J Cerebrovasc Endovasc Neurosurg.
2021 Sep;23(3):251-259. 10.7461/jcen.2021.E2020.10.006.
Delayed intracerebral hemorrhage from a traumatic carotid-cavernous fistula associated with an enucleated orbit
- Affiliations
-
- 1Department of Neurosurgery, Neuropsychiatric Institute, University of Illinois at Chicago, Chicago, IL, USA
- KMID: 2520885
- DOI: http://doi.org/10.7461/jcen.2021.E2020.10.006
Abstract
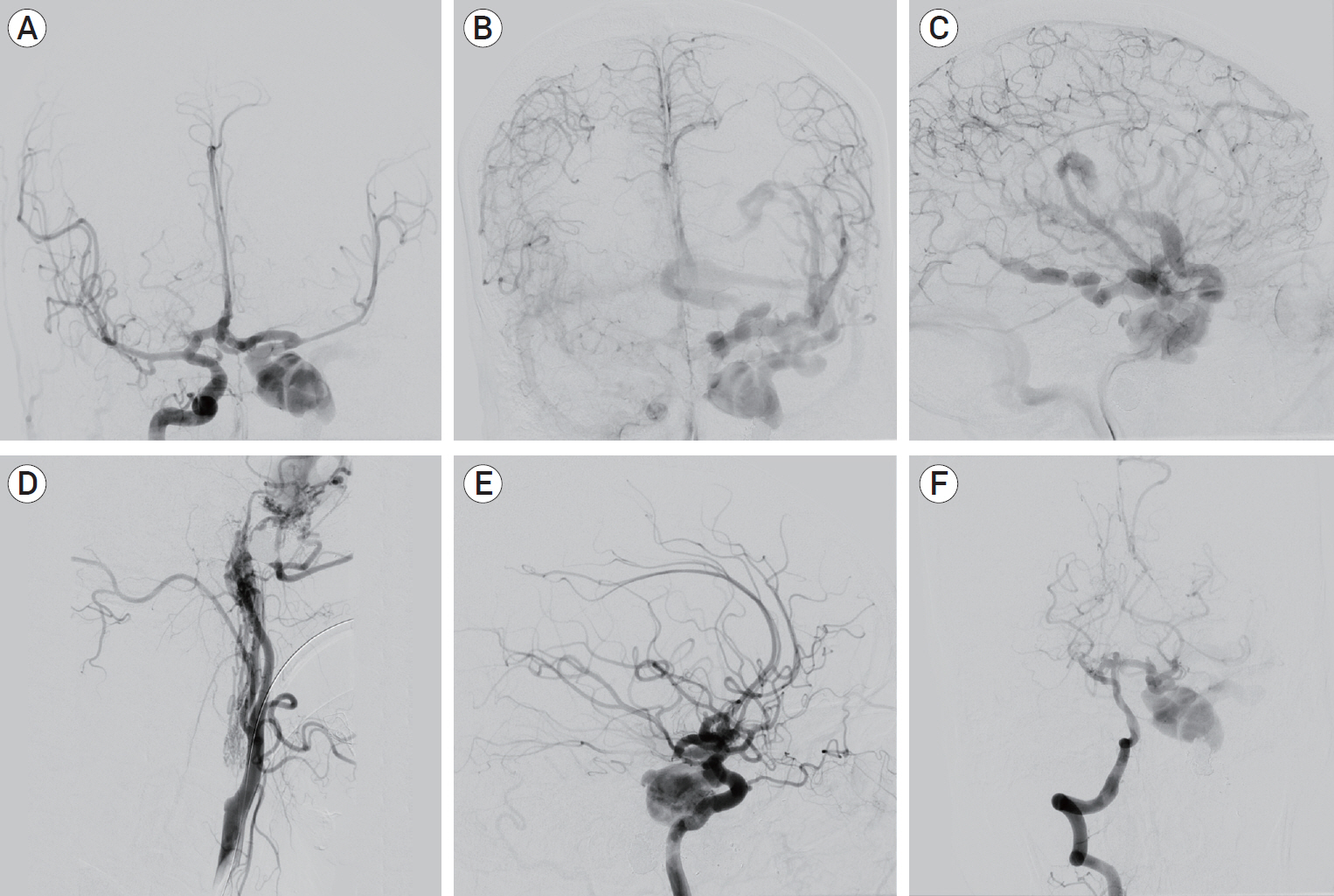
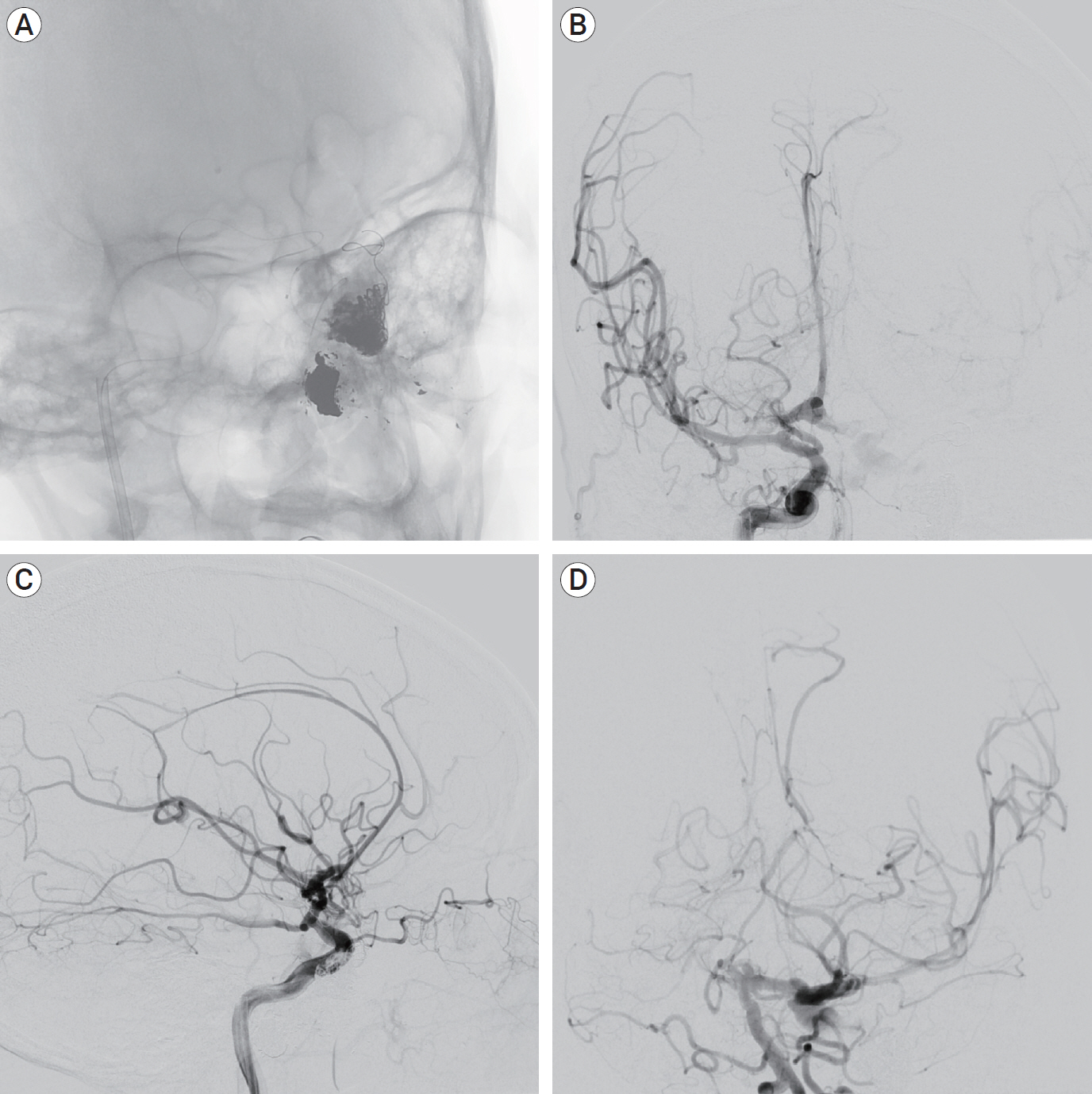
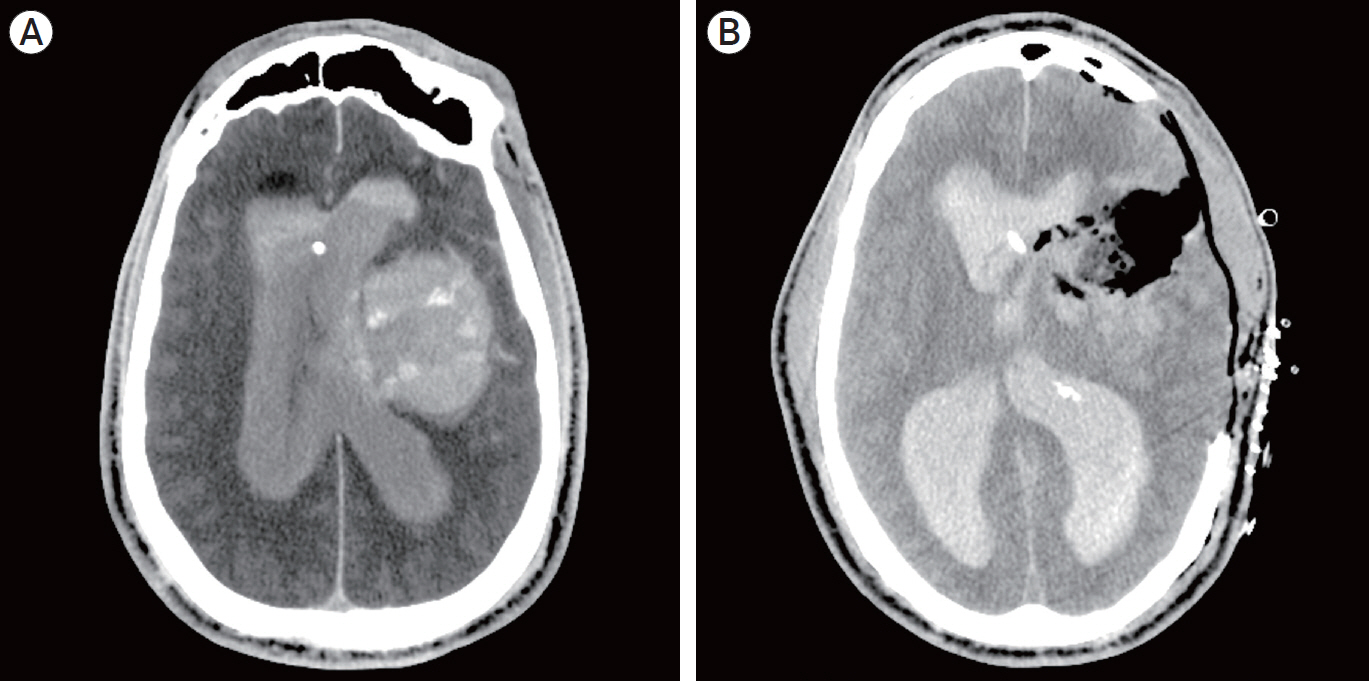
- Spontaneous intracerebral hemorrhage (ICH) from a traumatic carotid-cavernous fistula (CCF) is a rare occurrence with few cases reported in the literature. Patients classically present shortly after the inciting trauma with symptoms of ocular venous hypertension. We report a case of an ICH due to delayed rupture of a venous aneurysm from a CCF in a patient with decades-old history of enucleation of the left globe secondary to trauma with no sentinel symptoms. Our patient represents a unique presentation of a rare pathology. This case highlights the need for ongoing surveillance in patients with a history of severe craniofacial trauma, as ICH from ruptured CCF(s) demands emergent treatment due to the potential for rapid neurological deterioration.
Keyword
Figure
Reference
-
1. Al-Mufti F, Amuluru K, El-Ghanem M, Changa A, Singh P, Gandhi C, et al. Spontaneous bilateral carotid-cavernous fistulas secondary to cavernous sinus thrombosis. Neurosurgery. 2017; Apr. 80(4):646–54.
Article2. Amuluru K, Al-Mufti F, Gandhi CD, Prestigiacomo CJ, Singh IP. Direct carotid-cavernous fistula: A complication of, and treatment with, flow diversion. Interv Neuroradiol. 2016; Oct. 22(5):569–76.
Article3. Aralasmak A, Karaali K, Cevikol C, Senol U, Sindel T, Toprak H, et al. Venous drainage patterns in carotid cavernous fistulas. ISRN Radiol. 2014; Jan. 2014:760267.
Article4. Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985; Feb. 62(2):248–56.
Article5. Chan FH, Shen CY, Liu JT, Li CS. Brainstem hemorrhage caused by direct carotid-cavernous fistula. A case report and literature review. Interv Neuroradiol. 2014; Jul-Aug. 20(4):487–94.6. Chang CM, Cheng CS. Late intracranial haemorrhage and subsequent carotid-cavernous sinus fistula after fracture of the facial bones. Br J Oral Maxillofac Surg. 2013; Dec. 51(8):e296–8.
Article7. Chavan RG, Kamble RB, Bonde V. Endovascular treatment in an unusual case of direct carotid cavernous fistula. Neuroradiol J. 2014; Apr. 27(2):207–12.
Article8. D’Angelo L, Paglia F, Caporlingua A, Sampirisi L, Guidetti G, Santoro A. Atypical manifestation of direct low-flow carotid-cavernous fistula: case report and review of the literature. World Neurosurg. 2019; May. 125:456–60.9. d’Angelo VA, Monte V, Scialfa G, Fiumara E, Scotti G. Intracerebral venous hemorrhage in “high-risk” carotid-cavernous fistula. Surg Neurol. 1988; Nov. 30(5):387–90.10. Halbach VV, Hieshima GB, Higashida RT, Reicher M. Carotid cavernous fistulae: indications for urgent treatment. AJR Am J Roentgenol. 1987; Sep. 149(3):587–93.
Article11. Hayashi K, Suyama K, Nagata I. Traumatic carotid cavernous fistula complicated with intracerebral hemorrhage: case report. Neurol Med Chir (Tokyo). 2011; 51(3):214–6.12. Hiramatsu K, Utsumi S, Kyoi K, Sakaki T, Tada T, Iwasaki S, et al. Intracerebral hemorrhage in carotid-cavernous fistula. Neuroradiology. 1991; 33(1):67–9.
Article13. Imrie A, Redmond K, Leggett D. Spontaneous direct carotid-cavernous sinus fistula secondary to a persistent primitive trigeminal artery treated by trans-venous coil embolisation. Interv Neuroradiol. 2018; Oct. 24(5):567–70.
Article14. Kamio Y, Hiramatsu H, Kamiya M, Yamashita S, Namba H. Cerebellar hemorrhage due to a direct carotid-cavernous fistula after surgery for maxillary cancer. J Korean Neurosurg Soc. 2017; Jan. 60(1):89–93.
Article15. Lang M, Habboub G, Mullin JP, Rasmussen PA. A brief history of carotid-cavernous fistula. J Neurosurg. 2017; Jun. 126(6):1995–2001.
Article16. Lee CJ, Choi SW, Kim SH, Youm JY. Traumatic carotid-cavernous fistula bringing about intracerebral hemorrhage. J Korean Neurosurgc Soc. 2005; Aug. 38(2):155–7.17. Leone G, Renieri L, Enriquez-Marulanda A, Dmytriw AA, Nappini S, Laiso A, et al. Carotid cavernous fistulas and dural arteriovenous fistulas of the cavernous sinus: Validation of a new classification according to venous drainage. World Neurosurg. 2019; Aug. 128:e621–31.
Article18. Lin TK, Chang CN, Wai YY. Spontaneous intracerebral hematoma from occult carotid-cavernous fistula during pregnancy and puerperium. Case report. J Neurosurg. 1992; Apr. 76(4):714–7.19. Moon KY, Kang SD. Spontaneous intracerebral hematoma from transient occult carotid-cavernous fistula: a case report. J Korean Med Sci. 2005; Feb. 20(1):166–8.20. Nagesh CP, Mohimen A, Kannath SK, Rajan JE. Primary intraventricular haemorrhage due to rupture of giant varix of the basal vein of Rosenthal in a patient with long-standing direct CCF: angiographic features and treatment considerations. BMJ Case Rep. 2017; Nov. 2017:bcr2017013396.
Article21. Tanaka A, Fukushima T, Tomonaga M. Intracerebral hematomas in cases of dural arteriovenous malformation and carotid-cavernous fistula. Surg Neurol. 1986; Jun. 25(6):557–62.
Article22. Thomas AJ, Chua M, Fusco M, Ogilvy C, Tubbs RS, Harrigan M, et al. Proposal of venous drainage – based classification system for carotid cavernous fistulae with validity assessment in a multicenter cohort. Neurosurgery. 2015; Sep. 77(3):380–5.23. Turner DM, Vangilder JC, Mojtahedi S, Pierson EW. Spontaneous intracerebral hematoma in carotid-cavernous fistula. Report of three cases. J Neurosurg. 1983; Oct. 59(4):680–6.24. Workman MJ, Dion JE, Tong FC, Cloft HJ. Treatment of Trapped CCF by Direct Puncture of the Cavernous Sinus by Infraocular Trans-SOF Approach. Case Report and Anatomical Basis. Interv Neuroradiol. 2002; Sep. 8(3):299–304.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Traumatic Carotid-cavernous Fistula Bringing about Intracerebral Hemorrhage
- Intracerebral Hemorrhage from a Traumatic Carotid Cavernous Fistula: Case Report
- Spontaneous Intracerebral Hematoma from Transient Occult Carotid-cavernous Fistula: A Case Report
- Bilateral Traumatic Carotid-Cavernous Fistula
- Regional Cerebral Blood Flow Changes in Traumatic Carotid Cavernous Fistula During Trapping Procedure: Case Study, Preliminary Report