Diabetes Metab J.
2021 Sep;45(5):753-764. 10.4093/dmj.2020.0134.
Appraisal of Guidelines for the Management of Blood Pressure in Patients with Diabetes Mellitus: The Consensuses, Controversies and Gaps
- Affiliations
-
- 1Department of Cardiology, The First Affiliated Hospital, Sun Yat-Sen University, Guangzhou, China
- 2NHC Key Laboratory of Assisted Circulation, Sun Yat-Sen University, Guangzhou, China
- 3Department of Otorhinolaryngology, The Third Affiliated Hospital, Sun Yat-Sen University, Guangzhou, China
- KMID: 2520857
- DOI: http://doi.org/10.4093/dmj.2020.0134
Abstract
- Background
Currently available guidelines contain conflicting recommendations on the management of blood pressure (BP) in patients with diabetes mellitus (DM). Therefore, it is necessary to appraise the guidelines and summarize the agreements and differences among recommendations.
Methods
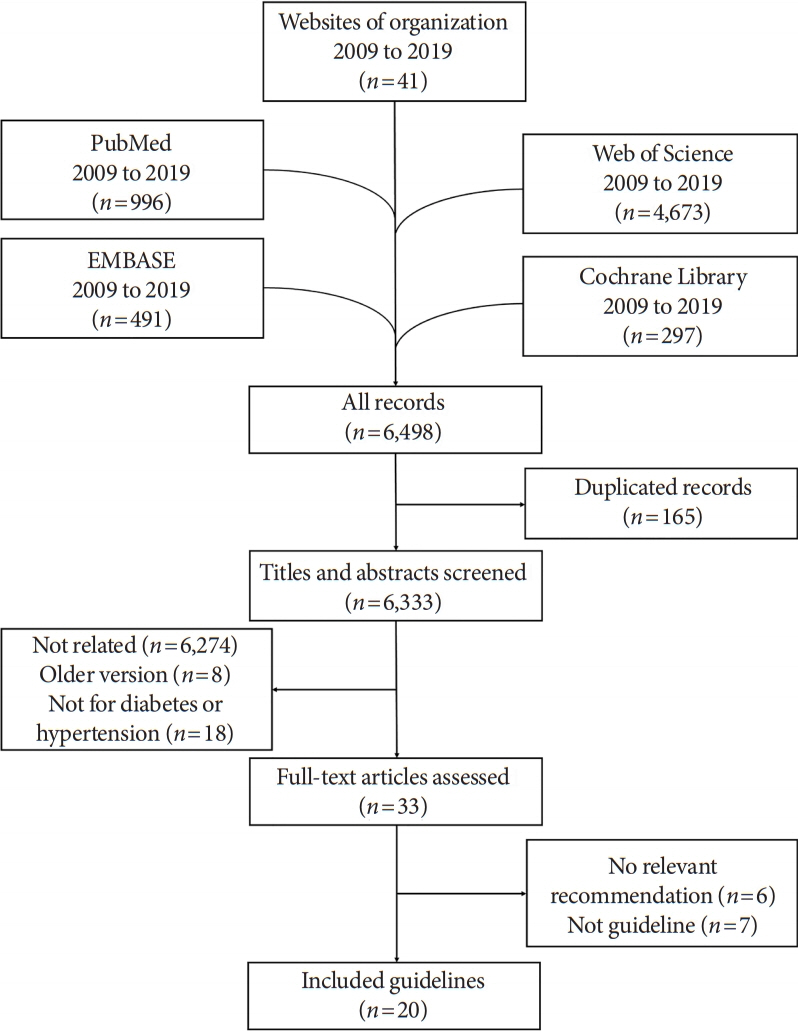
Four databases and the websites of guideline organizations were searched for guidelines regarding BP targets and thresholds for pharmacologic therapy in DM patients, and the included guidelines were appraised with the Appraisal of Guidelines for Research and Evaluation (AGREE) II instrument.
Results
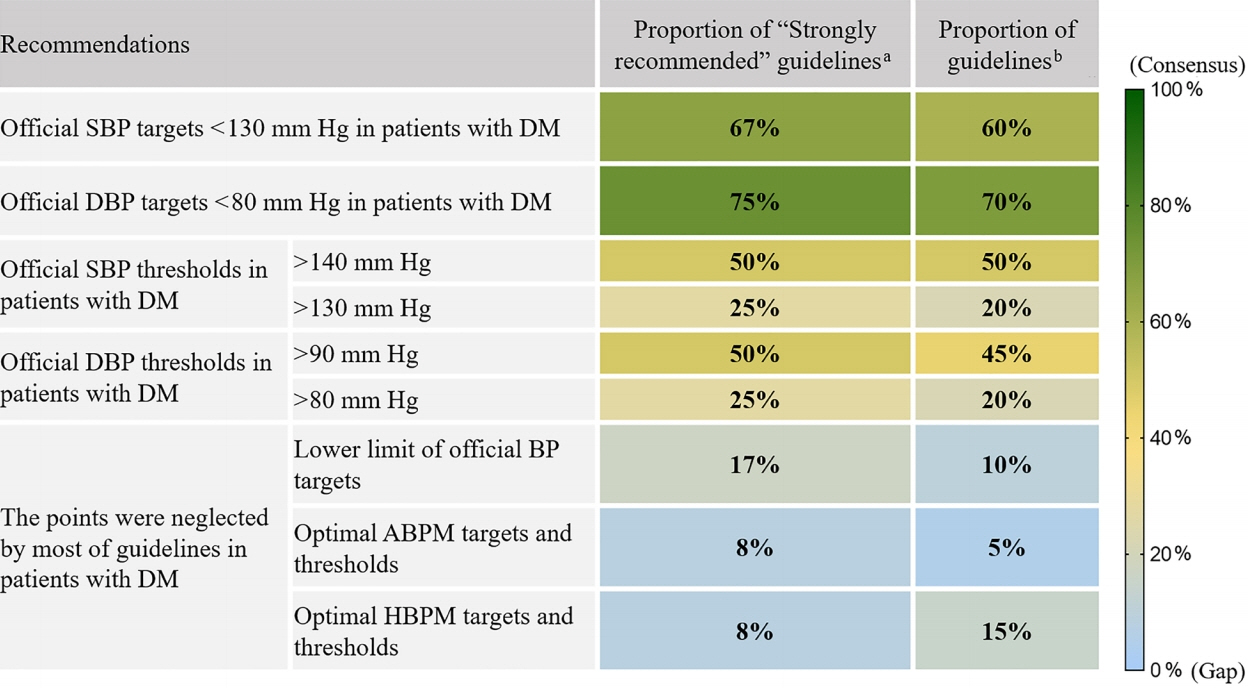
In 6,498 records identified, 20 guidelines met our inclusion criteria with 64.0% AGREE II scores (interquartile range, 48.5% to 72.0%). The scores of the European and American guidelines were superior to those of the Asian guidelines (both adjusted P<0.001). Most of the guidelines advocated systolic BP targets <130 mm Hg (12 guidelines, 60%) and diastolic BP targets <80 mm Hg (14 guidelines, 70%) in DM patients. Approximately half of the guidelines supported systolic BP thresholds >140 mm Hg (10 guidelines, 50%) and diastolic BP thresholds >90 mm Hg (nine guidelines, 45%). The tiny minority of the guidelines provided the relevant recommendations regarding the lower limit of official BP targets and the ambulatory BP monitoring (ABPM)/home BP monitoring (HBPM) targets and thresholds in DM patients.
Conclusion
The lower official BP targets (<130/80 mm Hg) in patients with DM are advocated by most of the guidelines, but they contain conflicting recommendations on the official BP thresholds. Moreover, the gaps regarding the lower limit of official BP targets and the ABPM/HBPM targets and thresholds need to be considered by future study.
Figure
Reference
-
1. The 1984 report of the Joint National Committee on detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1984; 144:1045–57.2. Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015; 313:603–15.3. Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020; 41:255–323.4. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2018; 138:e484–594.5. National Institute for Health and Care Excellence: Hypertension in adults: diagnosis and management. https://www.nice.org.uk/guidance/ng136 (coted 2021 Mar 24).6. Graham R; Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Clinical practice guidelines we can trust. Washington: National Academies Press (US);2011.
Article7. Dans AL, Dans LF. Appraising a tool for guideline appraisal (the AGREE II instrument). J Clin Epidemiol. 2010; 63:1281–2.
Article8. Ou Y, Goldberg I, Migdal C, Lee PP. A critical appraisal and comparison of the quality and recommendations of glaucoma clinical practice guidelines. Ophthalmology. 2011; 118:1017–23.
Article9. American Diabetes Association. 10. Cardiovascular disease and risk management: standards of Medical Care in Diabetes-2019. Diabetes Care. 2019; 42(Suppl 1):S103–23.10. Kim KI, Ihm SH, Kim GH, Kim HC, Kim JH, Lee HY, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part III-hypertension in special situations. Clin Hypertens. 2019; 25:19.
Article11. Lee HY, Shin J, Kim GH, Park S, Ihm SH, Kim HC, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens. 2019; 25:20.
Article12. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39:3021–104.
Article13. Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019; 42:1235–481.
Article14. Haneda M, Noda M, Origasa H, Noto H, Yabe D, Fujita Y, et al. Japanese clinical practice guideline for diabetes 2016. J Diabetes Investig. 2018; 9:657–97.
Article15. Elwyn G, Quinlan C, Mulley A, Agoritsas T, Vandvik PO, Guyatt G. Trustworthy guidelines: excellent; customized care tools. Even better. BMC Med. 2015; 13:199.
Article16. Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001; 39 (8 Suppl 2):II46–54.
Article17. Davis DA, Taylor-Vaisey A. Translating guidelines into practice. A systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ. 1997; 157:408–16.18. Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993; 342:1317–22.
Article19. Estacio RO, Jeffers BW, Gifford N, Schrier RW. Effect of blood pressure control on diabetic microvascular complications in patients with hypertension and type 2 diabetes. Diabetes Care. 2000; 23 Suppl 2:B54–64.20. ACCORD Study Group, Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010; 362:1575–85.
Article21. SPRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103–16.
Article22. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016; 387:957–67.
Article23. Bress AP, King JB, Kreider KE, Beddhu S, Simmons DL, Cheung AK, et al. Effect of intensive versus standard blood pressure treatment according to baseline prediabetes status: a post hoc analysis of a randomized trial. Diabetes Care. 2017; 40:1401–8.24. Turnbull F, Neal B, Algert C, Chalmers J, Chapman N, Cutler J, et al. Effects of different blood pressure-lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus: results of prospectively designed overviews of randomized trials. Arch Intern Med. 2005; 165:1410–9.25. Perkovic V, Rodgers A. Redefining blood-pressure targets: SPRINT starts the marathon. N Engl J Med. 2015; 373:2175–8.26. Buckley LF, Dixon DL, Wohlford GF 4th, Wijesinghe DS, Baker WL, Van Tassell BW. Intensive versus standard blood pressure control in SPRINT-eligible participants of ACCORD-BP. Diabetes Care. 2017; 40:1733–8.
Article27. Rahman F, McEvoy JW. The J-shaped curve for blood pressure and cardiovascular disease risk: historical context and recent updates. Curr Atheroscler Rep. 2017; 19:34.
Article28. Bhatt DL. Troponin and the J-curve of diastolic blood pressure: when lower is not better. J Am Coll Cardiol. 2016; 68:1723–6.29. McEvoy JW, Chen Y, Rawlings A, Hoogeveen RC, Ballantyne CM, Blumenthal RS, et al. Diastolic blood pressure, subclinical myocardial damage, and cardiac events: implications for blood pressure control. J Am Coll Cardiol. 2016; 68:1713–22.30. Vidal-Petiot E, Greenlaw N, Ford I, Ferrari R, Fox KM, Tardif JC, et al. Relationships between components of blood pressure and cardiovascular events in patients with stable coronary artery disease and hypertension. Hypertension. 2018; 71:168–76.
Article31. Vidal-Petiot E, Ford I, Greenlaw N, Ferrari R, Fox KM, Tardif JC, et al. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet. 2016; 388:2142–52.
Article32. Brunstrom M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. BMJ. 2016; 352:i717.
Article33. Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and metaanalysis. Lancet. 2016; 387:435–43.
Article34. Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006; 24:215–33.
Article35. Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007; 334:885–8.
Article36. Wijkman M, Lanne T, Engvall J, Lindstrom T, Ostgren CJ, Nystrom FH. Masked nocturnal hypertension: a novel marker of risk in type 2 diabetes. Diabetologia. 2009; 52:1258–64.37. Kamoi K, Miyakoshi M, Soda S, Kaneko S, Nakagawa O. Usefulness of home blood pressure measurement in the morning in type 2 diabetic patients. Diabetes Care. 2002; 25:2218–23.
Article38. Sakaguchi K, Horimatsu T, Kishi M, Takeda A, Ohnishi Y, Koike T, et al. Isolated home hypertension in the morning is associated with target organ damage in patients with type 2 diabetes. J Atheroscler Thromb. 2005; 12:225–31.
Article