Brain Tumor Res Treat.
2021 Oct;9(2):46-57. 10.14791/btrt.2021.9.e9.
Outcome After Protontherapy for Progression or Recurrence of Surgically Treated Meningioma
- Affiliations
-
- 1Department of Neurosurgery, Lariboisière Hospital, Paris, France
- 2INSERM U1153, Statistic and Epidemiologic Research Center Sorbonne Paris Cité (CRESS), ECSTRRA Team, Université de Paris, Paris, France
- 3Agence régionale de santé, Saint Denis, France
- KMID: 2522219
- DOI: http://doi.org/10.14791/btrt.2021.9.e9
Abstract
- Background
To assess the outcome after meningioma surgery and protontherapy (PT).
Methods
We processed the French Système National des Données de Santé database to retrieve appropriate cases of meningiomas operated and irradiated between 2008 and 2017. Survival methods were implemented.
Results
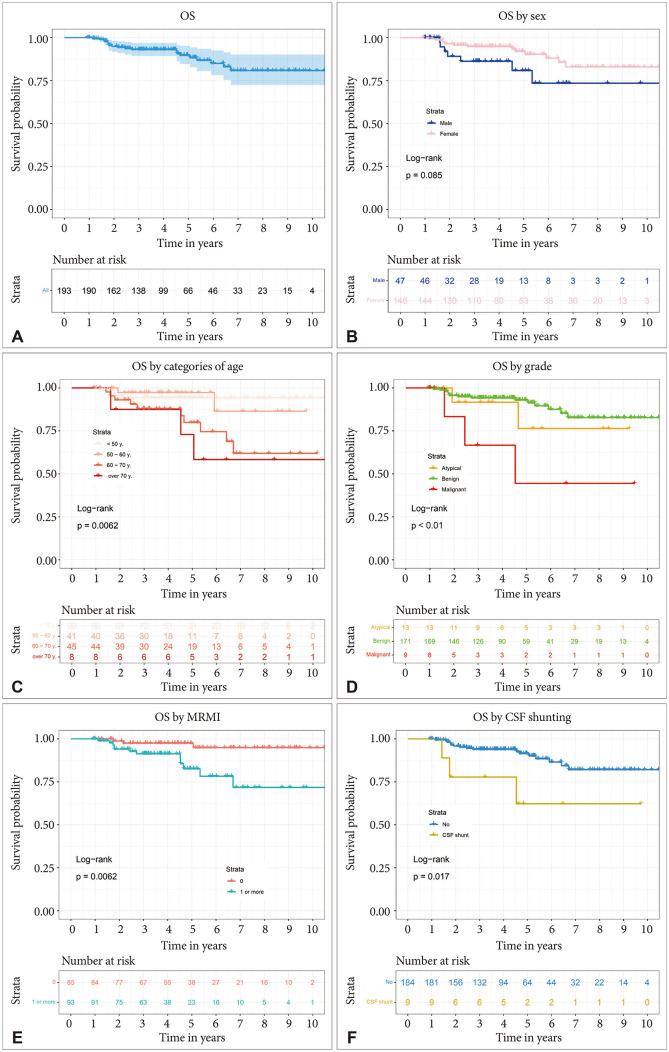
One hundred ninety-three patients who received PT after meningioma surgery over a 10-year period were identified. Of the 193 patients, 75.6% were female. Median age at surgery was 50 years (interquartile range [IQR] 41-62). The median number of PT fractions was 31 (IQR 30-39) given over a median duration of 52 days (IQR 44-69). Fourteen patients (7.3%) also received photon radiotherapy and six patients (3.1%) stereotactic radiosurgery. Median follow-up was 4.4 years (IQR 3.86-4.71). Five-year progression-free survival (PFS) rate was 69% (95% confidence interval [CI] 62.1–76.6). For benign, atypical, and malignant meningioma, 5-year PFS rates were 71.5% (95% CI 64.4-79.4), 55.6% (95% CI 32.5-95), and 35.6% (95% CI 12.8-98.9), respectively (p<0.01). In the adjusted regression, tumour location (hazard ratio [HR]=0.1, 95% CI 0.05-0.22, p<0.001), aggressive meningioma (HR=2.26, 95% CI 1.1-4.66, p=0.027), and the need of cerebrospinal fluid (CSF) insertion for hydrocephalus (HR=3.51, 95% CI 1.32-9.31, p=0.012) remained significantly associated to the PFS. All grades considered, 5-year overall survival (OS) rates was 89.7% (95% CI 84.6-95.1). For benign, atypical, and malignant meningioma, 5-year OS rates were 93% (95% CI 88.7-97.4), 76.4% (95% CI 51.4-100), and 44.4% (95% CI 16.7-100), respectively (p<0.01). In the multivariable regression, an older age above 70 years (HR=5.95, 95% CI 2.09-16.89, p<0.001) associated to a high level of comorbidities (HR=5.31, 95% CI 1.43-19.78, p=0.013) and a malignant meningioma (HR=5.68, 95% CI 1.54-20.94, p=0.009) remained significantly associated to a reduced OS.
Conclusion
Five-year PFS and OS after meningioma surgery and PT is favourable but impaired for older patients with high level of morbidities, tumour of the convexity, malignant histopathology and for those requiring CSF shunting. Further inclusion and prolonged follow-up is required to assess other predictors such as sex, tumour volume, or given dose.
Keyword
Figure
Reference
-
1. Champeaux C, Wilson E, Brandner S, Shieff C, Thorne L. World Health Organization grade III meningiomas. A retrospective study for outcome and prognostic factors assessment. Br J Neurosurg. 2015; 29:693–698. PMID: 26098606.2. Champeaux C, Dunn L. World Health Organization grade II meningioma: a 10-year retrospective study for recurrence and prognostic factor assessment. World Neurosurg. 2016; 89:180–186. PMID: 26850975.3. Champeaux C, Houston D, Dunn L. Atypical meningioma. A study on recurrence and disease-specific survival. Neurochirurgie. 2017; 63:273–281. PMID: 28882609.4. Gavrielov-Yusim N, Friger M. Use of administrative medical databases in population-based research. J Epidemiol Community Health. 2014; 68:283–287. PMID: 24248997.5. Tuppin P, Rudant J, Constantinou P, et al. Value of a national administrative database to guide public decisions: from the système national d'information interrégimes de l'Assurance Maladie (SNIIRAM) to the système national des données de santé (SNDS) in France. Rev Epidemiol Sante Publique. 2017; 65 Suppl 4:S149–S167. PMID: 28756037.6. Champeaux C, Weller J, Katsahian S. Epidemiology of meningiomas. A nationwide study of surgically treated tumours on French medico-administrative data. Cancer Epidemiol. 2019; 58:63–70. PMID: 30481723.7. Champeaux-Depond C, Constantinou P, Weller J. Cause-specific survival after meningioma surgery: a nationwide population-based competing risk study. World Neurosurg. 2021; 146:e67–e75. PMID: 33096279.8. Champeaux-Depond C, Weller J, Resche-Rigon M. Neurofibromatosis type 2: a nationwide population-based study focused on survival after meningioma surgery. Clin Neurol Neurosurg. 2020; 198:106236. PMID: 33002675.9. Champeaux-Depond C, Weller J, Froelich S, Resche-Rigon M. A nationwide population-based study on overall survival after meningioma surgery. Cancer Epidemiol. 2020; 70:101875. PMID: 33360358.10. Constantinou P, Tuppin P, Fagot-Campagna A, Gastaldi-Ménager C, Schellevis FG, Pelletier-Fleury N. Two morbidity indices developed in a nationwide population permitted performant outcome-specific severity adjustment. J Clin Epidemiol. 2018; 103:60–70. PMID: 30016643.11. Lang TA, Altman DG. Basic statistical reporting for articles published in biomedical journals: the “Statistical Analyses and Methods in the Published Literature” or the SAMPL guidelines. Int J Nurs Stud. 2015; 52:5–9. PMID: 25441757.12. Nicholls SG, Quach P, von Elm E, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement: methods for arriving at consensus and developing reporting guidelines. PLoS One. 2015; 10:e0125620. PMID: 25965407.13. Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957; 20:22–39. PMID: 13406590.14. Florijn MA, Sharfo AWM, Wiggenraad RGJ, et al. Lower doses to hippocampi and other brain structures for skull-base meningiomas with intensity modulated proton therapy compared to photon therapy. Radiother Oncol. 2020; 142:147–153. PMID: 31522879.15. Kaur G, Sayegh ET, Larson A, et al. Adjuvant radiotherapy for atypical and malignant meningiomas: a systematic review. Neuro Oncol. 2014; 16:628–636. PMID: 24696499.16. Champeaux C, Jecko V, Houston D, et al. Malignant meningioma: an international multicentre retrospective study. Neurosurgery. 2019; 85:E461–E469. PMID: 30566646.17. Jenkinson MD, Javadpour M, Haylock BJ, et al. The ROAM/EORTC-1308 trial: radiation versus observation following surgical resection of atypical meningioma: study protocol for a randomised controlled trial. Trials. 2015; 16:519. PMID: 26576533.18. Detti B, Scoccianti S, Di Cataldo V, et al. Atypical and malignant meningioma: outcome and prognostic factors in 68 irradiated patients. J Neurooncol. 2013; 115:421–427. PMID: 24045968.19. Vernimmen FJ, Harris JK, Wilson JA, Melvill R, Smit BJ, Slabbert JP. Stereotactic proton beam therapy of skull base meningiomas. Int J Radiat Oncol Biol Phys. 2001; 49:99–105. PMID: 11163502.20. Boskos C, Feuvret L, Noel G, et al. Combined proton and photon conformal radiotherapy for intracranial atypical and malignant meningioma. Int J Radiat Oncol Biol Phys. 2009; 75:399–406. PMID: 19203844.21. Gennatas ED, Wu A, Braunstein SE, et al. Preoperative and postoperative prediction of long-term meningioma outcomes. PLoS One. 2018; 13:e0204161. PMID: 30235308.22. van Alkemade H, de Leau M, Dieleman EM, et al. Impaired survival and long-term neurological problems in benign meningioma. Neuro Oncol. 2012; 14:658–666. PMID: 22406926.23. Champeaux C, Houston D, Dunn L, Resche-Rigon M. Intracranial WHO grade I meningioma: a competing risk analysis of progression and disease-specific survival. Acta Neurochir (Wien). 2019; 161:2541–2549.24. Wenkel E, Thornton AF, Finkelstein D, et al. Benign meningioma: partially resected, biopsied, and recurrent intracranial tumors treated with combined proton and photon radiotherapy. Int J Radiat Oncol Biol Phys. 2000; 48:1363–1370. PMID: 11121635.25. Lesueur P, Calugaru V, Nauraye C, et al. Proton therapy for treatment of intracranial benign tumors in adults: a systematic review. Cancer Treat Rev. 2019; 72:56–64. PMID: 30530009.26. Weber DC, Schneider R, Goitein G, et al. Spot scanning-based proton therapy for intracranial meningioma: long-term results from the Paul Scherrer Institute. Int J Radiat Oncol Biol Phys. 2012; 83:865–871. PMID: 22138457.27. Hug EB, Devries A, Thornton AF, et al. Management of atypical and malignant meningiomas: role of high-dose, 3D-conformal radiation therapy. J Neurooncol. 2000; 48:151–160. PMID: 11083080.28. DeVries A, Munzenrider JE, Hedley-Whyte T, Hug EB. The role of radiotherapy in the treatment of malignant meningiomas. Strahlenther Onkol. 1999; 175:62–67. PMID: 10065140.29. Sanford NN, Yeap BY, Larvie M, et al. Prospective, randomized study of radiation dose escalation with combined proton-photon therapy for benign meningiomas. Int J Radiat Oncol Biol Phys. 2017; 99:787–796. PMID: 28865924.30. El Shafie RA, Czech M, Kessel KA, et al. Evaluation of particle radiotherapy for the re-irradiation of recurrent intracranial meningioma. Radiat Oncol. 2018; 13:86. PMID: 29739417.31. Woehrer A, Hackl M, Waldhör T, et al. Relative survival of patients with non-malignant central nervous system tumours: a descriptive study by the Austrian Brain Tumour Registry. Br J Cancer. 2014; 110:286–296. PMID: 24253501.32. Burkhardt JK, Zinn PO, Graenicher M, et al. Predicting postoperative hydrocephalus in 227 patients with skull base meningioma. Neurosurg Focus. 2011; 30:E9.33. Bir SC, Sapkota S, Maiti TK, Konar S, Bollam P, Nanda A. Evaluation of ventriculoperitoneal shunt-related complications in intracranial meningioma with hydrocephalus. J Neurol Surg B Skull Base. 2017; 78:30–36. PMID: 28180040.34. Doyen J, Falk AT, Floquet V, Hérault J, Hannoun-Lévi JM. Proton beams in cancer treatments: clinical outcomes and dosimetric comparisons with photon therapy. Cancer Treat Rev. 2016; 43:104–112. PMID: 26827698.35. Verma V, Mishra MV, Mehta MP. A systematic review of the cost and cost-effectiveness studies of proton radiotherapy. Cancer. 2016; 122:1483–1501. PMID: 26828647.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Extradural En-Plaque Meningioma Involving Thoracic Spine
- A Rapidly Regrowing Benign Meningioma After Total Removal: Case Report
- A Case of Malignant Meningioma Involving Frontal Bone and Frontal Lobe
- A Case of Primary Extracranial Meningioma in the Ethmoid Sinus
- Prognostic Factors of Atypical Meningioma: Overall Survival Rate and Progression Free Survival Rate