J Korean Med Sci.
2021 Nov;36(45):e316. 10.3346/jkms.2021.36.e316.
Effect of Quality Control Program in Surgical Management of Early Cervical Cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2522554
- DOI: http://doi.org/10.3346/jkms.2021.36.e316
Abstract
- Background
Regular assessments of clinical performance in gynecologic cancer surgery is important for the safety of patients. We evaluated the effects of quality control (QC) program on the treatment pattern and clinical outcomes of early cervical cancer.
Methods
Medical records of cervical cancer patients who received operation in our institution from January 2007 to December 2018 were retrospectively reviewed. Cases were divided into 2 groups, before and after the initiation of QC program, group 1 (2007–2013) and group 2 (2014–2018), based on the operation date. Two groups were compared in clinicopathologic variables, surgical methods, operative details, adjuvant treatments, recurrence and survival.
Results
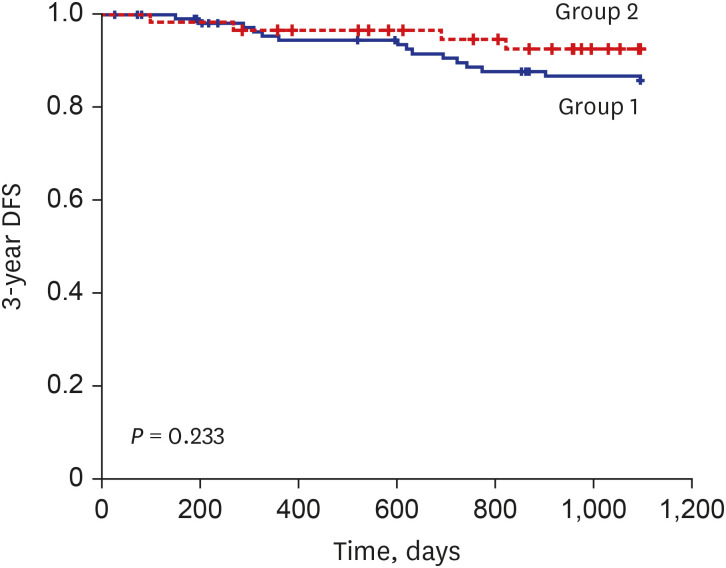
A total of 305 cervical cancer patients were included in the analysis, 210 in group 1 and 95 in group 2. In group 2, minimally invasive surgery (MIS) was more frequently performed (60.0% vs. 76.8%, P = 0.004), especially in earlier stages (stage IA, 72.6% vs. 100.0%; stage IB, 52.2% vs. 69.5%). However, the median tumor size treated by MIS was decreased in stage IB (20 mm vs. 17 mm, P = 0.015). Frequency of adjuvant treatment was also reduced in stage IB (56.5% vs. 37.3%, P = 0.016). Recurrence within 3 years, 3-year disease free survival and overall survival did not show significant difference; however, 3-year recurrence after MIS was significantly reduced in stage IB.
Conclusion
QC program enforced stricter patient selection criteria for MIS and positively affected clinical outcomes in cervical cancer patients who underwent surgery. Systemic monitoring should be considered for patient safety.
Figure
Reference
-
1. Koh WJ, Abu-Rustum NR, Bean S, Bradley K, Campos SM, Cho KR, et al. Cervical cancer, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019; 17(1):64–84. PMID: 30659131.
Article2. Verleye L, Vergote I, Reed N, Ottevanger PB. Quality assurance for radical hysterectomy for cervical cancer: the view of the European Organization for Research and Treatment of Cancer--Gynecological Cancer Group (EORTC-GCG). Ann Oncol. 2009; 20(10):1631–1638. PMID: 19556323.
Article3. du Bois A, Rochon J, Pfisterer J, Hoskins WJ. Variations in institutional infrastructure, physician specialization and experience, and outcome in ovarian cancer: a systematic review. Gynecol Oncol. 2009; 112(2):422–436. PMID: 18990435.
Article4. Arora V, Somashekhar SP. Essential surgical skills for a gynecologic oncologist. Int J Gynaecol Obstet. 2018; 143(Suppl 2):118–130. PMID: 30306588.
Article5. Vernooij F, Heintz P, Witteveen E, van der Graaf Y. The outcomes of ovarian cancer treatment are better when provided by gynecologic oncologists and in specialized hospitals: a systematic review. Gynecol Oncol. 2007; 105(3):801–812. PMID: 17433422.
Article6. Hillner BE, Smith TJ, Desch CE. Hospital and physician volume or specialization and outcomes in cancer treatment: importance in quality of cancer care. J Clin Oncol. 2000; 18(11):2327–2340. PMID: 10829054.
Article7. Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018; 379(20):1895–1904. PMID: 30380365.
Article8. Rao ST, Nusrath S, Iyer RR, Patnaik SC, Saksena AR, Vanzar P, et al. Interpretation and implications of LACC trial. Indian J Gynecol Oncolog. 2019; 17(2):39.
Article9. Köhler C, Schneider A, Marnitz S, Plaikner A. The basic principles of oncologic surgery during minimally invasive radical hysterectomy. J Gynecol Oncol. 2020; 31(1):e33. PMID: 31833260.
Article10. Vergote I, Magrina JF, Zanagnolo V, Magtibay PM, Butler K, Gil-Moreno A, et al. The LACC trial and minimally invasive surgery in cervical cancer. J Minim Invasive Gynecol. 2020; 27(2):462–463. PMID: 31520725.
Article11. Kimmig R, Ind T. Minimally invasive surgery for cervical cancer: consequences for treatment after LACC Study. J Gynecol Oncol. 2018; 29(4):e75. PMID: 29770634.
Article12. Li P, Chen L, Ni Y, Liu J, Li D, Guo J, et al. Comparison between laparoscopic and abdominal radical hysterectomy for stage IB1 and tumor size <2 cm cervical cancer with visible or invisible tumors: a multicentre retrospective study. J Gynecol Oncol. 2021; 32(2):e17. PMID: 33470062.
Article13. Kim SI, Cho JH, Seol A, Kim YI, Lee M, Kim HS, et al. Comparison of survival outcomes between minimally invasive surgery and conventional open surgery for radical hysterectomy as primary treatment in patients with stage IB1-IIA2 cervical cancer. Gynecol Oncol. 2019; 153(1):3–12. PMID: 30642625.
Article14. Chen C, Liu P, Ni Y, Tang L, Xu Y, Bin X, et al. Laparoscopic versus abdominal radical hysterectomy for stage IB1 cervical cancer patients with tumor size ≤ 2 cm: a case-matched control study. Int J Clin Oncol. 2020; 25(5):937–947. PMID: 32062731.15. Stranne J, Axen E, Franck-Lissbrant I, Fransson P, Frånlund M, Hugosson J, et al. Single institution followed by national implementation of systematic surgical quality control and feedback for radical prostatectomy: a 20-year journey. World J Urol. 2020; 38(6):1397–1411. PMID: 31388817.
Article16. Biau DJ, Resche-Rigon M, Godiris-Petit G, Nizard RS, Porcher R. Quality control of surgical and interventional procedures: a review of the CUSUM. Qual Saf Health Care. 2007; 16(3):203–207. PMID: 17545347.
Article17. Murzi M, Cerillo AG, Bevilacqua S, Gasbarri T, Kallushi E, Farneti P, et al. Enhancing departmental quality control in minimally invasive mitral valve surgery: a single-institution experience. Eur J Cardiothorac Surg. 2012; 42(3):500–506. PMID: 22427391.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of the Self-efficacy Promoting Program for Prevention of Uterine Cervical Cancer on Self-efficacy and Performance of Preventive Health Behaviors in Nurses
- National Cancer Screening Program
- Minimally invasive radical hysterectomy and the importance of avoiding cancer cell spillage for early-stage cervical cancer: a narrative review
- The Development and Effect of Navigator Education Program for Cancer Screening on Women in the Community
- Trend analysis of process quality indicators for the Korean National Cervical Cancer Screening Program from 2005 to 2013