Acute Crit Care.
2020 Feb;35(1):1-9. 10.4266/acc.2020.00080.
Role of extracorporeal cardiopulmonary resuscitation in adults
- Affiliations
-
- 1Department of Thoracic and Cardiovascular surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2500944
- DOI: http://doi.org/10.4266/acc.2020.00080
Abstract
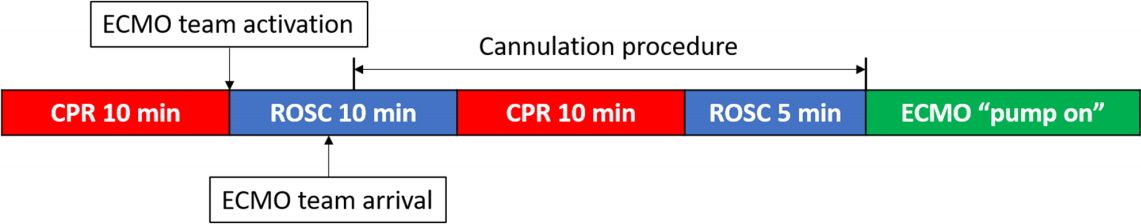
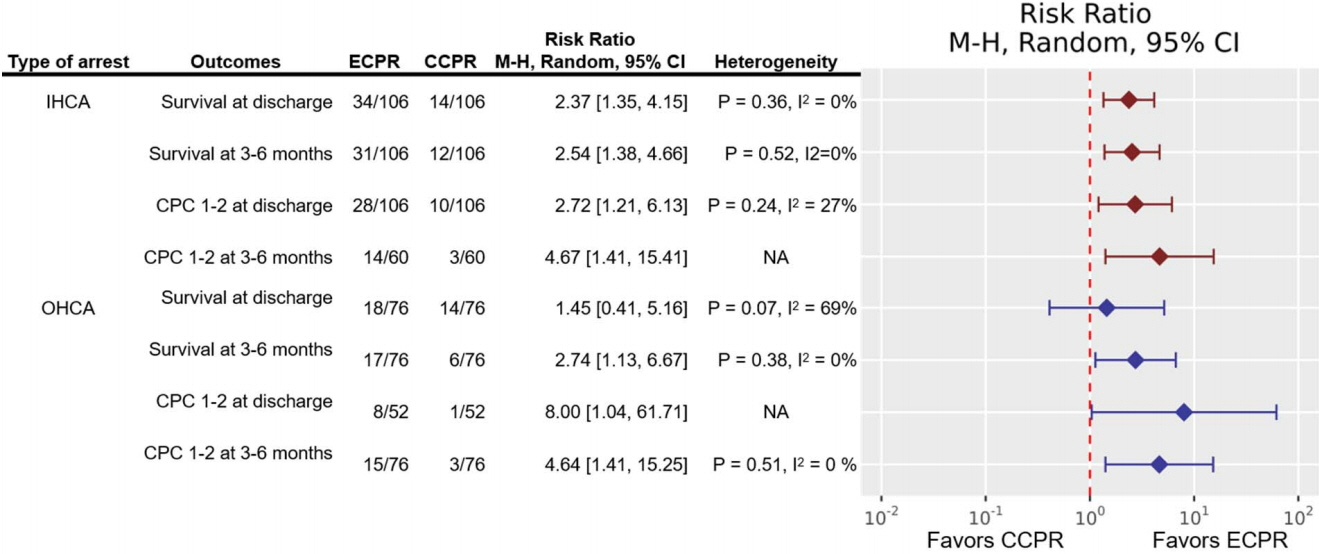
- Extracorporeal cardiopulmonary resuscitation (ECPR) has been performed with increasing frequency worldwide to improve the low survival rate of conventional cardiopulmonary resuscitation (CCPR). Several studies have shown that among patients who experience in-hospital cardiac arrest, better survival outcomes and neurological outcomes can be expected after ECPR than after CCPR. However, studies have not clearly shown a short-term survival benefit of ECPR for patients who experience out-of-hospital cardiac arrest. Favorable outcomes are associated with a shorter low-flow time, an initial shockable rhythm, lower serum lactate levels, higher blood pH, and a lower Sequential Organ Failure Assessment score. Indications for ECPR include young age, witnessed arrest with bystander cardiopulmonary resuscitation, an initial shockable rhythm, correctable causes such as a cardiac etiology, and no return of spontaneous circulation within 10–20 minutes of CCPR. ECPR is a complex intervention that requires a highly trained team, specialized equipment, and multidisciplinary support within a healthcare system, and it has the risk of several life-threatening complications. Therefore, physicians should carefully select patients for ECPR who can gain the most benefit, instead of applying ECPR indiscriminately.
Keyword
Figure
Cited by 1 articles
-
Critical care management of pulmonary arterial hypertension in pregnancy: the pre-, peri- and post-partum stages
Vorakamol Phoophiboon, Monvasi Pachinburavan, Nicha Ruamsap, Natthawan Sanguanwong, Nattapong Jaimchariyatam
Acute Crit Care. 2021;36(4):286-293. doi: 10.4266/acc.2021.00458.
Reference
-
1. Centers for Disease Control and Prevention. Out-of-hospital cardiac arrest surveillance: cardiac arrest registry to enhance survival (CARES). United States, October 1, 2005-December 31, 2010. MMWR 2011;60.2. Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003; 58:297–308.
Article3. Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010; 81:1479–87.
Article4. Kennedy JH. The role of assisted circulation in cardiac resuscitation. JAMA. 1966; 197:615–8.
Article5. Annich GM, Lynch WR, MacLaren G, Wilson JM, Bartlett RH. ECMO: extracorporeal cardiopulmonary support in critical care. Seattle: University of Washington Press;2018.6. Extracorporeal Life Support Organization. ECLS registry report: international summary [Internet]. Ann Arbor (MI): Extracorporeal Life Support Organization;2003. [cited 2020 Feb 25]. Available from: https://www.elso.org/Portals/0/Files/Reports/2017/InternationalSummary January2017.pdf.7. Richardson AS, Schmidt M, Bailey M, Pellegrino VA, Rycus PT, Pilcher DV. ECMO Cardio-Pulmonary Resuscitation (ECPR), trends in survival from an international multicentre cohort study over 12-years. Resuscitation. 2017; 112:34–40.
Article8. Extracorporeal Life Support Organization. ECLS registry report: July, 2019 [Internet]. Ann Arbor (MI): Extracorporeal Life Support Organization;2019. [cited 2020 Feb 25]. Available from: https://www.elso.org/Registry/Statistics/International-Summary.aspx.9. Brooks SC, Anderson ML, Bruder E, Daya MR, Gaffney A, Otto CW, et al. Part 6: alternative techniques and ancillary devices for cardiopulmonary resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015; 132(Suppl 2):S436–43.10. Panchal AR, Berg KM, Hirsch KG, Kudenchuk PJ, Del Rios M, Cabañas JG, et al. 2019 American Heart Association focused update on advanced cardiovascular life support: use of advanced airways, vasopressors, and extracorporeal cardiopulmonary resuscitation during cardiac arrest: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2019; 140:e881–94.
Article11. Kim SJ, Kim HJ, Lee HY, Ahn HS, Lee SW. Comparing extracorporeal cardiopulmonary resuscitation with conventional cardiopulmonary resuscitation: a meta-analysis. Resuscitation. 2016; 103:106–16.
Article12. Twohig CJ, Singer B, Grier G, Finney SJ. A systematic literature review and meta-analysis of the effectiveness of extracorporeal- CPR versus conventional-CPR for adult patients in cardiac arrest. J Intensive Care Soc. 2019; 20:347–57.13. Chen YS, Lin JW, Yu HY, Ko WJ, Jerng JS, Chang WT, et al. Cardiopulmonary resuscitation with assisted extracorporeal lifesupport versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008; 372:554–61.
Article14. Shin TG, Choi JH, Jo IJ, Sim MS, Song HG, Jeong YK, et al. Extracorporeal cardiopulmonary resuscitation in patients with inhospital cardiac arrest: a comparison with conventional cardiopulmonary resuscitation. Crit Care Med. 2011; 39:1–7.
Article15. Maekawa K, Tanno K, Hase M, Mori K, Asai Y. Extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest of cardiac origin: a propensity-matched study and predictor analysis. Crit Care Med. 2013; 41:1186–96.16. Kim SJ, Jung JS, Park JH, Park JS, Hong YS, Lee SW. An optimal transition time to extracorporeal cardiopulmonary resuscitation for predicting good neurological outcome in patients with out-of-hospital cardiac arrest: a propensity-matched study. Crit Care. 2014; 18:535.
Article17. Wengenmayer T, Rombach S, Ramshorn F, Biever P, Bode C, Duerschmied D, et al. Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Crit Care. 2017; 21:157.
Article18. Lee SW, Han KS, Park JS, Lee JS, Kim SJ. Prognostic indicators of survival and survival prediction model following extracorporeal cardiopulmonary resuscitation in patients with sudden refractory cardiac arrest. Ann Intensive Care. 2017; 7:87.
Article19. Ko RE, Ryu JA, Cho YH, Sung K, Jeon K, Suh GY, et al. The differential neurologic prognosis of low-flow time according to the initial rhythm in patients who undergo extracorporeal cardiopulmonary resuscitation. Resuscitation. 2020; 148:121–7.
Article20. Ryu JA, Chung CR, Cho YH, Sung K, Jeon K, Suh GY, et al. Neurologic outcomes in patients who undergo extracorporeal cardiopulmonary resuscitation. Ann Thorac Surg. 2019; 108:749–55.
Article21. D’Arrigo S, Cacciola S, Dennis M, Jung C, Kagawa E, Antonelli M, et al. Predictors of favourable outcome after in-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation: a systematic review and meta-analysis. Resuscitation. 2017; 121:62–70.
Article22. Debaty G, Babaz V, Durand M, Gaide-Chevronnay L, Fournel E, Blancher M, et al. Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest: a systematic review and metaanalysis. Resuscitation. 2017; 112:1–10.
Article23. Riou B, Adnet F, Baud F, Cariou A, Carli P, Combes A, et al. Recommandations sur les indications de l’assistance circulatoire dans le traitement des arrêts cardiaques réfractaires. Ann Fr Anesth Reanim. 2009; 28:182–6.24. Michels G, Wengenmayer T, Hagl C, Dohmen C, Böttiger BW, Bauersachs J, et al. Recommendations for extracorporeal cardiopulmonary resuscitation (eCPR): consensus statement of DGIIN, DGK, DGTHG, DGfK, DGNI, DGAI, DIVI and GRC. Clin Res Cardiol. 2019; 108:455–64.
Article25. Sulzgruber P, Sterz F, Poppe M, Schober A, Lobmeyr E, Datler P, et al. Age-specific prognostication after out-of-hospital cardiac arrest: the ethical dilemma between ‘life-sustaining treatment’ and ‘the right to die’ in the elderly. Eur Heart J Acute Cardiovasc Care. 2017; 6:112–20.26. Yannopoulos D, Bartos JA, Raveendran G, Conterato M, Frascone RJ, Trembley A, et al. Coronary artery disease in patients with out-of-hospital refractory ventricular fibrillation cardiac arrest. J Am Coll Cardiol. 2017; 70:1109–17.27. Lamhaut L, Hutin A, Puymirat E, Jouan J, Raphalen JH, Jouffroy R, et al. A pre-hospital extracorporeal cardio pulmonary resuscitation (ECPR) strategy for treatment of refractory out hospital cardiac arrest: an observational study and propensity analysis. Resuscitation. 2017; 117:109–17.
Article28. Lamhaut L, Jouffroy R, Soldan M, Phillipe P, Deluze T, Jaffry M, et al. Safety and feasibility of prehospital extra corporeal life support implementation by non-surgeons for out-of-hospital refractory cardiac arrest. Resuscitation. 2013; 84:1525–9.
Article29. Bol ME, Suverein MM, Lorusso R, Delnoij TS, Brandon Bravo Bruinsma GJ, Otterspoor L, et al. Early initiation of extracorporeal life support in refractory out-of-hospital cardiac arrest: design and rationale of the INCEPTION trial. Am Heart J. 2019; 210:58–68.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracranial Hemorrhage Identified in the Early Stage after Applying Extracorporeal Membrane Oxygenation to Support Cardiopulmonary Resuscitation
- Venovenous and Venoarterial Extracorporeal Membrane Oxygenation for Repeated Life Threatening Hemoptysis: A case report
- Extracorporeal Cardiopulmonary Resuscitation in Infants: Outcomes and Predictors of Mortality
- Successful Resuscitation of Prolonged Cardiac Arrest Using Emergency Extracorporeal Membrane Oxygenator: A case report
- Clinical Significance of Low-flow Time in Patients Treated with Extracorporeal Cardiopulmonary Resuscitation