Neurointervention.
2021 Nov;16(3):267-274. 10.5469/neuroint.2021.00269.
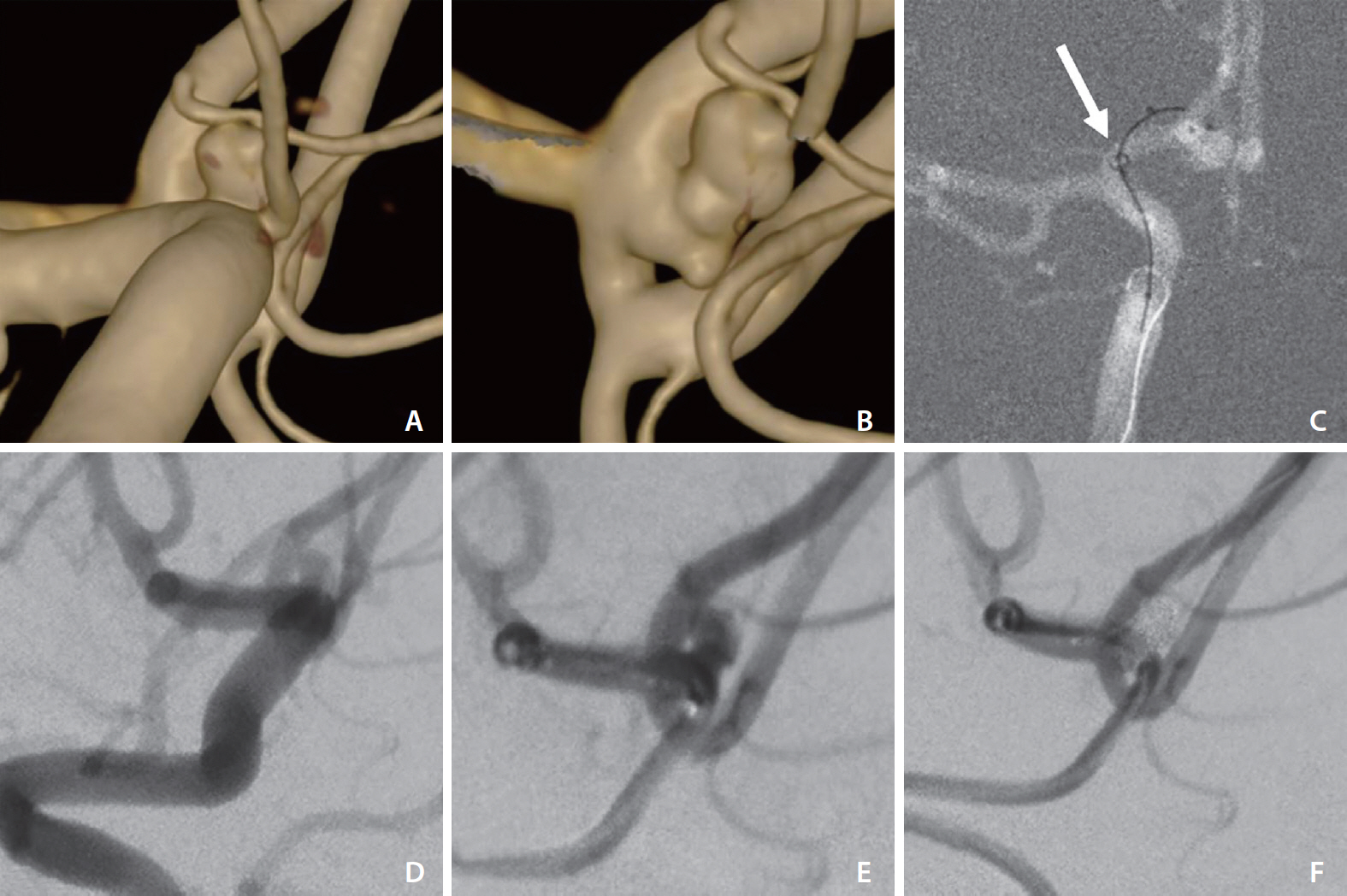
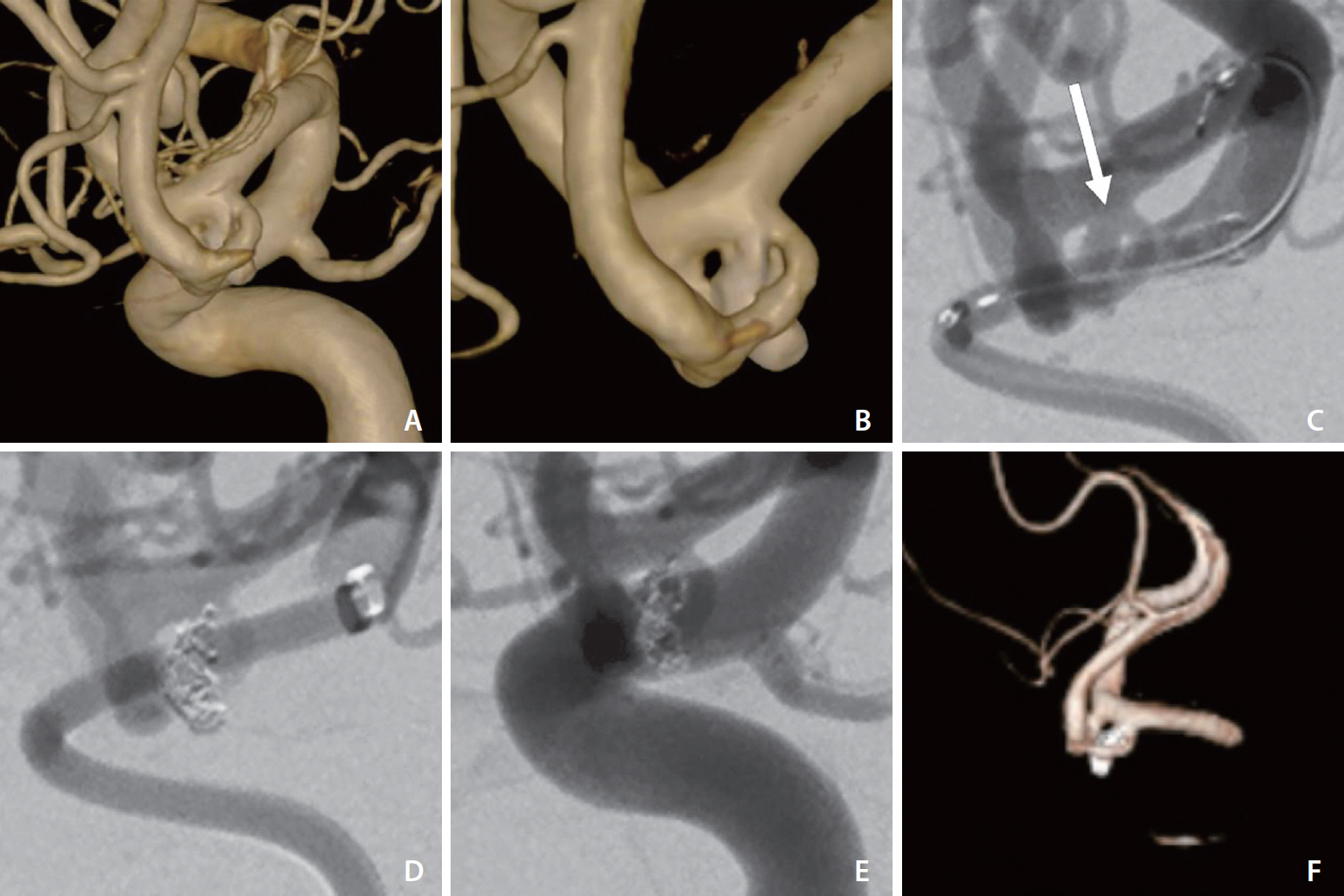
Use of Distal Intracranial Catheters for Better Working View of Cerebral Aneurysms Hidden by Parent Artery or Its Branches: A Technical Note
- Affiliations
-
- 1Department of Surgical Sciences, Uppsala University Hospital, Uppsala, Sweden
- KMID: 2522041
- DOI: http://doi.org/10.5469/neuroint.2021.00269
Abstract
- A good working view is critical for safe and successful endovascular treatment of cerebral aneurysms. In a few cases, endovascular treatment of cerebral aneurysms may be challenging due to difficulty in obtaining a proper working view. In this report of 6 cases, we described the advantage of using a distal intracranial catheter (DIC) to achieve better visualization of cerebral aneurysms hidden by a parent artery or its branches. Between September 2017 and January 2021, we treated 390 aneurysms with endovascular techniques. In 6 cases in which it was difficult to obtain a proper working view, the DIC was placed distally close to the aneurysm in order to remove the parent artery projection from the working view and obtain better visualization of the aneurysm. Clinical and procedural outcomes and complications were evaluated. The position of the DIC was above the internal carotid artery siphon in the 6 cases. All aneurysms were successfully embolized. Raymond–Roy class 1 occlusion was achieved in all 4 unruptured aneurysms, while the result was class 2 in the 2 ruptured aneurysms. Placement of the DIC was atraumatic without dissections or significant catheter-induced vasospasm in all patients. Transient dysphasia was seen in 2 cases and transient aphasia in 1. Using this technique, we have found it possible to better visualize the aneurysm sac or neck and thereby treat cases we otherwise would have considered untreatable.
Keyword
Figure
Reference
-
1. Fargen KM, Singh J, Wilson JA, Wolfe SQ. Unassisted aneurysm coil embolization. In : Spiotta AM, Turner RD, Chaudry MI, Turk AS, editors. Management of cerebrovascular disorders: a comprehensive, multidisciplinary approach. Cham: Springer;2019. p. 143–160.2. Anxionnat R, Bracard S, Ducrocq X, Trousset Y, Launay L, Kerrien E, et al. Intracranial aneurysms: clinical value of 3D digital subtraction angiography in the therapeutic decision and endovascular treatment. Radiology. 2001; 218:799–808.
Article3. Rossitti S, Pfister M. 3D road-mapping in the endovascular treatment of cerebral aneurysms and arteriovenous malformations. Interv Neuroradiol. 2009; 15:283–290.
Article4. Lin LM, Colby GP, Huang J, Tamargo RJ, Coon AL. Ultra-distal large-bore intracranial access using the hyperflexible Navien distal intracranial catheter for the treatment of cerebrovascular pathologies: a technical note. J Neurointerv Surg. 2014; 6:301–307.
Article5. Jindal G, Giacon L, Iyoha M, Miller T, Aldrich F, Simard M, et al. Navien catheter experience in neuroendovascular interventions. Interv Neuroradiol. 2017; 23:551–555.
Article6. Chandran A, Puthuran M, Eldridge PR, Nahser HC. Distal access using hyperflexible atraumatic distal tip with optimized proximal stability of the Benchmark intracranial guide catheter for the treatment of cerebral vascular diseases: a technical note. J Neurointerv Surg. 2016; 8:718–721.
Article7. Hauck EF, Tawk RG, Karter NS, Binning MJ, Khalessi AA, Natarajan SK, et al. Use of the outreach distal access catheter as an intracranial platform facilitates coil embolization of select intracranial aneurysms: technical note. J Neurointerv Surg. 2011; 3:172–176.
Article8. Binning MJ, Yashar P, Orion D, Hauck EF, Levy EI, Hopkins LN, et al. Use of the Outreach Distal Access Catheter for microcatheter stabilization during intracranial arteriovenous malformation embolization. AJNR Am J Neuroradiol. 2012; 33:E117–E119.
Article9. Matsushige T, Sakamoto S, Ishii D, Shinagawa K, Shimonaga K, Hosogai M, et al. Safety and efficacy of a new outreach distal access catheter, TACTICS, for coil embolization of unruptured intracranial aneurysms. Interv Neuroradiol. 2018; 24:482–488.
Article10. Spiotta AM, Hussain MS, Sivapatham T, Bain M, Gupta R, Moskowitz SI, et al. The versatile distal access catheter: the Cleveland Clinic experience. Neurosurgery. 2011; 68:1677–1686. discussion 1686.
Article11. Turk A, Manzoor MU, Nyberg EM, Turner RD, Chaudry I. Initial experience with distal guide catheter placement in the treatment of cerebrovascular disease: clinical safety and efficacy. J Neurointerv Surg. 2013; 5:247–252.
Article12. Lee S, Gong TS, Lee YW, Kim HJ, Kweon CY. The benefits of Navien™ intracranial support catheter for endovascular treatment. J Cerebrovasc Endovasc Neurosurg. 2016; 18:234–238.
Article13. Chaudhary N, Pandey AS, Thompson BG, Gandhi D, Ansari SA, Gemmete JJ. Utilization of the Neuron 6 French 0.053 inch inner luminal diameter guide catheter for treatment of cerebral vascular pathology: continued experience with ultra distal access into the cerebral vasculature. J Neurointerv Surg. 2012; 4:301–306.
Article14. Mascitelli JR, Moyle H, Oermann EK, Polykarpou MF, Patel AA, Doshi AH, et al. An update to the Raymond-Roy occlusion classification of intracranial aneurysms treated with coil embolization. J Neurointerv Surg. 2015; 7:496–502.
Article15. Andaluz N, Zuccarello M. Treatment strategies for complex intracranial aneurysms: review of a 12-year experience at the University of Cincinnati. Skull Base. 2011; 21:233–242.
Article16. Möhlenbruch MA, Kabbasch C, Kowoll A, Broussalis E, Sonnberger M, Müller M, et al. Multicenter experience with the new SOFIA Plus catheter as a primary local aspiration catheter for acute stroke thrombectomy. J Neurointerv Surg. 2017; 9:1223–1227.
Article17. Sallustio F, Pampana E, Davoli A, Merolla S, Koch G, Alemseged F, et al. Mechanical thrombectomy of acute ischemic stroke with a new intermediate aspiration catheter: preliminary results. J Neurointerv Surg. 2018; 10:975–977.
Article18. Lin LM, Colby GP, Iyer RR, Jiang B, Huang J, Tamargo RJ, et al. Pentaxial access platform for ultra-distal intracranial delivery of a large-bore hyperflexible DIC (distal intracranial catheter): a technical note. Interdiscip Neurosurg. 2016; 6:29–34.
Article19. Harada Y, Kairamkonda SR, Ilyas U, Pothineni NVK, Samant RS, Shah VA, et al. Pearls & Oy-sters: contrast-induced encephalopathy following coronary angiography: a rare stroke mimic. Neurology. 2020; 94:e2491–e2494.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Aneurysms of the Distal Anterior Cerebral Artery: Case Report
- Z-Shaped Microcatheter Tip Shaping for Embolization of Aneurysms at the Proximal A1 Segment of the Anterior Cerebral Artery: A Technical Note
- Diagnosis and Treatment of Intracranial Aneurysms with 3-dimensional Digital Subtraction Angiography
- Multiple Intracranial Aneurysms: A Case Report of Patient with Nine Multiple Intracranial Aneurysms
- Experience of Endovascular Treatment of Distal Posterior Cerebral Artery Aneurysms