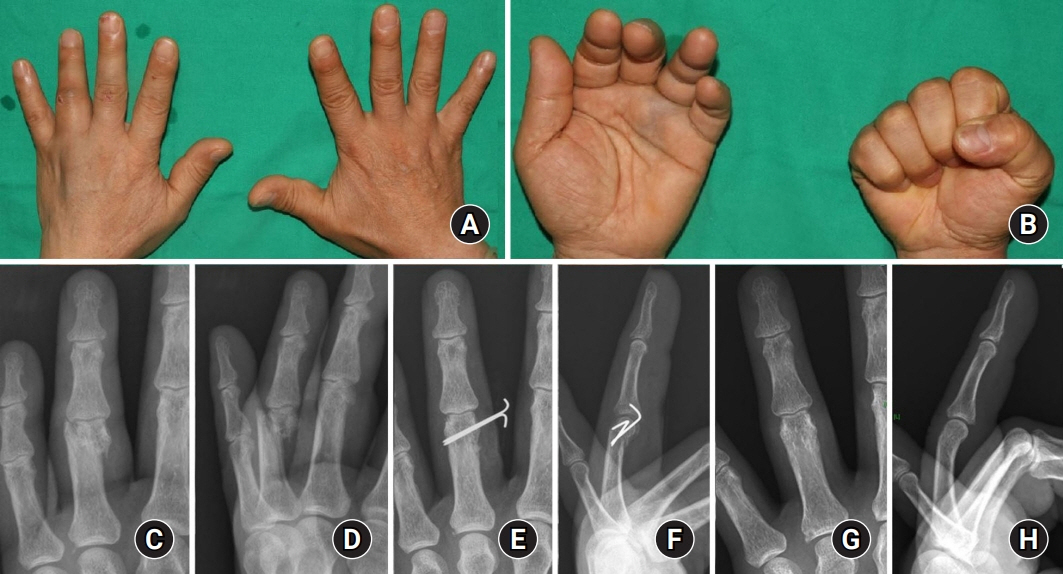
Fifty-two patients who underwent operative procedures for proximal phalangeal fractures and showed finger stiffness from March 2015 to January 2021 were included in this retrospective study. The patients in group 1 (n=24) performed elastic resistance exercises, while those in group 2 (n=28) underwent conventional exercise. ROM and pain score were measured at 5, 8, and 12 weeks postoperatively. Furthermore, a patient with a swan-neck deformity and intractable stiffness was treated using partial translocation of the extensor apparatus, and the postoperative outcome is presented.
Results
Group 1 showed a larger ROM and less pain than group 2 at 12 weeks postoperatively (p<0.05). Patients in both groups exhibited notable improvements with regard to ROM and pain during the study period (p<0.05). In addition, the swan-neck deformity accompanying hyperextension of the proximal interphalangeal joint was significantly relieved.
Conclusion
Proximal phalangeal bone fractures can lead to stiffness of the interphalangeal and metacarpophalangeal joints. Joint stiffness was relieved using an elastic resistance exercise protocol in the early postoperative period. Intractable stiffness showing a fixed joint angle can be treated with thorough tenolysis and corrective surgery.
Keyword
Figure
Cited by 1 articles
-
A novel finger brace for preventing finger stiffness after trauma or surgery: a preliminary report with a case series
Dae-Geun Kim, Hyo Jun Park
Arch Hand Microsurg. 2023;28(4):239-249. doi: 10.12790/ahm.23.0033.
Reference
-
1. Green DP, Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH. Green’s operative hand surgery. 5th ed. Philadelphia: Saunders/Elsevier;2010.2. Oetgen ME, Dodds SD. Non-operative treatment of common finger injuries. Curr Rev Musculoskelet Med. 2008; 1:97–102.
Article3. Widgerow AD, Edinburg M, Biddulph SL. An analysis of proximal phalangeal fractures. J Hand Surg Am. 1987; 12:134–9.
Article4. Freeland AE, Orbay JL. Extraarticular hand fractures in adults: a review of new developments. Clin Orthop Relat Res. 2006; 445:133–45.5. Hardy MA. Principles of metacarpal and phalangeal fracture management: a review of rehabilitation concepts. J Orthop Sports Phys Ther. 2004; 34:781–99.
Article6. Vahey JW, Wegner DA, Hastings H 3rd. Effect of proximal phalangeal fracture deformity on extensor tendon function. J Hand Surg Am. 1998; 23:673–81.
Article7. Beekman RA, Abbot AE, Taylor NL, Rosenwasser MP, Strauch RJ. Extensor mechanism slide for the treatment of proximal interphalangeal joint extension lag: an anatomic study. J Hand Surg Am. 2004; 29:1063–8.
Article8. Glasgow C, Fleming J, Tooth LR, Hockey RL. The long-term relationship between duration of treatment and contracture resolution using dynamic orthotic devices for the stiff proximal interphalangeal joint: a prospective cohort study. J Hand Ther. 2012; 25:38–46.
Article9. Freeland AE, Hardy MA, Singletary S. Rehabilitation for proximal phalangeal fractures. J Hand Ther. 2003; 16:129–42.
Article10. Schneider LH. Tenolysis and capsulectomy after hand fractures. Clin Orthop Relat Res. 1996; (327):72–8.
Article11. Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998; 23:827–32.
Article12. Yang G, McGlinn EP, Chung KC. Management of the stiff finger: evidence and outcomes. Clin Plast Surg. 2014; 41:501–12.13. Wang D, Sun K, Jiang W. Mini-plate versus Kirschner wire internal fixation for treatment of metacarpal and phalangeal fractures. J Int Med Res. 2020; 48:300060519887264.
Article14. Tuffaha SH, Lee WP. Treatment of proximal interphalangeal joint contracture. Hand Clin. 2018; 34:229–35.
Article15. Lutsky KF, Matzon JL, Dwyer J, Kim N, Beredjiklian PK. Results of operative intervention for finger stiffness after fractures of the hand. Hand (N Y). 2016; 11:341–6.
Article16. Brüser P, Poss T, Larkin G. Results of proximal interphalangeal joint release for flexion contractures: midlateral versus palmar incision. J Hand Surg Am. 1999; 24:288–94.17. Hiwatari R, Kuniyoshi K, Aoki M, Hashimoto K, Suzuki T, Takahashi K. Fractional Fowler tenotomy for chronic mallet finger: a cadaveric biomechanical study. J Hand Surg Am. 2012; 37:2263–8.
Article18. Charruau B, Laulan J, Saint-Cast Y. Lateral band translocation for swan-neck deformity: outcomes of 41 digits after a mean follow-up of eight years. Orthop Traumatol Surg Res. 2016; 102(4 Suppl):S221–4.
Article19. Miller L, Crosbie J, Wajon A, Ada L. No difference between two types of exercise after proximal phalangeal fracture fixation: a randomised trial. J Physiother. 2016; 62:12–9.
Article20. Vinstrup J, Calatayud J, Jakobsen MD, et al. Hand strengthening exercises in chronic stroke patients: dose-response evaluation using electromyography. J Hand Ther. 2018; 31:111–21.
Article21. Liao CD, Tsauo JY, Huang SW, Ku JW, Hsiao DJ, Liou TH. Effects of elastic band exercise on lean mass and physical capacity in older women with sarcopenic obesity: a randomized controlled trial. Sci Rep. 2018; 8:2317.
Article22. Ganesh Kumar N, Chung KC. An evidence-based guide for managing phalangeal fractures. Plast Reconstr Surg. 2021; 147:846e–861e.
Article23. Chang BL, Mondshine J, Attinger CE, Kleiber GM. Targeted muscle reinnervation improves pain and ambulation outcomes in highly comorbid amputees. Plast Reconstr Surg. 2021; 148:376–86.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Proximal Phalangeal Fractures of the Hand Using Finger Nail Traction and a Digital Splint: A Prospective Study of 43 Cases
- Current Concepts in Management of Phalangeal Fractures
- Operative treatment of the phalangeal neck fracture in hand
- Operative Treatment of the Malunited Phalangeal Neck Fractures
- Usefulness of Miniplate Fixation for the Fractures of Metacarpal and Phalangeal Bones of the Hand