J Korean Neurosurg Soc.
2021 Nov;64(6):913-921. 10.3340/jkns.2021.0011.
Analyzing the Significance of T1 Slope minus Cervical Lordosis in Patients with Anterior Cervical Discectomy and Fusion Surgery
- Affiliations
-
- 1Department of Neurosurgery, St. Vincent Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- 2Department of Neurosurgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2521981
- DOI: http://doi.org/10.3340/jkns.2021.0011
Abstract
Objective
: Accurate measurement of T1 slope (a component of T1s minus cervical lordosis [CL]) is often constrained by anatomical limitations. In this situation, efforts should be made to find the exact meaning of T1s-CL and whether there are any alternatives to it.
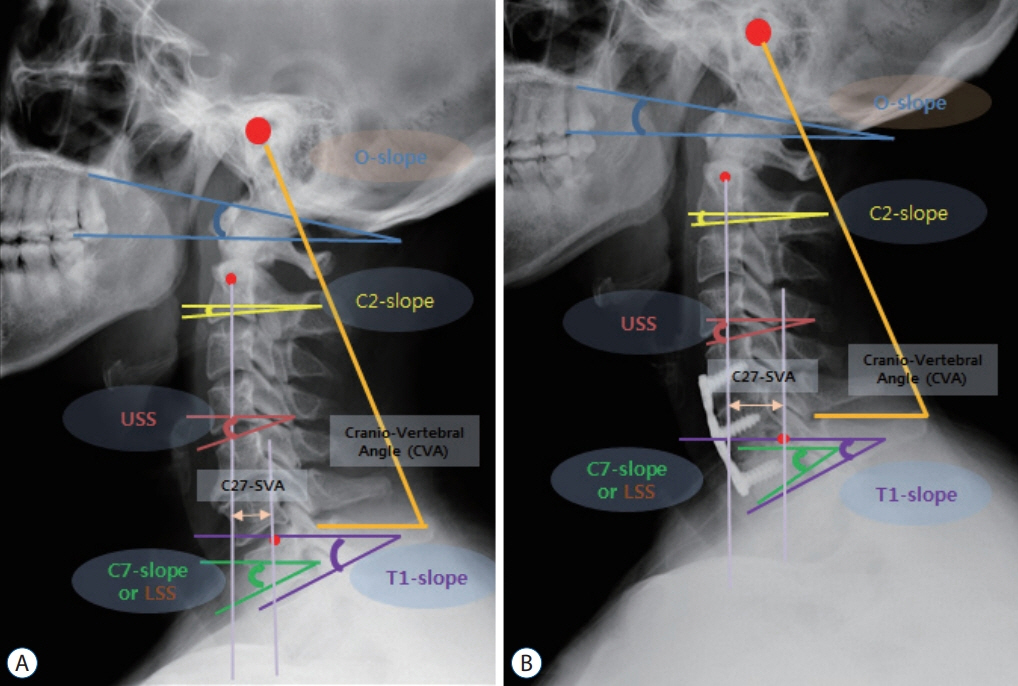
Methods
: We enrolled 117 patients who received two-level anterior cervical discectomy and fusion (ACDF). Occipital slope, C2 slope (C2s), C7 slope (C7s), T1, O-C2 angle (O-C2A), C2-7 angle (C2-7A), O-C7 angle (O-C7A), T1s-CL, C7-T1 angle (C7-T1A), and C2-7 sagittal vertical axis were measured. We determined 16° (T1s-CL) as the reference point for dividing subjects into the mismatch group and the balance group, and a comparative analysis was performed.
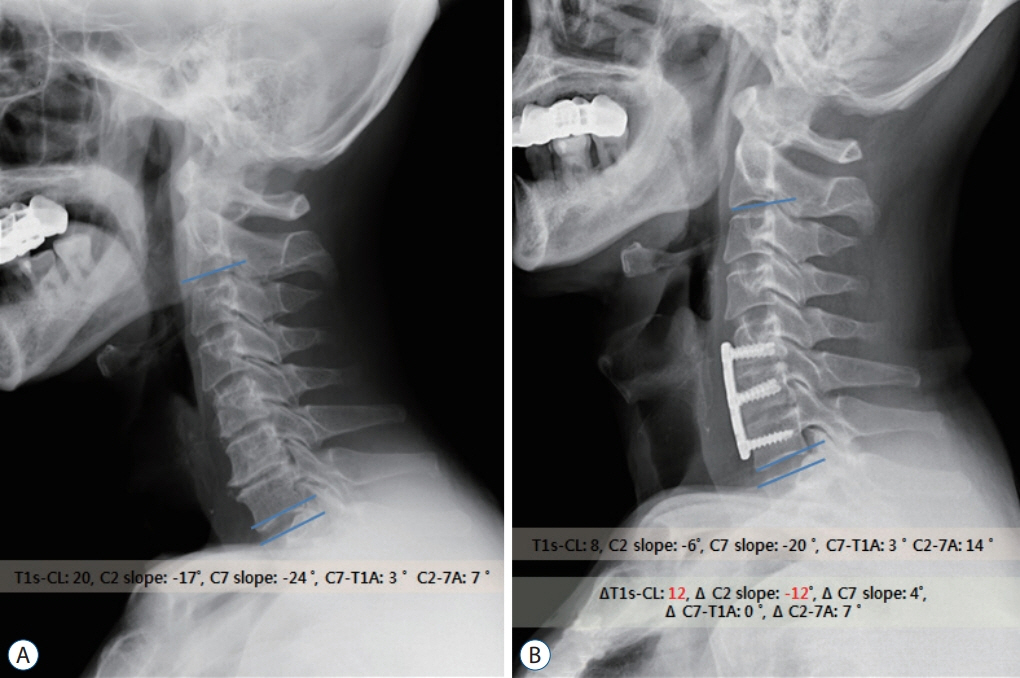
Results
: The mean value of C7-T1A was constantly maintained within 2.6° peri-operatively. In addition, C2s and T1s-CL showed the same absolute change (Δ|0.8|°). The mean values of T1s-CL of the mismatch and balance groups were 23.0° and 7.6°, respectively. The five factors with the largest differences between the two groups were as follows : C2s (Δ13.3°), T1s-CL (Δ15.4°), O-C2A (Δ8.7°), C2-7A (Δ14.7°), and segmental angle (Δ7.9°) before surgery. Only four factors showed statistically significant change between the two groups after ACDF : T1s-CL (Δ4.0° vs. Δ0.2°), C2s (Δ3.2° vs. Δ0.7°), O-C2A (Δ2.6° vs. Δ1.3°), C2-7A (Δ6.3° vs. Δ1.3°). A very strong correlation between T1s-CL and C2s was also found (r=|0.88–0.96|).
Conclusion
: C2s itself may be the essential key to represent T1s-CL. The amounts and directions of change of these two factors (T1s-CL and C2s) were also almost identical. The above phenomenon was re-confirmed once again through the correlation analysis.
Keyword
Figure
Reference
-
References
1. Ajello M, Marengo N, Pilloni G, Penner F, Vercelli G, Pecoraro F, et al. Is it possible to evaluate the ideal cervical alignment for each patient needing surgery? An easy rule to determine the appropriate crvical lordosis in preoperative planning. World Neurosurg. 97:471–478. 2017.
Article2. Diebo BG, Challier V, Henry JK, Oren JH, Spiegel MA, Vira S, et al. Predicting cervical alignment required to maintain horizontal gaze based on global spinal alignment. Spine (Phila Pa 1976). 41:1795–1800. 2016.
Article3. Gillis CC, Kaszuba MC, Traynelis VC. Cervical radiographic parameters in 1- and 2-level anterior cervical discectomy and fusion. J Neurosurg Spine. 25:421–429. 2016.
Article4. Ha Y, Schwab F, Lafage V, Mundis G, Shaffrey C, Smith J, et al. Reciprocal changes in cervical spine alignment after corrective thoracolumbar deformity surgery. Eur Spine J. 23:552–559. 2014.
Article5. Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Relationship between T1 slope and cervical alignment following multilevel posterior cervical fusion surgery: impact of T1 slope minus cervical lordosis. Spine (Phila Pa 1976). 41:E396–E402. 2016.6. Jenkins LA, Capen DA, Zigler JE, Nelson RW, Nagelberg S. Cervical spine fusions for trauma. A long-term radiographic and clinical evaluation. Orthop Rev. Suppl:13–19. 1994.7. Kawakami M, Tamaki T, Yoshida M, Hayashi N, Ando M, Yamada H. Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. J Spinal Disord. 12:50–56. 1999.
Article8. Kim HJ, Choi BW, Park J, Pesenti S, Lafage V. Anterior cervical discectomy and fusion can restore cervical sagittal alignment in degenerative cervical disease. Eur J Orthop Surg Traumatol. 29:767–774. 2019.
Article9. Kim JH, Park JY, Yi S, Kim KH, Kuh SU, Chin DK, et al. Anterior cervical discectomy and fusion alters whole-spine sagittal alignment. Yonsei Med J. 56:1060–1070. 2015.
Article10. Kim JT, Lee HJ, Choi DY, Shin MH, Hong JT. Sequential alignment change of the cervical spine after anterior cervical discectomy and fusion in the lower cervical spine. Eur Spine J. 25:2223–2232. 2016.
Article11. Kwon WK, Kim PS, Ahn SY, Song JY, Kim JH, Park YK, et al. Analysis of associating factors with C2-7 sagittal vertical axis after two-level anterior cervical fusion: comparison between plate augmentation and standalone cages. Spine (Phila Pa 1976). 42:318–325. 2017.
Article12. Lan Z, Huang Y, Xu W. Relationship between T1 slope minus C2-7 lordosis and cervical alignment parameters after adjacent 2-level anterior cervical diskectomy and fusion of lower cervical spine. World Neurosurg. 122:e1195–e1201. 2019.
Article13. Lau D, DiGiorgio AM, Chan AK, Dalle Ore CL, Virk MS, Chou D, et al. Applicability of cervical sagittal vertical axis, cervical lordosis, and T1 slope on pain and disability outcomes after anterior cervical discectomy and fusion in patients without deformity. J Neurosurg Spine. 18:1–8. 2019.
Article14. Lee HJ, Kim JH, Kim IS, Hong JT. Physiologic cervical alignment change between whole spine radiographs and normal standing cervical radiographs. World Neurosurg. 122:e1222–e1227. 2019.
Article15. Lee SH, Son ES, Seo EM, Suk KS, Kim KT. Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J. 15:705–712. 2015.
Article16. Ling FP, Chevillotte T, Leglise A, Thompson W, Bouthors C, Le Huec JC. Which parameters are relevant in sagittal balance analysis of the cervical spine? A literature review. Eur Spine J. 27:8–15. 2018.
Article17. Naderi S, Ozgen S, Pamir MN, Ozek MM, Erzen C. Cervical spondylotic myelopathy: surgical results and factors affecting prognosis. Neurosurgery. 43:43–49. discussion 49-50. 1998.
Article18. Oe S, Togawa D, Nakai K, Yamada T, Arima H, Banno T, et al. The influence of age and sex on cervical spinal alignment among volunteers aged over 50. Spine (Phila Pa 1976). 40:1487–1494. 2015.
Article19. Smith JS, Shaffrey CI, Lafage V, Blondel B, Schwab F, Hostin R, et al. Spontaneous improvement of cervical alignment after correction of global sagittal balance following pedicle subtraction osteotomy. J Neurosurg Spine. 17:300–307. 2012.
Article20. Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP. The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine (Phila Pa 1976). 34:2886–2892. 2009.
Article21. Staub BN, Lafage R, Kim HJ, Shaffrey CI, Mundis GM, Hostin R, et al. Cervical mismatch: the normative value of T1 slope minus cervical lordosis and its ability to predict ideal cervical lordosis. J Neurosurg Spine. 30:31–37. 2018.
Article22. Tamai K, Buser Z, Paholpak P, Sessumpun K, Nakamura H, Wang JC. Can C7 slope substitute the T1 slope?: an analysis using cervical radiographs and kinematic MRIs. Spine (Phila Pa 1976). 43:520–525. 2018.23. Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 76 Suppl. 1:S14–S21. discussion S21. 2015.
Article24. Villavicencio AT, Babuska JM, Ashton A, Busch E, Roeca C, Nelson EL, et al. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery. 68:1309–1316. discussion 1316. 2011.
Article25. Wang Q, Wang XT, Zhu L, Wei YX. Thoracic inlet parameters for degenerative cervical spondylolisthesis imaging measurement. Med Sci Monit. 24:2025–2030. 2018.
Article26. Weng C, Wang J, Tuchman A, Wang J, Fu C, Hsieh PC, et al. Influence of T1 slope on the cervical sagittal balance in degenerative cervical spine: an analysis using kinematic MRI. Spine (Phila Pa 1976). 41:185–190. 2016.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Late Results of Anterior Cervical Discectomy and Fusion with Interbody Cages
- Comparative Study of Clinical Outcomes of Anterior Cervical Discectomy and Fusion Using Autobone Graft or Cage with Bone Substitute
- The Effect of Cervical Lordosis on Cervical Disc Degeneration in Patients with a High T1 Slope
- Clinical Results from Subsidence and Loss of Lordosis after Anterior Cervical Discectomy and Fusion
- Total Cervical Disc Replacement using Artificial Disc in Cervical Disc Herniations