Realization of improved outcomes following liver resection in hepatocellular carcinoma patients aged 75 years and older
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Pathology and Translational Genomics, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Surgery, Digestive Disease and Surgery Institute, Cleveland Clinic, Cleveland, OH, USA
- 4Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2521847
- DOI: http://doi.org/10.4174/astr.2021.101.5.257
Abstract
- Purpose
Little is known about liver resection (LR) in hepatocellular carcinoma (HCC) patients older than 75 years of age. This study aimed to compare the postoperative and long-term outcomes of hepatectomy in this patient population according to operation period.
Methods
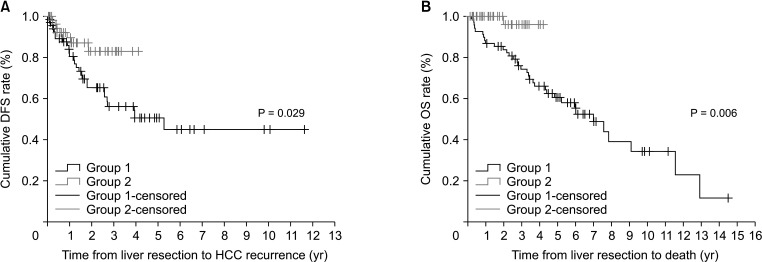
This study included 130 elderly patients who underwent LR for solitary treatment-naïve HCC between November 1998 and March 2020. Group 1 included patients who underwent LR before 2016 (n = 68) and group 2 included those who underwent LR during or after 2016 (n = 62).
Results
The proportion of major LR, anatomical LR, and laparoscopic LR (LLR) in group 1 was significantly lower than those in group 2. Also, the median operation time, amount of blood loss, hospitalization length, rates of intraoperative blood transfusion, and complications in group 2 were less than those in group 1. In the subgroup analysis of group 1, high proteins induced by vitamin K absence or antagonist-II, long hospitalization, and LLR were closely associated with mortality. In the subgroup analysis of group 2, however, none of the factors increased mortality. Nevertheless, the presence of tumor grade 3 or 4 and the incidence of microvascular invasion were higher in group 1 than in group 2, and the disease-free survival and overall survival were better in group 2 than in group 1 because of minimized blood loss and quicker recovery period by increased surgical techniques and anatomical approach, and LLR.
Conclusion
LR in elderly HCC patients has been frequently performed recently, and the outcomes have improved significantly compared to the past.
Figure
Cited by 4 articles
-
Comparing efficacies of different treatment regimens in patients with hepatocellular carcinoma accompanied by portal vein tumor thrombus using network meta-analysis
Seungji Lee, Sung Kyu Song, Byungje Bae, Yongkeun Park
Ann Surg Treat Res. 2022;103(5):280-289. doi: 10.4174/astr.2022.103.5.280.2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma
J Liver Cancer. 2023;23(1):1-120. doi: 10.17998/jlc.2022.11.07.A systematic review and meta-analysis of blood transfusion rates during liver resection by country
Seonju Kim, Yun Kyung Jung, Kyeong Geun Lee, Kyeong Sik Kim, Hanjun Kim, Dongho Choi, Sumi Lee, Boyoung Park
Ann Surg Treat Res. 2023;105(6):404-416. doi: 10.4174/astr.2023.105.6.404.Liver resection in selective hepatocellular carcinoma with Vp3 or Vp4 portal vein tumor thrombosis improves prognosis
Manuel Lim, Jongman Kim, Jinsoo Rhu, Gyu-Seong Choi, Jae-Won Joh
J Liver Cancer. 2024;24(1):102-112. doi: 10.17998/jlc.2024.01.31.
Reference
-
1. Korc-Grodzicki B, Downey RJ, Shahrokni A, Kingham TP, Patel SG, Audisio RA. Surgical considerations in older adults with cancer. J Clin Oncol. 2014; 32:2647–2653. PMID: 25071124.
Article2. Kim YY, Park MS, Aljoqiman KS, Choi JY, Kim MJ. Gadoxetic acid-enhanced magnetic resonance imaging: hepatocellular carcinoma and mimickers. Clin Mol Hepatol. 2019; 25:223–233. PMID: 30661336.
Article3. Torimura T, Iwamoto H. Optimizing the management of intermediate-stage hepatocellular carcinoma: current trends and prospects. Clin Mol Hepatol. 2021; 27:236–245. PMID: 33317248.
Article4. Shin IS, Kim DG, Cha SW, Kang SH, Kim SH, Kim MY, et al. Hepatocellular carcinoma in old age: are there any benefits of liver resection in old age? Ann Surg Treat Res. 2020; 99:65–71. PMID: 32802811.
Article5. Chon YE, Jeong SW, Jun DW. Hepatocellular carcinoma statistics in South Korea. Clin Mol Hepatol. 2021; 27:512–514. PMID: 34153973.
Article6. Kinoshita A, Koike K, Nishino H. Clinical features and prognosis of elderly patients with hepatocellular carcinoma not indicated for surgical resection. Geriatr Gerontol Int. 2017; 17:189–201. PMID: 26847184.
Article7. Frith J, Jones D, Newton JL. Chronic liver disease in an ageing population. Age Ageing. 2009; 38:11–18. PMID: 19029099.
Article8. Cho E, Cho HA, Jun CH, Kim HJ, Cho SB, Choi SK. A review of hepatocellular carcinoma in elderly patients focused on management and outcomes. In Vivo. 2019; 33:1411–1420. PMID: 31471386.
Article9. Caglià P, Tracia A, Buffone A, Amodeo L, Tracia L, Amodeo C, et al. Physiopathology and clinical considerations of laparoscopic surgery in the elderly. Int J Surg. 2016; 33 Suppl 1:S97–S102. PMID: 27255126.
Article10. Kim JM, Kim S, Rhu J, Choi GS, Kwon CH, Joh JW. Elderly hepatocellular carcinoma patients: open or laparoscopic approach? Cancers (Basel). 2020; 12:2281.
Article11. Kim JM, Kwon CH, Joh JW, Park JB, Ko JS, Lee JH, et al. The effect of alkaline phosphatase and intrahepatic metastases in large hepatocellular carcinoma. World J Surg Oncol. 2013; 11:40. PMID: 23432910.
Article12. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.13. Kenkūykai NK. Liver Cancer Study Group of Japan. General rules for the clinical and pathological study of primary liver cancer. 2nd ed. Tokyo: Kanehara & Co.;2003.14. Edmondson HA, Steiner PE. Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer. 1954; 7:462–503. PMID: 13160935.15. Wang YY, Zhong JH, Su ZY, Huang JF, Lu SD, Xiang BD, et al. Albumin-bilirubin versus Child-Pugh score as a predictor of outcome after liver resection for hepatocellular carcinoma. Br J Surg. 2016; 103:725–734. PMID: 27005482.
Article16. Cheng J, Zhao P, Liu J, Liu X, Wu X. Preoperative aspartate aminotransferase-to-platelet ratio index (APRI) is a predictor on postoperative outcomes of hepatocellular carcinoma. Medicine (Baltimore). 2016; 95:e5486. PMID: 27902606.
Article17. Rhu J, Choi GS, Kwon CH, Kim JM, Joh JW. Learning curve of laparoscopic living donor right hepatectomy. Br J Surg. 2020; 107:278–288. PMID: 31652003.
Article18. Kim JM, Kwon CH, Yoo H, Kim KS, Lee J, Kim K, et al. Which approach is preferred in left hepatocellular carcinoma?: laparoscopic versus open hepatectomy using propensity score matching. BMC Cancer. 2018; 18:668. PMID: 29921239.
Article19. Kim JM, Cho BI, Kwon CH, Joh JW, Park JB, Lee JH, et al. Hepatectomy is a reasonable option for older patients with hepatocellular carcinoma. Am J Surg. 2015; 209:391–397. PMID: 25682096.
Article20. Lee N, Cho CW, Kim JM, Choi GS, Kwon CH, Joh JW. Application of temporary inflow control of the Glissonean pedicle method provides a safe and easy technique for totally laparoscopic hemihepatectomy by Glissonean approach. Ann Surg Treat Res. 2017; 92:383–386. PMID: 28480187.
Article21. Hori M, Tanaka M, Ando E, Sakata M, Shimose S, Ohno M, et al. Long-term outcome of elderly patients (75 years or older) with hepatocellular carcinoma. Hepatol Res. 2014; 44:975–982. PMID: 24256493.
Article22. Korean Statistical Information Service. Life expectancy at birth (Korea) [Internet]. Daejeon: Statistics Korea;2019. cited 2021 Jun 10. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPA201&vw_cd=MT_ETITLE&list_id=A41_10&scrId=&seqNo=&language=en&obj_var_id=&itm_id=&conn_path=A6&path=%252Feng%252Fsearch%252FsearchList.do .23. Chen K, Pan Y, Maher H, Zhang B, Zheng XY. Laparoscopic hepatectomy for elderly patients: major findings based on a systematic review and meta-analysis. Medicine (Baltimore). 2018; 97:e11703. PMID: 30045330.24. Tee MC, Chen L, Peightal D, Franko J, Kim PT, Brahmbhatt RD, et al. Minimally invasive hepatectomy is associated with decreased morbidity and resource utilization in the elderly. Surg Endosc. 2020; 34:5030–5040. PMID: 31820156.
Article25. Tranchart H, Gaillard M, Chirica M, Ferretti S, Perlemuter G, Naveau S, et al. Multivariate analysis of risk factors for postoperative complications after laparoscopic liver resection. Surg Endosc. 2015; 29:2538–2544. PMID: 25472746.
Article26. Cho W, Kwon CH, Choi JY, Lee SH, Kim JM, Choi GS, et al. Impact of technical innovation on surgical outcome of laparoscopic major liver resection: 10 years’ experience at a large-volume center. Ann Surg Treat Res. 2019; 96:14–18. PMID: 30603629.
Article27. Yeh MM, Yeung RS, Apisarnthanarax S, Bhattacharya R, Cuevas C, Harris WP, et al. Multidisciplinary perspective of hepatocellular carcinoma: a Pacific Northwest experience. World J Hepatol. 2015; 7:1460–1483. PMID: 26085907.
Article28. Lim TS, Kim JK. Is liver biopsy still useful in the era of non-invasive tests? Clin Mol Hepatol. 2020; 26:302–304. PMID: 32646204.
Article29. Kim JM, Kwon CH, Joh JW, Park JB, Lee JH, Kim SJ, et al. Differences between hepatocellular carcinoma and hepatitis B virus infection in patients with and without cirrhosis. Ann Surg Oncol. 2014; 21:458–465. PMID: 24132624.
Article30. Kim JM, Kwon CH, Joh JW, Park JB, Lee JH, Kim SJ, et al. Outcomes after curative hepatectomy in patients with non-B non-C hepatocellular carcinoma and hepatitis B virus hepatocellular carcinoma from non-cirrhotic liver. J Surg Oncol. 2014; 110:976–981. PMID: 25171344.
Article31. Farges O, Malassagne B, Flejou JF, Balzan S, Sauvanet A, Belghiti J. Risk of major liver resection in patients with underlying chronic liver disease: a reappraisal. Ann Surg. 1999; 229:210–215. PMID: 10024102.32. Wada H, Eguchi H, Nagano H, Kubo S, Nakai T, Kaibori M, et al. Perioperative allogenic blood transfusion is a poor prognostic factor after hepatocellular carcinoma surgery: a multi-center analysis. Surg Today. 2018; 48:73–79. PMID: 28597349.
Article33. Bennett S, Baker LK, Martel G, Shorr R, Pawlik TM, Tinmouth A, et al. The impact of perioperative red blood cell transfusions in patients undergoing liver resection: a systematic review. HPB (Oxford). 2017; 19:321–330. PMID: 28161216.
Article34. Hallet J, Mahar AL, Nathens AB, Tsang ME, Beyfuss KA, Lin Y, et al. The impact of perioperative blood transfusions on short-term outcomes following hepatectomy. Hepatobiliary Surg Nutr. 2018; 7:1–10. PMID: 29531938.
Article35. Zhang Y, Wang R, Yang X. FIB-4 index serves as a noninvasive prognostic biomarker in patients with hepatocellular carcinoma: a meta-analysis. Medicine (Baltimore). 2018; 97:e13696. PMID: 30572498.36. Xun Y, Tian H, Hu L, Yan P, Yang K, Guo T. The impact of perioperative allogeneic blood transfusion on prognosis of hepatocellular carcinoma after radical hepatectomy: a systematic review and meta-analysis of cohort studies. Medicine (Baltimore). 2018; 97:e12911. PMID: 30412094.37. Korean Liver Cancer Association. National Cancer Center. 2018 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Gut Liver. 2019; 13:227–299. PMID: 31060120.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Perspectives of Hepatocellular Carcinoma beyond the Barcelona Clinical Liver Cancer Guideline; Focusing on Liver Resection
- Survival rate of hepatectomy according to liver cirrhosis in hepatoculluar carcinoma
- Hepatocellular Carcinoma Arising in Hepatocellular Adenoma
- Comparison of survival outcomes after anatomical resection and non-anatomical resection in patients with hepatocellular carcinoma
- Histopathologic consideration of hepatocellular carcinoma