J Stroke.
2021 Sep;23(3):388-400. 10.5853/jos.2021.00850.
Stroke Etiology and Outcomes after Endovascular Thrombectomy: Results from the SITS Registry and a Meta-Analysis
- Affiliations
-
- 1Department of Clinical Neuroscience, Karolinska Institute, Stockholm, Sweden
- 2Department of Research and Education, Karolinska University Hospital, Stockholm, Sweden
- 3Department of Neurology, Karolinska University Hospital, Stockholm, Sweden
- 4Department of Neurology, North Estonia Medical Centre Foundation, Tallinn, Estonia
- 5Stroke Unit, Saint Joseph's Hospital, Central Lisbon University Hospital Centre, Lisbon, Portugal
- 6Stroke Unit, University Hospital of Siena, Siena, Italy
- 7Stroke Unit, Department of Neurology, San Carlos Clinical Hospital, Madrid, Spain
- 8Stroke Unit, Tampere University Hospital, Tampere, Finland
- 9Department of Neuroscience, Neurologal Clinic, Civil Hospital of Baggiovara, University Hospital of Modena, Modena, Italy
- 10Department of Neuroradiology, Karolinska University Hospital, Stockholm, Sweden
- KMID: 2520916
- DOI: http://doi.org/10.5853/jos.2021.00850
Abstract
- Background and Purpose
The influence of stroke etiology on outcomes after endovascular thrombectomy (EVT) is not well understood. We aimed to investigate whether stroke etiology subgrouped as large artery atherosclerosis (LAA) and cardiac embolism (CE) influences outcomes in large artery occlusion (LAO) treated by EVT.
Methods
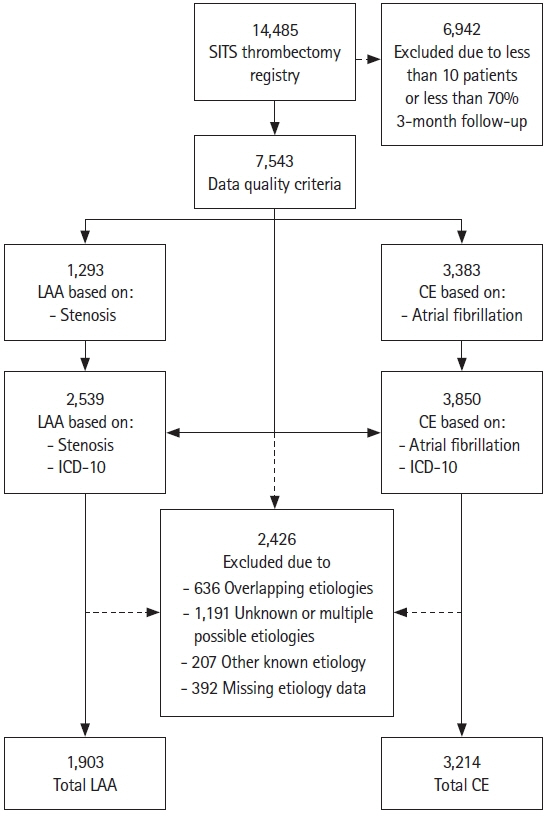
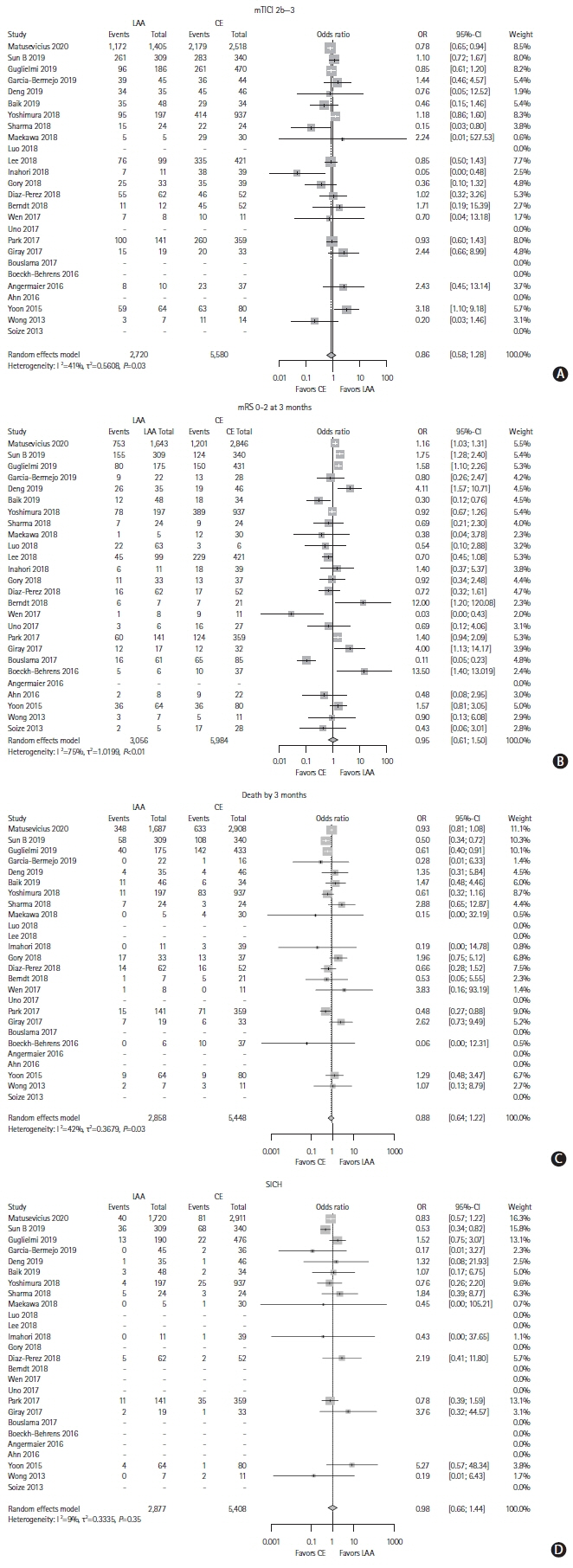
We included EVT treated LAO stroke patients registered in the Safe Implementation of Treatment in Stroke (SITS) thrombectomy register between January 1, 2014 and September 3, 2019. Primary outcome was successful reperfusion (modified Treatment in Cerebral Infarction 2b-3). Secondary outcomes were symptomatic intracranial hemorrhage (SICH), 3-month functional independence (modified Ranking Scale 0–2) and death. Multivariable logistic regression models were used for comparisons. In addition, a meta-analysis of aggregate data from the current literature was conducted (PROSPERO, ID 167447).
Results
Of 7,543 patients, 1,903 (25.2%) had LAA, 3,214 (42.6%) CE, and 2,426 (32.2%) unknown, other, or multiple etiologies. LAA patients were younger (66 vs. 74, P<0.001) and had lower National Institutes of Health Stroke Scale score at baseline (15 vs. 16, P<0.001) than CE patients. Multivariable analyses showed that LAA patients had lower odds of successful reperfusion (odds ratio [OR], 0.70; 95% confidence interval [CI], 0.57 to 0.86) and functional independence (OR, 0.74; 95% CI, 0.63 to 0.85), higher risk of death (OR, 1.44; 95% CI, 1.21 to 1.71), but no difference in SICH (OR, 1.09; 95% CI, 0.71 to 1.66) compared to CE patients. The systematic review found 25 studies matching the criteria. The meta-analysis did not find any difference between etiologies. Conclusions From the SITS thrombectomy register, we observed a lower chance of reperfusion and worse outcomes after thrombectomy in patients with LAA compared to CE etiology, despite more favorable baseline characteristics. In contrast, the meta-analysis did not find any difference between etiologies with aggregate data.
Figure
Reference
-
References
1. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article2. Campbell BCV, De Silva DA, Macleod MR, Coutts SB, Schwamm LH, Davis SM, et al. Ischaemic stroke. Nat Rev Dis Primers. 2019; 5:70.
Article3. Mustard JF, Murphy EA, Rowsell HC, Downie HG. Factors influencing thrombus formation in vivo. Am J Med. 1962; 33:621–647.
Article4. Deykin D. Thrombogenesis. N Engl J Med. 1967; 276:622–628.
Article5. Mistry EA, Mistry AM, Nakawah MO, Chitale RV, James RF, Volpi JJ, et al. Mechanical thrombectomy outcomes with and without intravenous thrombolysis in stroke patients: a meta-analysis. Stroke. 2017; 48:2450–2456.
Article6. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article7. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.8. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.9. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372:2285–2295.
Article10. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018.
Article11. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306.
Article12. Todo K, Sakai N, Imamura H, Yamagami H, Adachi H, Kono T, et al. Successful reperfusion with endovascular therapy has beneficial effects on long-term outcome beyond 90 days. Cerebrovasc Dis. 2019; 47:127–134.
Article13. Wollenweber FA, Tiedt S, Alegiani A, Alber B, Bangard C, Berrouschot J, et al. Functional outcome following stroke thrombectomy in clinical practice. Stroke. 2019; 50:2500–2506.
Article14. Giray S, Ozdemir O, Baş DF, İnanç Y, Arlıer Z, Kocaturk O. Does stroke etiology play a role in predicting outcome of acute stroke patients who underwent endovascular treatment with stent retrievers? J Neurol Sci. 2017; 372:104–109.
Article15. Guglielmi V, LeCouffe NE, Zinkstok SM, Compagne KCJ, Eker R, Treurniet KM, et al. Collateral circulation and outcome in atherosclerotic versus cardioembolic cerebral large vessel occlusion. Stroke. 2019; 50:3360–3368.16. Tsang ACO, Orru E, Klostranec JM, Yang IH, Lau KK, Tsang FCP, et al. Thrombectomy outcomes of intracranial atherosclerosis-related occlusions. Stroke. 2019; 50:1460–1466.
Article17. Wahlgren N, Ahmed N, Dávalos A, Ford GA, Grond M, Hacke W, et al. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet. 2007; 369:275–282.
Article18. Matusevicius M, Cooray C, Bottai M, Mazya M, Tsivgoulis G, Nunes AP, et al. Blood pressure after endovascular thrombectomy: modeling for outcomes based on recanalization status. Stroke. 2020; 51:519–525.19. Matusevicius M, Paciaroni M, Caso V, Bottai M, Khurana D, de Bastos M, et al. Outcome after intravenous thrombolysis in patients with acute lacunar stroke: an observational study based on SITS international registry and a meta-analysis. Int J Stroke. 2019; 14:878–886.
Article20. Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013; 44:2650–2663.21. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988; 19:604–607.
Article22. Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999; 10:37–48.
Article23. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014; 14:135.
Article24. Sun B, Shi Z, Pu J, Yang S, Wang H, Yang D, et al. Effects of mechanical thrombectomy for acute stroke patients with etiology of large artery atherosclerosis. J Neurol Sci. 2019; 396:178–183.
Article25. Deng Y, Jia B, Huo X, Peng Y, Cao Y, Chen S, et al. Association of cardioembolism and intracranial arterial stenosis with outcomes of mechanical thrombectomy in acute ischemic stroke. World Neurosurg. 2019; 121:e154–e158.
Article26. Lee JS, Lee SJ, Yoo JS, Hong JH, Kim CH, Kim YW, et al. Prognosis of acute intracranial atherosclerosis-related occlusion after endovascular treatment. J Stroke. 2018; 20:394–403.
Article27. Imahori T, Okamura Y, Sakata J, Shose H, Yokote A, Matsushima K, et al. Stent expansion and in-stent thrombus sign in the trevo stent retriever predict recanalization and possible etiology during mechanical thrombectomy: a case series of 50 patients with acute middle cerebral artery occlusion. World Neurosurg. 2019; 124:e303–e311.
Article28. Yoon W, Kim SK, Park MS, Kim BC, Kang HK. Endovascular treatment and the outcomes of atherosclerotic intracranial stenosis in patients with hyperacute stroke. Neurosurgery. 2015; 76:680–686.
Article29. Boeckh-Behrens T, Kleine JF, Zimmer C, Neff F, Scheipl F, Pelisek J, et al. Thrombus histology suggests cardioembolic cause in cryptogenic stroke. Stroke. 2016; 47:1864–1871.
Article30. Baik SH, Park HJ, Kim JH, Jang CK, Kim BM, Kim DJ. Mechanical thrombectomy in subtypes of basilar artery occlusion: relationship to recanalization rate and clinical outcome. Radiology. 2019; 291:730–737.
Article31. Garcia-Bermejo P, Patro SN, Ahmed AZ, Al Rumaihi G, Akhtar N, Kamran S, et al. Baseline occlusion angiographic appearance on mechanical thrombectomy suggests underlying etiology and outcome. Front Neurol. 2019; 10:499.
Article32. Gory B, Mazighi M, Labreuche J, Blanc R, Piotin M, Turjman F, et al. Predictors for mortality after mechanical thrombectomy of acute basilar artery occlusion. Cerebrovasc Dis. 2018; 45:61–67.
Article33. Yoshimura S, Sakai N, Uchida K, Yamagami H, Ezura M, Okada Y, et al. Endovascular therapy in ischemic stroke with acute large-vessel occlusion: recovery by endovascular salvage for cerebral ultra-acute embolism Japan registry 2. J Am Heart Assoc. 2018; 7:e008796.34. Sharma R, Llinas RH, Urrutia V, Marsh EB. Collaterals predict outcome regardless of time last known normal. J Stroke Cerebrovasc Dis. 2018; 27:971–977.
Article35. Maekawa K, Shibata M, Nakajima H, Mizutani A, Kitano Y, Seguchi M, et al. Erythrocyte-rich thrombus is associated with reduced number of maneuvers and procedure time in patients with acute ischemic stroke undergoing mechanical thrombectomy. Cerebrovasc Dis Extra. 2018; 8:39–49.
Article36. Luo G, Mo D, Tong X, Liebeskind DS, Song L, Ma N, et al. Factors associated with 90-day outcomes of patients with acute posterior circulation stroke treated by mechanical thrombectomy. World Neurosurg. 2018; 109:e318–e328.
Article37. Díaz-Pérez J, Parrilla G, Espinosa de Rueda M, Cabrera-Maqueda JM, García-Villalba B, Alba-Isasi MT, et al. Mechanical thrombectomy in acute stroke due to carotid occlusion: a series of 153 consecutive patients. Cerebrovasc Dis. 2018; 46:132–141.
Article38. Berndt M, Friedrich B, Maegerlein C, Moench S, Hedderich D, Lehm M, et al. Thrombus permeability in admission computed tomographic imaging indicates stroke pathogenesis based on thrombus histology. Stroke. 2018; 49:2674–2682.
Article39. Wen WL, Li ZF, Zhang YW, Yang PF, Simfukwe K, Fang YB, et al. Effect of baseline characteristics on the outcome of stent retriever-based thrombectomy in acute basilar artery occlusions: a single-center experience and pooled data analysis. World Neurosurg. 2017; 104:1–8.
Article40. Uno J, Kameda K, Otsuji R, Ren N, Nagaoka S, Maeda K, et al. Mechanical thrombectomy for acute basilar artery occlusion in early therapeutic time window. Cerebrovasc Dis. 2017; 44:217–224.
Article41. Park HK, Chung JW, Hong JH, Jang MU, Noh HD, Park JM, et al. Preceding intravenous thrombolysis in patients receiving endovascular therapy. Cerebrovasc Dis. 2017; 44:51–58.
Article42. Bouslama M, Haussen DC, Aghaebrahim A, Grossberg JA, Walker G, Rangaraju S, et al. Predictors of good outcome after endovascular therapy for vertebrobasilar occlusion stroke. Stroke. 2017; 48:3252–3257.
Article43. Angermaier A, Michel P, Khaw AV, Kirsch M, Kessler C, Langner S. Intravenous thrombolysis and passes of thrombectomy as predictors for endovascular revascularization in ischemic stroke. J Stroke Cerebrovasc Dis. 2016; 25:2488–2495.
Article44. Ahn SH, Hong R, Choo IS, Heo JH, Nam HS, Kang HG, et al. Histologic features of acute thrombi retrieved from stroke patients during mechanical reperfusion therapy. Int J Stroke. 2016; 11:1036–1044.
Article45. Wong EH, Yu SC, Lau AY, Hui VS, Leung CS, Hui JW, et al. Intra-arterial revascularisation therapy for acute ischaemic stroke: initial experience in a Hong Kong hospital. Hong Kong Med J. 2013; 19:135–141.46. Soize S, Barbe C, Kadziolka K, Estrade L, Serre I, Pierot L. Predictive factors of outcome and hemorrhage after acute ischemic stroke treated by mechanical thrombectomy with a stent-retriever. Neuroradiology. 2013; 55:977–987.
Article47. Tiedt S, Herzberg M, Küpper C, Feil K, Kellert L, Dorn F, et al. Stroke etiology modifies the effect of endovascular treatment in acute stroke. Stroke. 2020; 51:1014–1016.
Article48. Brinjikji W, Duffy S, Burrows A, Hacke W, Liebeskind D, Majoie CBLM, et al. Correlation of imaging and histopathology of thrombi in acute ischemic stroke with etiology and outcome: a systematic review. J Neurointerv Surg. 2017; 9:529–534.
Article49. Sporns PB, Hanning U, Schwindt W, Velasco A, Buerke B, Cnyrim C, et al. Ischemic stroke: histological thrombus composition and pre-interventional CT attenuation are associated with intervention time and rate of secondary embolism. Cerebrovasc Dis. 2017; 44:344–350.
Article50. Liebeskind DS, Sanossian N, Yong WH, Starkman S, Tsang MP, Moya AL, et al. CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke. 2011; 42:1237–1243.
Article51. De Meyer SF, Andersson T, Baxter B, Bendszus M, Brouwer P, Brinjikji W, et al. Analyses of thrombi in acute ischemic stroke: a consensus statement on current knowledge and future directions. Int J Stroke. 2017; 12:606–614.
Article52. Sporns PB, Jeibmann A, Minnerup J, Broocks G, Nawabi J, Schön G, et al. Histological clot composition is associated with preinterventional clot migration in acute stroke patients. Stroke. 2019; 50:2065–2071.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Alberta Stroke Program Early CT Score in the Prognostication after Endovascular Treatment for Ischemic Stroke: A Meta-analysis
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Differences in Effectiveness among Devices for Endovascular Thrombectomy in Patients with Acute Ischemic Stroke
- Endovascular Treatment of Acute Ischemic Stroke
- Predictive Modeling of Symptomatic Intracranial Hemorrhage Following Endovascular Thrombectomy: Insights From the Nationwide TREAT-AIS Registry