Korean Circ J.
2021 Oct;51(10):851-862. 10.4070/kcj.2021.0116.
Electrocardiographic Manifestations in Patients with COVID-19: Daegu in South Korea
- Affiliations
-
- 1Division of Cardiology, Daegu Catholic University College of Medicine, Daegu, Korea
- 2Division of Cardiology, Daegu Fatima General Hospital, Daegu, Korea
- 3Division of Cardiology, Yeungnam University College of Medicine, Daegu, Korea
- 4Division of Cardiology, Kyungpook National University, Daegu, Korea
- 5Division of Cardiology, Keimyung University Dongsan Medical Center, Daegu, Korea
- 6Division of Cardiology, Daegu Veterans Hospital, Daegu, Korea
- 7Division of Cardiology, Kyungpook National University Chilgok Hospital, Daegu, Korea
- KMID: 2520692
- DOI: http://doi.org/10.4070/kcj.2021.0116
Abstract
- Background and Objectives
As the coronavirus disease 2019 (COVID-19) spreads worldwide, cardiac injury in patients infected with COVID-19 becomes a significant concern. Thus, this study investigates the impact of several electrocardiogram (ECG) parameters and disease severity in COVID-19 patients.
Methods
Seven medical centers in Daegu admitted 822 patients with COVID-19 between February and April 2020. This study examined 267 patients among them who underwent an ECG test and evaluated their biochemical parameters like C-reactive protein (CRP), log N-terminal pro-B-type Natriuretic Peptide (NT-proBNP), cardiac enzyme, and ECG parameters (heart rate, PR interval, QRS interval, T inversion, QT interval, and Tpe [the interval between peak to end in a T wave]).
Results
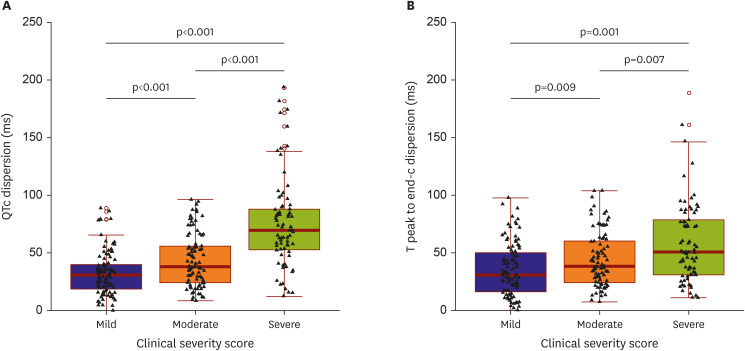
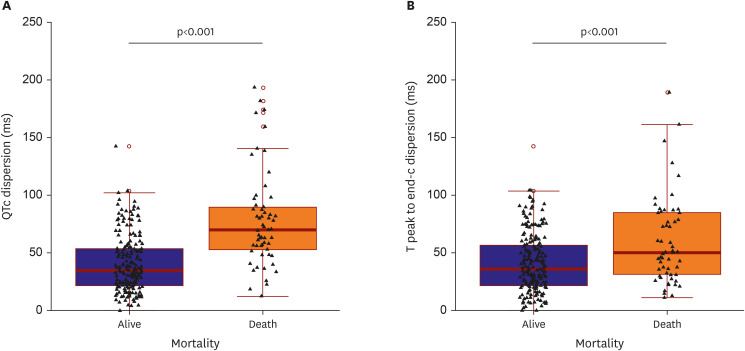
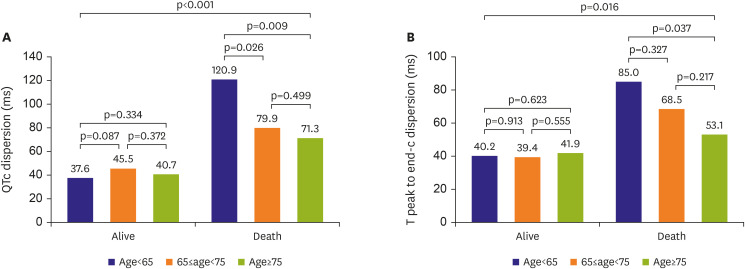
Those patients were divided into 3 groups of mild (100 patients), moderate (89 patients), and severe (78 patients) according to clinical severity score. The level of CRP, log NT-proBNP, and creatinine kinase-myocardial band were significantly increased in severe patients. Meanwhile, severe patients exhibited prolonged QT intervals (QTc) and Tpe (Tpe-c) compared to mild or moderate patients. Moreover, deceased patients (58; 21.7%) showed increased dispersion of QTc and Tpe-c compared with surviving patients (78.2±41.1 vs. 40.8±24.6 ms and 60.2±37.3 vs. 40.8±24.5 ms, both p<0.05, respectively). The QTc dispersion of more than 56.1 ms could predict the mortality in multivariate analysis (odd ratio, 11.55; 95% confidence interval, 3.746–42.306).
Conclusions
COVID-19 infections could involve cardiac injuries, especially cardiac repolarization abnormalities. A prolonged QTc dispersion could be an independent predictable factor of mortality.
Keyword
Figure
Cited by 1 articles
-
QTc Dispersion Predicts Prognosis in COVID-19 Disease
Sung-Won Jang
Korean Circ J. 2021;51(10):863-865. doi: 10.4070/kcj.2021.0275.
Reference
-
1. World Health Organization. Coronavirus disease (COVID-19) outbreak [Internet]. Geneva: World Health Organization;2020. cited 2020 September 27. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.2. Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020; 5:819–824. PMID: 32219357.
Article3. Sinkeler FS, Berger FA, Muntinga HJ, Jansen MM. The risk of QTc-interval prolongation in COVID-19 patients treated with chloroquine. Neth Heart J. 2020; 28:418–423. PMID: 32648153.
Article4. Magadum A, Kishore R. Cardiovascular manifestations of COVID-19 infection. Cells. 2020; 9:2508.
Article5. Sandoval Y, Januzzi JL Jr, Jaffe AS. Cardiac troponin for assessment of myocardial injury in COVID-19: JACC review topic of the week. J Am Coll Cardiol. 2020; 76:1244–1258. PMID: 32652195.6. Farré N, Mojón D, Llagostera M, et al. Prolonged QT interval in SARS-CoV-2 infection: prevalence and prognosis. J Clin Med. 2020; 9:2712.
Article7. Kochi AN, Tagliari AP, Forleo GB, Fassini GM, Tondo C. Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovasc Electrophysiol. 2020; 31:1003–1008. PMID: 32270559.
Article8. Sahu P, Lim PO, Rana BS, Struthers AD. QT dispersion in medicine: electrophysiological holy grail or fool's gold? QJM. 2000; 93:425–431. PMID: 10874051.
Article9. Rosenthal TM, Masvidal D, Abi Samra FM, et al. Optimal method of measuring the T-peak to T-end interval for risk stratification in primary prevention. Europace. 2018; 20:698–705. PMID: 28339886.
Article10. Tschope C, Ammirati E, Bozkurt B, et al. Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nat Rev Cardiol. 2021; 18:169–193. PMID: 33046850.
Article11. Jakhmola S, Indari O, Kashyap D, et al. Recent updates on COVID-19: a holistic review. Heliyon (Lond). 2020; 6:e05706.
Article12. Clerkin KJ, Fried JA, Raikhelkar J, et al. COVID-19 and cardiovascular disease. Circulation. 2020; 141:1648–1655. PMID: 32200663.
Article13. Frangogiannis NG. The significance of COVID-19-associated myocardial injury: how overinterpretation of scientific findings can fuel media sensationalism and spread misinformation. Eur Heart J. 2020; 41:3836–3838. PMID: 33006608.
Article14. Dou Q, Wei X, Zhou K, Yang S, Jia P. Cardiovascular manifestations and mechanisms in patients with COVID-19. Trends Endocrinol Metab. 2020; 31:893–904. PMID: 33172748.
Article15. Zhang P, Zhu L, Cai J, et al. Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020; 126:1671–1681. PMID: 32302265.
Article16. Li J, Wang X, Chen J, Zhang H, Deng A. Association of renin-angiotensin system inhibitors with severity or risk of death in patients with hypertension hospitalized for coronavirus disease 2019 (COVID-19) infection in Wuhan, China. JAMA Cardiol. 2020; 5:825–830. PMID: 32324209.
Article17. Lutz C, Maher L, Lee C, Kang W. COVID-19 preclinical models: human angiotensin-converting enzyme 2 transgenic mice. Hum Genomics. 2020; 14:20. PMID: 32498696.
Article18. Oudit GY, Kassiri Z, Jiang C, et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009; 39:618–625. PMID: 19453650.
Article19. Johansen MD, Irving A, Montagutelli X, et al. Animal and translational models of SARS-CoV-2 infection and COVID-19. Mucosal Immunol. 2020; 13:877–891. PMID: 32820248.
Article20. Viljoen C, Sliwa K, Chin A. Interpreting the need for implantable loop recorder monitoring in pregnant women at high risk of arrhythmias-reply. JAMA Cardiol. 2020; 5:1304–1305.
Article21. Öztürk F, Karaduman M, Çoldur R, İncecik Ş, Güneş Y, Tuncer M. Interpretation of arrhythmogenic effects of COVID-19 disease through ECG. Aging Male. 2020; 23:1362–1365. PMID: 32449420.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiovascular Manifestations of COVID-19
- Neurological Manifestations in Patients with COVID-19: Experiences from the Central Infectious Diseases Hospital in South Korea
- Experience of Treating Critically Ill COVID-19 Patients in Daegu, South Korea
- How to Cope with COVID-19 in Patients with Inflammatory Bowel Disease
- Skin Manifestations Following COVID-19 Vaccination: A Multicenter Case Series Study in Korea