Ann Surg Treat Res.
2021 Nov;101(5):299-305. 10.4174/astr.2021.101.5.299.
A multicenter, prospective, randomized clinical trial of marine mussel-inspired adhesive hemostatic materials, InnoSEAL Plus
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Center for Liver Cancer, National Cancer Center, Goyang, Korea
- 3Department of Surgery, Pusan National University Hospital, Busan, Korea
- 4Department of Surgery, Pusan National University Yangsan Hospital, Yangsan, Korea
- 5Good GanaAn Hospital, Busan, Korea
- 6R&D Center, InnoTherapy Inc., Seoul, Korea
- 7Department of Chemistry, Korea Advanced Institute of Science and Technology (KAIST), Daejeon, Korea
- 8Department of Trauma Surgery and Surgical Critical Care, Pusan National University Hospital, Busan, Korea
- 9Department of Surgery, Pusan National University College of Medicine, Busan, Korea
- KMID: 2521852
- DOI: http://doi.org/10.4174/astr.2021.101.5.299
Abstract
- Purpose
InnoSEAL Plus is an adhesive, coagulant-free hemostatic material that mimics the adhesion mechanism of marine mussels. This study reports on the safety and efficacy of InnoSEAL Plus for patients with hemorrhage after hepatectomy despite first-line hemostasis treatments.
Methods
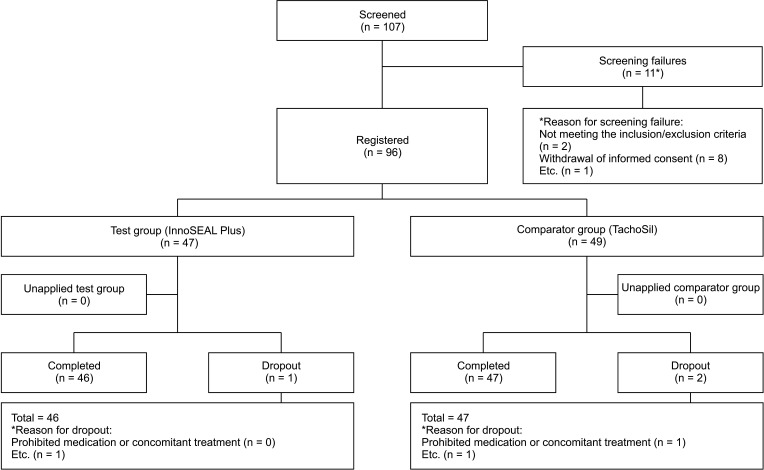
This is a multicenter, prospective, single-blinded, randomized clinical trial involving 96 hepatectomy patients. TachoSil was used as a comparator group. Three-minute and 10-minute hemostatic success rates were monitored. Rebleeding rates were also observed. Safety was assessed by recording all novel undesirable symptoms.
Results
InnoSEAL Plus showed a 3-minute hemostasis rate of 100%, while TachoSil had a rate of 98.0% (48 of 49 patients), demonstrating that the 2 had similar hemostatic efficacies. The difference in efficacy between the test and comparator group was 2.04%, and the lower limit of the one-sided 97.5% confidence interval was –1.92%; as this is greater than the noninferiority limit of –23.9%, the 2 treatments were equivalent. Meanwhile, the 10-minute hemostatic success rate was the same in both groups (100%). No rebleeding occurred in either group. In the safety evaluation, 89 patients experienced adverse events (45 in the test group and 44 in the comparator group). The difference between the 2 groups was not significant. No death occurred after application of the test or comparator group product.
Conclusion
Given that InnoSEAL Plus is a coagulation factor-free product, the hemostasis results are encouraging, especially considering that TachoSil contains a coagulation factor. InnoSEAL Plus was found to be a safe and effective hemostatic material for control of bleeding in hepatectomy patients.
Figure
Reference
-
1. Alfieri S, Carriero C, Caprino P, Di Giorgio A, Sgadari A, Crucitti F, et al. Avoiding early postoperative complications in liver surgery: a multivariate analysis of 254 patients consecutively observed. Dig Liver Dis. 2001; 33:341–346. PMID: 11432513.
Article2. Imamura H, Seyama Y, Kokudo N, Maema A, Sugawara Y, Sano K, et al. One thousand fifty-six hepatectomies without mortality in 8 years. Arch Surg. 2003; 138:1198–1206. PMID: 14609867.
Article3. Kubo S, Takemura S, Yamamoto S, Hai S, Ichikawa T, Kodai S, et al. Risk factors for massive blood loss during liver resection for hepatocellular carcinoma in patients with cirrhosis. Hepatogastroenterology. 2007; 54:830–833. PMID: 17591073.4. Spotnitz WD. Hemostats, sealants, and adhesives: a practical guide for the surgeon. Am Surg. 2012; 78:1305–1321. PMID: 23265118.5. Ding H, Yuan JQ, Zhou JH, Zheng XY, Ye P, Mao C, et al. Systematic review and meta-analysis of application of fibrin sealant after liver resection. Curr Med Res Opin. 2013; 29:387–394. PMID: 23339601.
Article6. Lee H, Dellatore SM, Miller WM, Messersmith PB. Mussel-inspired surface chemistry for multifunctional coatings. Science. 2007; 318:426–430. PMID: 17947576.
Article7. Lee H, Scherer NF, Messersmith PB. Single-molecule mechanics of mussel adhesion. Proc Natl Acad Sci U S A. 2006; 103:12999–13003. PMID: 16920796.
Article8. Kim K, Ryu JH, Koh MY, Yun SP, Kim S, Park JP, et al. Coagulopathy-independent, bioinspired hemostatic materials: a full research story from preclinical models to a human clinical trial. Sci Adv. 2021; 7:eabc9992. PMID: 33762330.
Article9. Genyk Y, Kato T, Pomposelli JJ, Wright JK Jr, Sher LS, Tetens V, et al. Fibrin sealant patch (TachoSil) vs oxidized regenerated cellulose patch (Surgicel Original) for the secondary treatment of local bleeding in patients undergoing hepatic resection: a randomized controlled trial. J Am Coll Surg. 2016; 222:261–268. PMID: 26776356.10. Fischer L, Seiler CM, Broelsch CE, de Hemptinne B, Klempnauer J, Mischinger HJ, et al. Hemostatic efficacy of TachoSil in liver resection compared with argon beam coagulator treatment: an open, randomized, prospective, multicenter, parallel-group trial. Surgery. 2011; 149:48–55. PMID: 20385397.
Article11. Kawasaki S, Origasa H, Tetens V, Kobayashi M. Comparison of TachoSil and TachoComb in patients undergoing liver resection-a randomized, double-blind, non-inferiority trial. Langenbecks Arch Surg. 2017; 402:591–598. PMID: 28365804.
Article12. Zhang C, Fu D, Wang F, Zhong X, Yang L, Wu G, et al. A randomized controlled trial to compare the efficacy of regenerated and non-regenerated oxidized cellulose gauze for the secondary treatment of local bleeding in patients undergoing hepatic resection. Ann Surg Treat Res. 2021; 100:193–199. PMID: 33854988.
Article13. Achneck HE, Sileshi B, Jamiolkowski RM, Albala DM, Shapiro ML, Lawson JH. A comprehensive review of topical hemostatic agents: efficacy and recommendations for use. Ann Surg. 2010; 251:217–228. PMID: 20010084.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical application of a new hemostatic material using mussel-inspired catecholamine hemostat: A pilot study
- Comparison of Hemostatic Effect of Endoscopic Injection with Fibrin Glue (FG) and Hypertonic Saline - epinephrine (HSE) for Peptic Ulcer Bleeding: A prospective randomized trial
- The use of green mussel as bioindicator of heavy metal pollution in Indonesia: a review
- Efficacy of Intra-Articular Injection of Thrombin-Based Hemostatic Agent in the Control of Bleeding after Primary Total Knee Arthroplasty
- Effect of an aluminum chloride hemostatic agent on the dentin shear bond strength of a universal adhesive