Cancer Res Treat.
2021 Oct;53(4):1057-1071. 10.4143/crt.2020.1308.
Conditional Survival of Surgically Treated Patients with Lung Cancer: A Comprehensive Analyses of Overall, Recurrence-free, and Relative Survival
- Affiliations
-
- 1Department of Family Medicine, Supportive Care Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Clinical Research Design and Evaluation and, Samsung Advanced Institute for Health Sciences and Technology (SAIHST), Sungkyunkwan University, Seoul, Korea
- 3Department of Digital Health, Samsung Advanced Institute for Health Sciences and Technology (SAIHST), Sungkyunkwan University, Seoul, Korea
- 4Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 5Healthcare system Gangnan Center, Seoul National University Hospital, Seoul, Korea
- 6Cancer Education Center, Samsung Medical Center, Seoul, Korea
- 7Department of Health Sciences and Technology, Samsung Advanced Institute for Health Sciences and Technology, Sungkyunkwan University, Seoul, Korea
- 8Departments of Health, Behavior, and Society and Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA
- 9Department of Thoracic and Cardiovascular Surgery, Armed Forces Capital Hospital, Seongnam, Korea
- KMID: 2521581
- DOI: http://doi.org/10.4143/crt.2020.1308
Abstract
- Purpose
Survival probability changes over time in cancer survivors. This study examined conditional survival in patients undergoing curative resection for non-small cell lung cancer (NSCLC).
Materials and Methods
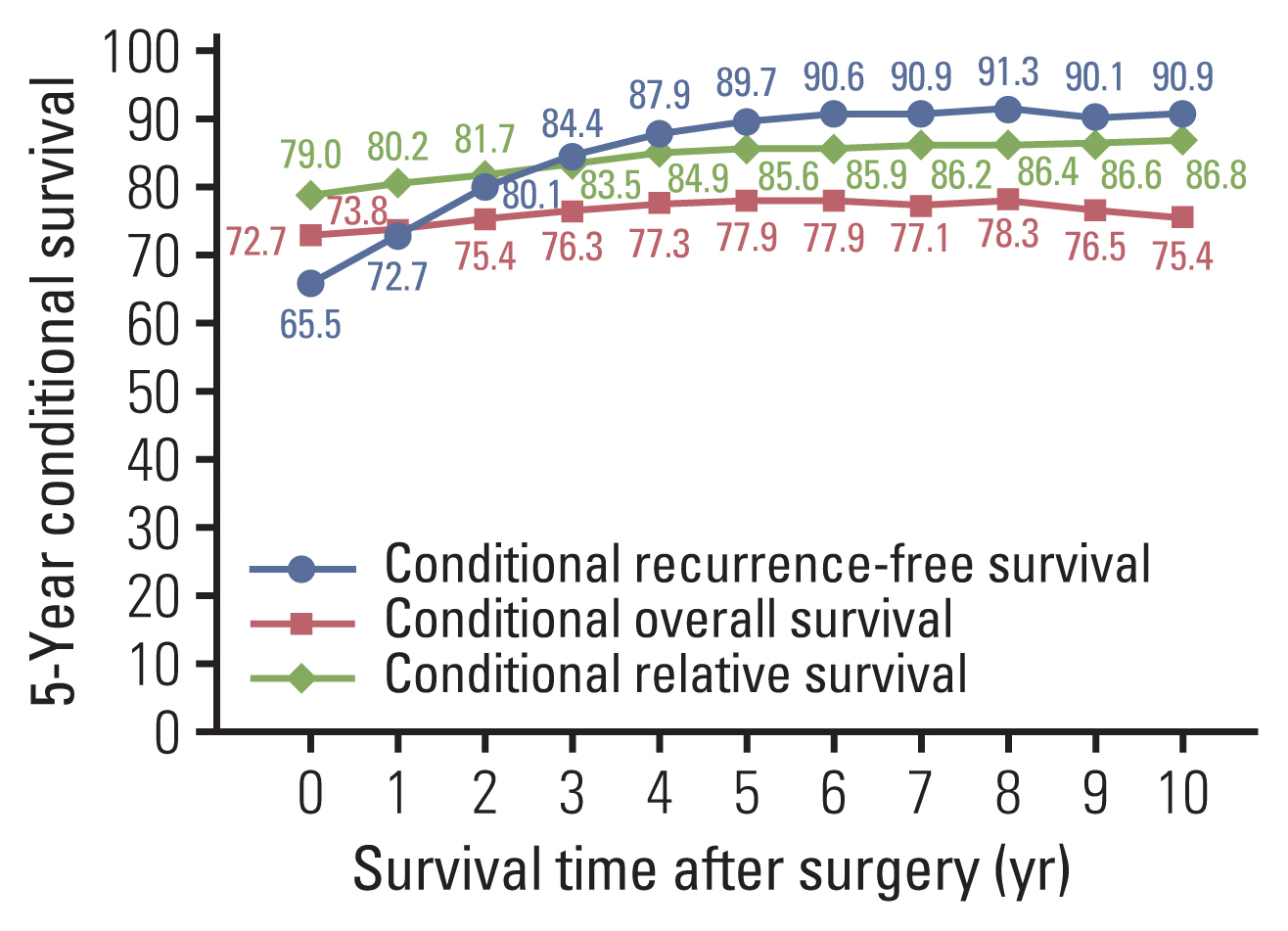
Five-year conditional recurrence-free survival (CRFS), conditional overall survival (COS), and conditional relative survival (CRS) up to 10 years after surgery were calculated in patients who underwent NSCLC resection from 1994 to 2016. These rates were stratified according to age, sex, year of diagnosis, pathological stage, tumor histology, smoking status, comorbidity, and lung function.
Results
Five-year CRFS increased from 65.6% at baseline to 90.9% at 10 years after surgery. Early differences in 5-year CRFS according to stratified patient characteristics disappeared, except for age: older patients exhibited persistently lower 5-year CRFS. Five-year COS increased from 72.7% to 78.3% at 8 years and then decreased to 75.4% at 10 years. Five-year CRS increased from 79.0% at baseline to 86.8% at 10 years. Older age and higher pathologic stage were associated with lower 5-year COS and CRS up to 10 years after surgery. Female patients, those with adenocarcinoma histology, non-smokers, patient without comorbidities and had good lung function showed higher COS and CRS.
Conclusion
CRFS improved over time, but significant risk remained after 5 years. CRS slightly improved over time but did not reach 90%, suggesting significant excess mortality compared to the general population. Age and stage remained significant predictors of conditional survival several years after surgery. Our conditional survival estimates should help clinicians and patients make informed treatment and personal life decisions based on survivorship status.
Keyword
Figure
Reference
-
References
1. Lin HT, Liu FC, Wu CY, Kuo CF, Lan WC, Yu HP. Epidemiology and survival outcomes of lung cancer: a population-based study. Biomed Res Int. 2019; 2019:8148156.
Article2. Merrill RM, Hunter BD. Conditional survival among cancer patients in the United States. Oncologist. 2010; 15:873–82.
Article3. Wang SJ, Fuller CD, Thomas CR Jr. Ethnic disparities in conditional survival of patients with non-small cell lung cancer. J Thorac Oncol. 2007; 2:180–90.
Article4. Henson DE, Ries LA. On the estimation of survival. Semin Surg Oncol. 1994; 10:2–6.
Article5. Skuladottir H, Olsen JH. Conditional survival of patients with the four major histologic subgroups of lung cancer in Denmark. J Clin Oncol. 2003; 21:3035–40.
Article6. Merrill RM, Henson DE, Barnes M. Conditional survival among patients with carcinoma of the lung. Chest. 1999; 116:697–703.
Article7. Janssen-Heijnen ML, Gondos A, Bray F, Hakulinen T, Brewster DH, Brenner H, et al. Clinical relevance of conditional survival of cancer patients in europe: age-specific analyses of 13 cancers. J Clin Oncol. 2010; 28:2520–8.
Article8. Groth SS, Rueth NM, Hodges JS, Habermann EB, Andrade RS, D’Cunha J, et al. Conditional cancer-specific versus cardiovascular-specific survival after lobectomy for stage I non-small cell lung cancer. Ann Thorac Surg. 2010; 90:375–82.
Article9. Liang Y, Fan X, Bai Y, Huang D, Yang C. Conditional survival analysis of four treatment strategies for patients with stage I non-small cell lung cancer. Oncol Lett. 2019; 18:1089–98.10. Fukui T, Okasaka T, Kawaguchi K, Fukumoto K, Nakamura S, Hakiri S, et al. Conditional survival after surgical intervention in patients with non-small cell lung cancer. Ann Thorac Surg. 2016; 101:1877–82.
Article11. Kim W, Lee HY, Jung SH, Woo MA, Kim HK, Choi YS, et al. Dynamic prognostication using conditional survival analysis for patients with operable lung adenocarcinoma. Oncotarget. 2017; 8:32201–11.
Article12. Yoo JE, Han K, Shin DW, Park SH, Cho IY, Yoon DW, et al. Conditional relative survival and competing mortality in patients who underwent surgery for lung cancer: a nationwide cohort study. Int J Cancer. 2021; 148:626–36.
Article13. Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg. 1975; 70:606–12.
Article14. Antakli T, Schaefer RF, Rutherford JE, Read RC. Second primary lung cancer. Ann Thorac Surg. 1995; 59:863–6.
Article15. Su S, Scott WJ, Allen MS, Darling GE, Decker PA, McKenna RJ, et al. Patterns of survival and recurrence after surgical treatment of early stage non-small cell lung carcinoma in the ACOSOG Z0030 (ALLIANCE) trial. J Thorac Cardiovasc Surg. 2014; 147:747–52.
Article16. Jaklitsch MT, Jacobson FL, Austin JH, Field JK, Jett JR, Keshavjee S, et al. The American Association for Thoracic Surgery guidelines for lung cancer screening using low-dose computed tomography scans for lung cancer survivors and other high-risk groups. J Thorac Cardiovasc Surg. 2012; 144:33–8.
Article17. Tsutani Y, Suzuki K, Koike T, Wakabayashi M, Mizutani T, Aokage K, et al. High-risk factors for recurrence of stage I lung adenocarcinoma: follow-up data from JCOG0201. Ann Thorac Surg. 2019; 108:1484–90.
Article18. Janssen-Heijnen ML, Houterman S, Lemmens VE, Brenner H, Steyerberg EW, Coebergh JW. Prognosis for long-term survivors of cancer. Ann Oncol. 2007; 18:1408–13.
Article19. Rich AL, Khakwani A, Free CM, Tata LJ, Stanley RA, Peake MD, et al. Non-small cell lung cancer in young adults: presentation and survival in the English National Lung Cancer Audit. QJM. 2015; 108:891–7.
Article20. Bossard N, Velten M, Remontet L, Belot A, Maarouf N, Bouvier AM, et al. Survival of cancer patients in France: a population-based study from The Association of the French Cancer Registries (FRANCIM). Eur J Cancer. 2007; 43:149–60.
Article21. Wisnivesky JP, Halm EA. Sex differences in lung cancer survival: do tumors behave differently in elderly women? J Clin Oncol. 2007; 25:1705–12.
Article22. North CM, Christiani DC. Women and lung cancer: what is new? Semin Thorac Cardiovasc Surg. 2013; 25:87–94.
Article23. Jung KW, Park S, Shin A, Oh CM, Kong HJ, Jun JK, et al. Do female cancer patients display better survival rates compared with males? Analysis of the Korean National Registry data, 2005–2009. PLoS One. 2012; 7:e52457.
Article24. Cheng TY, Cramb SM, Baade PD, Youlden DR, Nwogu C, Reid ME. The international epidemiology of lung cancer: latest trends, disparities, and tumor characteristics. J Thorac Oncol. 2016; 11:1653–71.
Article25. Tanner NT, Dai L, Bade BC, Gebregziabher M, Silvestri GA. Assessing the generalizability of the National Lung Screening Trial: comparison of patients with stage 1 disease. Am J Respir Crit Care Med. 2017; 196:602–8.
Article26. Vijayvergia N, Shah PC, Denlinger CS. Survivorship in non-small cell lung cancer: challenges faced and steps forward. J Natl Compr Canc Netw. 2015; 13:1151–61.
Article27. Yoon DW, Shin DW, Cho JH, Yang JH, Jeong SM, Han K, et al. Increased risk of coronary heart disease and stroke in lung cancer survivors: a Korean nationwide study of 20,458 patients. Lung Cancer. 2019; 136:115–21.
Article28. Ezeife DA, Leighl NB. Personalized medicine for non-small cell lung cancer: where are we now and where can we go? Expert Rev Respir Med. 2018; 12:81–2.
Article29. Wu CF, Fu JY, Yeh CJ, Liu YH, Hsieh MJ, Wu YC, et al. Recurrence risk factors analysis for stage I non-small cell lung cancer. Medicine (Baltimore). 2015; 94:e1337.
Article30. Basbug Tezel Y, Akyil M, Tezel C, Akyil FT, Evman S, Gurer D, et al. Impact of persistence of smoking on recurrence after early stage lung surgery. Eur Res J. 2016; 48:PA4339.
Article31. Jassem J. Tobacco smoking after diagnosis of cancer: clinical aspects. Transl Lung Cancer Res. 2019; 8(Suppl 1):S50–8.
Article32. Shin DW, Chun S, Kim YI, Kim SJ, Kim JS, Chong S, et al. A national survey of lung cancer specialists’ views on low-dose CT screening for lung cancer in Korea. PLoS One. 2018; 13:e0192626.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postoperative Radiation Therapy in Resected N2 Stage Non-Small Cell Lung Cancer
- Conditional relative survival of cervical cancer: a Korean National Cancer Registry Study
- The analysis of prognostic factors in endometrial cancer managed with surgical staging
- Analysis of prognositic factors and long-term survival according to the pattern of lymph node metastasis in surgically resected N2 Non-Small cell lung cancer(NSCLC)
- Pattern of Recurrence after Curative Resection of Local (Stage I and II) Non-Small Cell Lung Cancer: Difference According to the Histologic Type