Ann Surg Treat Res.
2021 Nov;101(5):306-313. 10.4174/astr.2021.101.5.306.
Clinical comparison between the presence and absence of protein plugs in pediatric choledochal cysts: experience in 390 patients over 30 years in a single center
- Affiliations
-
- 1Department of Pediatric Surgery, Korea University College of Medicine, Seoul, Korea
- 2Department of Pediatric Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2521853
- DOI: http://doi.org/10.4174/astr.2021.101.5.306
Abstract
- Purpose
The incidence of choledochal cyst (CC) with protein plugs is between 15.5%–40.4%. However, studies on CCs with protein plugs in children are limited. We aimed to analyze the clinical features, surgical findings, and complications of pediatric CCs with and without protein plugs.
Methods
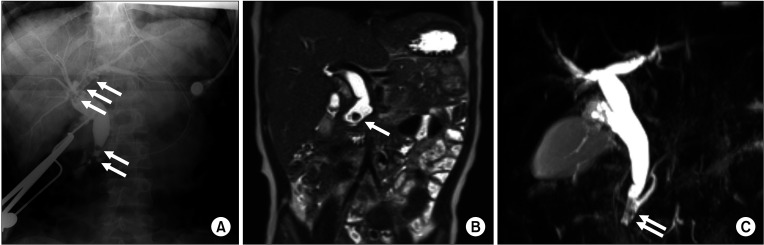
We retrospectively analyzed 390 patients who underwent surgery for CCs between January 1987 and September 2017. The patients were divided into 2 groups: groups A (CC with protein plugs) and B (CC without protein plugs). The presence of protein plugs was evaluated using preoperative images or identified during surgery.
Results
One hundred forty-two (36.4%) patients had protein plugs in the pancreaticobiliary duct. The most common initial clinical presentation was abdominal pain, and its incidence was significantly higher in group A (66.2%) than in group B (54.8%) (P = 0.032). The incidence of accompanying pancreatitis was also significantly higher in group A (37.3% vs. 27.0%) (P = 0.040). Anomalous pancreaticobiliary ductal union (APBDU) was found in 261 patients (66.9%) and its incidence was significantly higher in group A (74.6% vs. 62.5%) (P = 0.014). Most protein plugs were found in the cyst (88.0%) and common channel (31.7%). The incidence of early complications was higher in group A; conversely, that of late complications did not differ.
Conclusion
Approximately 36.4% of the pediatric CC patients were accompanied by protein plugs. Abdominal pain, pancreatitis, and APBDU were more commonly observed among those with protein plugs than among those without; longterm complications did not differ between them.
Keyword
Figure
Reference
-
1. Ryu HS, Lee JY, Kim DY, Kim SC, Namgoong JM. Minimally-invasive neonatal surgery: laparoscopic excision of choledochal cysts in neonates. Ann Surg Treat Res. 2019; 97:21–26. PMID: 31297349.
Article2. Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 2 of 3: diagnosis. Can J Surg. 2009; 52:506–511. PMID: 20011188.3. Hung MH, Lin LH, Chen DF, Huang CS. Choledochal cysts in infants and children: experiences over a 20-year period at a single institution. Eur J Pediatr. 2011; 170:1179–1185. PMID: 21350805.
Article4. Lipsett PA, Pitt HA. Surgical treatment of choledochal cysts. J Hepatobiliary Pancreat Surg. 2003; 10:352–359. PMID: 14598135.
Article5. Lai HS, Duh YC, Chen WJ, Chen CC, Hung WT, Lee PH, et al. Manifestations and surgical treatment of choledochal cyst in different age group patients. J Formos Med Assoc. 1997; 96:242–246. PMID: 9136509.6. Huang CS, Huang CC, Chen DF. Choledochal cysts: differences between pediatric and adult patients. J Gastrointest Surg. 2010; 14:1105–1110. PMID: 20422306.
Article7. Kaneko K, Ando H, Ito T, Watanabe Y, Seo T, Harada T, et al. Protein plugs cause symptoms in patients with choledochal cysts. Am J Gastroenterol. 1997; 92:1018–1021. PMID: 9177522.8. Komuro H, Makino SI, Yasuda Y, Ishibashi T, Tahara K, Nagai H. Pancreatic complications in choledochal cyst and their surgical outcomes. World J Surg. 2001; 25:1519–1523. PMID: 11775184.
Article9. Fujishiro J, Masumoto K, Urita Y, Shinkai T, Gotoh C. Pancreatic complications in pediatric choledochal cysts. J Pediatr Surg. 2013; 48:1897–1902. PMID: 24074664.
Article10. Guelrud M, Morera C, Rodriguez M, Prados JG, Jaén D. Normal and anomalous pancreaticobiliary union in children and adolescents. Gastrointest Endosc. 1999; 50:189–193. PMID: 10425411.
Article11. Kim MJ, Han SJ, Yoon CS, Kim JH, Oh JT, Chung KS, et al. Using MR cholangiopancreatography to reveal anomalous pancreaticobiliary ductal union in infants and children with choledochal cysts. AJR Am J Roentgenol. 2002; 179:209–214. PMID: 12076938.
Article12. Saito T, Terui K, Mitsunaga T, Nakata M, Yoshida H. Significance of imaging modalities for preoperative evaluation of the pancreaticobiliary system in surgery for pediatric choledochal cyst. J Hepatobiliary Pancreat Sci. 2016; 23:347–352. PMID: 26994400.
Article13. Morinville VD, Husain SZ, Bai H, Barth B, Alhosh R, Durie PR, et al. Definitions of pediatric pancreatitis and survey of present clinical practices. J Pediatr Gastroenterol Nutr. 2012; 55:261–265. PMID: 22357117.
Article14. Suzuki M, Shimizu T, Kudo T, Suzuki R, Ohtsuka Y, Yamashiro Y, et al. Usefulness of nonbreath-hold 1-shot magnetic resonance cholangiopancreatography for the evaluation of choledochal cyst in children. J Pediatr Gastroenterol Nutr. 2006; 42:539–544. PMID: 16707978.
Article15. Kaneko K, Ando H, Seo T, Ono Y, Tainaka T, Sumida W. Proteomic analysis of protein plugs: causative agent of symptoms in patients with choledochal cyst. Dig Dis Sci. 2007; 52:1979–1986. PMID: 17415647.
Article16. Guy O, Robles-Diaz G, Adrich Z, Sahel J, Sarles H. Protein content of precipitates present in pancreatic juice of alcoholic subjects and patients with chronic calcifying pancreatitis. Gastroenterology. 1983; 84:102–107. PMID: 6401181.
Article17. Mariani A, Bernard JP, Provansal-Cheylan M, Nitsche S, Sarles H. Differences of pancreatic stone morphology and content in patients with pancreatic lithiasis. Dig Dis Sci. 1991; 36:1509–1516. PMID: 19160597.
Article18. Lee BI, Mustafi D, Cho W, Nakagawa Y. Characterization of calcium binding properties of lithostathine. J Biol Inorg Chem. 2003; 8:341–347. PMID: 12589570.
Article19. Patard L, Lallemand JY, Stoven V. An insight into the role of human pancreatic lithostathine. JOP. 2003; 4:92–103. PMID: 12629266.20. Diao M, Li L, Cheng W. Congenital biliary dilatation may consist of 2 disease entities. J Pediatr Surg. 2011; 46:1503–1509. PMID: 21843715.
Article21. Sugiyama M, Atomi Y, Kuroda A. Pancreatic disorders associated with anomalous pancreaticobiliary junction. Surgery. 1999; 126:492–497. PMID: 10486601.
Article22. Komi N, Takehara H, Kunitomo K, Miyoshi Y, Yagi T. Does the type of anomalous arrangement of pancreaticobiliary ducts influence the surgery and prognosis of choledochal cyst? J Pediatr Surg. 1992; 27:728–731. PMID: 1306647.
Article23. Saito T, Terui K, Mitsunaga T, Nakata M, Kuriyama Y, Higashimoto Y, et al. Role of pediatric endoscopic retrograde cholangiopancreatography in an era stressing less-invasive imaging modalities. J Pediatr Gastroenterol Nutr. 2014; 59:204–209. PMID: 24762457.
Article24. Soares KC, Goldstein SD, Ghaseb MA, Kamel I, Hackam DJ, Pawlik TM. Pediatric choledochal cysts: diagnosis and current management. Pediatr Surg Int. 2017; 33:637–650. PMID: 28364277.
Article25. Edil BH, Olino K, Cameron JL. The current management of choledochal cysts. Adv Surg. 2009; 43:221–232. PMID: 19845181.
Article26. Soares KC, Arnaoutakis DJ, Kamel I, Rastegar N, Anders R, Maithel S, et al. Choledochal cysts: presentation, clinical differentiation, and management. J Am Coll Surg. 2014; 219:1167–1180. PMID: 25442379.
Article27. Park DH, Kim MH, Lee SK, Lee SS, Choi JS, Lee YS, et al. Can MRCP replace the diagnostic role of ERCP for patients with choledochal cysts? Gastrointest Endosc. 2005; 62:360–366. PMID: 16111952.
Article28. Terui K, Yoshida H, Kouchi K, Hishiki T, Saito T, Mitsunaga T, et al. Endoscopic sphincterotomy is a useful preoperative management for refractory pancreatitis associated with pancreaticobiliary maljunction. J Pediatr Surg. 2008; 43:495–499. PMID: 18358288.
Article29. Tsuchiya H, Kaneko K, Itoh A, Kawashima H, Ono Y, Tainaka T, et al. Endoscopic biliary drainage for children with persistent or exacerbated symptoms of choledochal cysts. J Hepatobiliary Pancreat Sci. 2013; 20:303–306. PMID: 22581057.
Article30. Wang Q, Moon SB, Zang J, Liu J, Weng H, Wang X, et al. Usefulness of pre-operative endoscopic retrograde cholangiopancreatography in diagnosis and management of forme fruste choledochal cyst in children. ANZ J Surg. 2020; 90:1041–1045. PMID: 31943672.
Article31. Limketkai BN, Chandrasekhara V, Kalloo AN, Okolo PI 3rd. Comparison of performance and safety of endoscopic retrograde cholangiopancreatography across pediatric age groups. Dig Dis Sci. 2013; 58:2653–2660. PMID: 23709156.
Article32. Rosen JD, Lane RS, Martinez JM, Perez EA, Tashiro J, Wagenaar AE, et al. Success and safety of endoscopic retrograde cholangiopancreatography in children. J Pediatr Surg. 2017; 52:1148–1151. PMID: 28188033.
Article33. Keil R, Drábek J, Lochmannová J, Šťovíček J, Koptová P, Wasserbauer M, et al. ERCP in infants, children, and adolescents: different roles of the methods in different age groups. PLoS One. 2019; 14:e0210805. PMID: 30653580.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Choledochal Cyst Associated with Cystic Duct Dilatation: Report of Three Cases
- Comparison of Clinical and Radiologic Findings Between Perforated and Non-Perforated Choledochal Cysts in Children
- A case of choledochal cyst diagnosed and conservatively treated during pregnancy
- Bile Amylase in Pediatric Choledochal Cyst
- Histopathological Study and Expression of Beta-Catenin in Congenital Choledochal Cyst in a Tertiary Care Pediatric Referral Center in South India