Association between a Multidisciplinary Team Approach and Clinical Outcomes in Patients Undergoing Extracorporeal Cardiopulmonary Resuscitation in the Emergency Department
- Affiliations
-
- 1Department of Emergency Medicine, Chungbuk National University Hospital, Cheongju, Korea
- 2Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Division of Cardiology, Department of Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2522108
- DOI: http://doi.org/10.4070/kcj.2021.0167
Abstract
- Background and Objectives
Despite recent improvements in advanced life support, the overall survival rate after cardiac arrest remains low. We aimed to examine the association of a multidisciplinary team approach with clinical outcomes in patients undergoing extracorporeal cardiopulmonary resuscitation (ECPR) in the emergency department (ED).
Methods
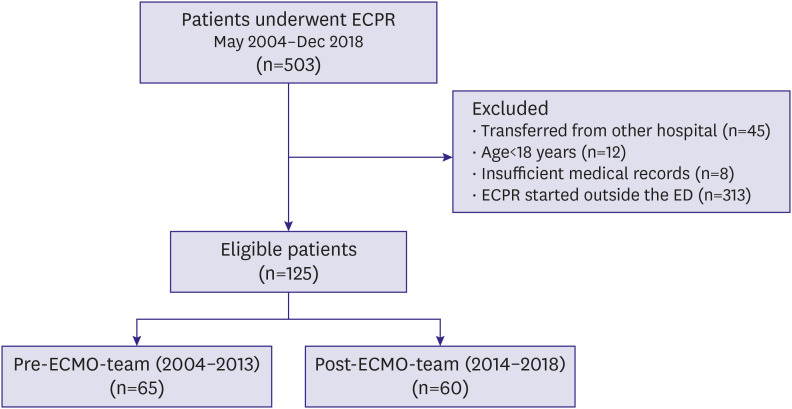
This retrospective, single-center, observational study included 125 patients who underwent ECPR in the ED between May 2004–December 2018. In January 2014, our institution implemented a multidisciplinary extracorporeal membrane oxygenation (ECMO) team. Eligible patients were classified into pre-ECMO-team (n=65) and post-ECMO-team (n=60) groups. The primary outcome was in-hospital mortality.
Results
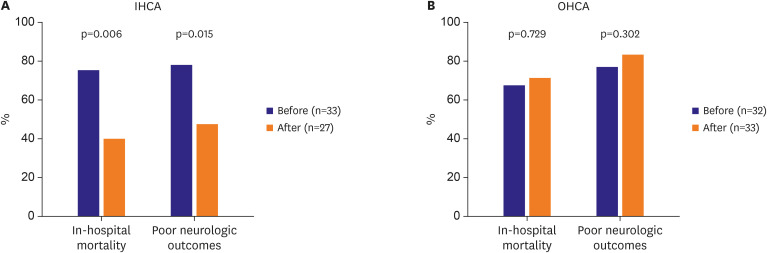
In-hospital mortality (72.3% vs. 58.3%, p=0.102) and poor neurological outcomes (78.5% vs. 68.3%, p=0.283) did not differ significantly between the pre- and post-ECMOteam groups. However, among the 60 patients who experienced in-hospital cardiac arrest,in-hospital mortality (75.8% vs. 40.7%, p=0.006) and poor neurological outcomes (78.8% vs. 48.1%, p=0.015) significantly decreased after the multidisciplinary team formation. Multivariable logistic regression analysis showed that the multidisciplinary team approach (adjusted odds ratio, 0.20; 95% confidence interval, 0.07–0.61; p=0.005) was an independent prognostic factor for in-hospital mortality in in-hospital cardiac arrest patients.
Conclusions
A multidisciplinary team approach was associated with improved clinical outcomes in in-hospital cardiac arrest patients undergoing ECPR in the ED. These findings may help in improving the selection criteria for ECPR in the ED. Further studies to overcome the study limitations may help improving the outcomes of out-of-hospital cardiac arrest patients.
Figure
Cited by 4 articles
-
Key Factors in Improving Clinical Outcomes in Patients with Cardiac Arrest Undergoing Extracorporeal Cardiopulmonary Resuscitation: a Multidisciplinary Team Approach
Jung-Joon Cha, Soon Jun Hong
Korean Circ J. 2021;51(11):919-921. doi: 10.4070/kcj.2021.0307.Current Unmet Needs and Clues to the Solution in the Management of Tricuspid Regurgitation
Byung Joo Sun, Jae-Hyeong Park
Korean Circ J. 2022;52(6):414-428. doi: 10.4070/kcj.2022.0117.Prognostic significance of respiratory quotient in patients undergoing extracorporeal cardiopulmonary resuscitation in Korea
Yun Im Lee, Ryoung-Eun Ko, Soo Jin Na, Jeong-Am Ryu, Yang Hyun Cho, Jeong Hoon Yang, Chi Ryang Chung, Gee Young Suh
Acute Crit Care. 2023;38(2):190-199. doi: 10.4266/acc.2022.01438.Editorial on Paper Titled Comparison of Veno-Arterial Extracorporeal Membrane Oxygenation Type in Patients Listed for Heart Transplantation
Jeong Hoon Yang
Korean Circ J. 2023;53(8):548-549. doi: 10.4070/kcj.2023.0168.
Reference
-
1. Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003; 58:297–308. PMID: 12969608.
Article2. Bloom HL, Shukrullah I, Cuellar JR, Lloyd MS, Dudley SC Jr, Zafari AM. Long-term survival after successful inhospital cardiac arrest resuscitation. Am Heart J. 2007; 153:831–836. PMID: 17452161.
Article3. Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009; 361:22–31. PMID: 19571280.
Article4. Hajbaghery MA, Mousavi G, Akbari H. Factors influencing survival after in-hospital cardiopulmonary resuscitation. Resuscitation. 2005; 66:317–321. PMID: 16081201.
Article5. Mattox KL, Beall AC Jr. Resuscitation of the moribund patient using portable cardiopulmonary bypass. Ann Thorac Surg. 1976; 22:436–442. PMID: 999368.
Article6. Chen YS, Lin JW, Yu HY, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008; 372:554–561. PMID: 18603291.
Article7. Richardson AS, Schmidt M, Bailey M, Pellegrino VA, Rycus PT, Pilcher DV. ECMO cardio-pulmonary resuscitation (ECPR), trends in survival from an international multicentre cohort study over 12-years. Resuscitation. 2017; 112:34–40. PMID: 27993632.
Article8. McCarthy FH, McDermott KM, Kini V, et al. Trends in U.S. extracorporeal membrane oxygenation use and outcomes: 2002–2012. Semin Thorac Cardiovasc Surg. 2015; 27:81–88. PMID: 26686427.
Article9. Paden ML, Rycus PT, Thiagarajan RR; ELSO Registry. Update and outcomes in extracorporeal life support. Semin Perinatol. 2014; 38:65–70. PMID: 24580761.
Article10. Tung YC, Chang GM, Chen YH. Associations of physician volume and weekend admissions with ischemic stroke outcome in Taiwan: a nationwide population-based study. Med Care. 2009; 47:1018–1025. PMID: 19648828.11. Abrams D, Garan AR, Abdelbary A, et al. Position paper for the organization of ECMO programs for cardiac failure in adults. Intensive Care Med. 2018; 44:717–729. PMID: 29450594.
Article12. Hong D, Choi KH, Cho YH, et al. Multidisciplinary team approach in acute myocardial infarction patients undergoing veno-arterial extracorporeal membrane oxygenation. Ann Intensive Care. 2020; 10:83. PMID: 32548658.
Article13. Swanson RW. Recommended guidelines for uniform reporting of data on out-of-hospital cardiac arrests: the “Utstein style”. CMAJ. 1991; 145:407–410. PMID: 1878823.14. D'Arrigo S, Cacciola S, Dennis M, et al. Predictors of favourable outcome after in-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation: A systematic review and meta-analysis. Resuscitation. 2017; 121:62–70. PMID: 29020604.15. Ryu JA, Cho YH, Sung K, et al. Predictors of neurological outcomes after successful extracorporeal cardiopulmonary resuscitation. BMC Anesthesiol. 2015; 15:26. PMID: 25774089.
Article16. Yu HY, Wang CH, Chi NH, et al. Effect of interplay between age and low-flow duration on neurologic outcomes of extracorporeal cardiopulmonary resuscitation. Intensive Care Med. 2019; 45:44–54. PMID: 30547322.
Article17. Langer T, Santini A, Bottino N, et al. “Awake” extracorporeal membrane oxygenation (ECMO): pathophysiology, technical considerations, and clinical pioneering. Crit Care. 2016; 20:150. PMID: 27357690.
Article18. Kass M, Moon M, Vo M, Singal R, Ravandi A. Awake extracorporeal membrane oxygenation for very high-risk coronary angioplasty. Can J Cardiol. 2015; 31:227.e11–227.e13.
Article19. Liu S, Ravandi A, Kass M, Elbarouni B. A case of awake percutaneous extracorporeal membrane oxygenation for high-risk percutaneous coronary intervention. Cureus. 2017; 9:e1191. PMID: 28553569.
Article20. Kacer J, Lindovska M, Surovcik R, et al. Refractory cardiogenic shock due to extensive anterior STEMI with covered left ventricular free wall rupture treated with awake VA-ECMO and LVAD as a double bridge to heart transplantation - collaboration of three cardiac centres. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2015; 159:681–687. PMID: 26498212.
Article21. Youn T, Kim D, Park TK, et al. Clinical outcomes of early extubation strategy in patients undergoing extracorporeal membrane oxygenation as a bridge to heart transplantation. J Korean Med Sci. 2020; 35:e346. PMID: 33140587.
Article22. Park JH, Kim YJ, Ro YS, Kim S, Cha WC, Shin SD. The effect of transport time interval on neurological recovery after out-of-hospital cardiac arrest in patients without a prehospital return of spontaneous circulation. J Korean Med Sci. 2019; 34:e73. PMID: 30863269.
Article23. Kim SJ, Jung JS, Park JH, Park JS, Hong YS, Lee SW. An optimal transition time to extracorporeal cardiopulmonary resuscitation for predicting good neurological outcome in patients with out-of-hospital cardiac arrest: a propensity-matched study. Crit Care. 2014; 18:535. PMID: 25255842.
Article24. Nagao K, Nonogi H, Yonemoto N, et al. Duration of prehospital resuscitation efforts after out-of-hospital cardiac arrest. Circulation. 2016; 133:1386–1396. PMID: 26920493.
Article25. Jo IJ, Shin TG, Sim MS, et al. Outcome of in-hospital adult cardiopulmonary resuscitation assisted with portable auto-priming percutaneous cardiopulmonary support. Int J Cardiol. 2011; 151:12–17. PMID: 20471704.
Article26. Fagnoul D, Combes A, De Backer D. Extracorporeal cardiopulmonary resuscitation. Curr Opin Crit Care. 2014; 20:259–265. PMID: 24785674.
Article27. Soar J, Nolan JP, Böttiger BW, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation. 2015; 95:100–147. PMID: 26477701.28. Maclaren G, Pasquali SK, Dalton HJ. Volume-outcome relationships in extracorporeal membrane oxygenation: is bigger really better? Crit Care Med. 2014; 42:726–727. PMID: 24534958.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Key Factors in Improving Clinical Outcomes in Patients with Cardiac Arrest Undergoing Extracorporeal Cardiopulmonary Resuscitation: a Multidisciplinary Team Approach
- Effectiveness of a Cardiopulmonary Resuscitation Team with an Emergency Physician for In-Hospital Cardiac Arrest
- Role of extracorporeal cardiopulmonary resuscitation in adults
- Intracranial Hemorrhage Identified in the Early Stage after Applying Extracorporeal Membrane Oxygenation to Support Cardiopulmonary Resuscitation
- Benefits, key protocol components, and considerations for successful implementation of extracorporeal cardiopulmonary resuscitation: a review of the recent literature