Ann Surg Treat Res.
2021 Oct;101(4):221-230. 10.4174/astr.2021.101.4.221.
The additional analgesic effects of transverse abdominis plane block in patients receiving low-dose intrathecal morphine for minimally invasive colorectal surgery: a randomized, single-blinded study
- Affiliations
-
- 1Division of Colorectal Surgery, Department of Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Surgery, College of Medicine, Taif University, Taif, Saudi Arabia
- 3Department of Anesthesiology and Pain Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2520653
- DOI: http://doi.org/10.4174/astr.2021.101.4.221
Abstract
- Purpose
Intrathecal analgesia (ITA) and transverse abdominis plane block (TAPB) are effective pain control methods in abdominal surgery. However, there is still no gold standard for postoperative pain control in minimally invasive colorectal surgery. This study aimed to investigate whether the analgesic effect could be increased when TAPB, which can further reduce wound somatic pain, was administered in low-dose morphine ITA patients.
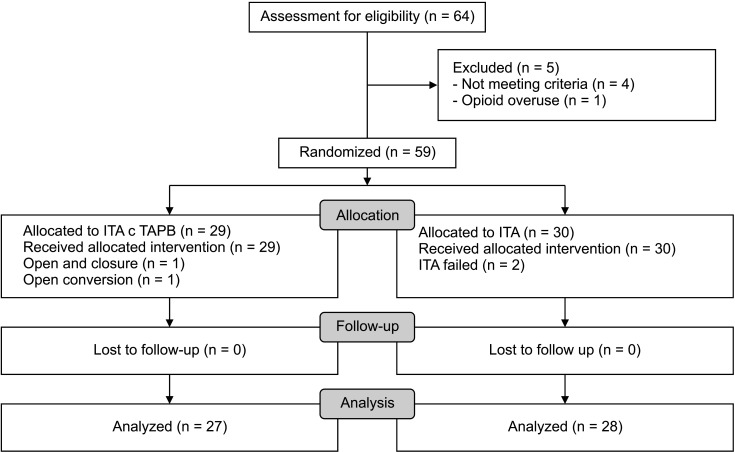
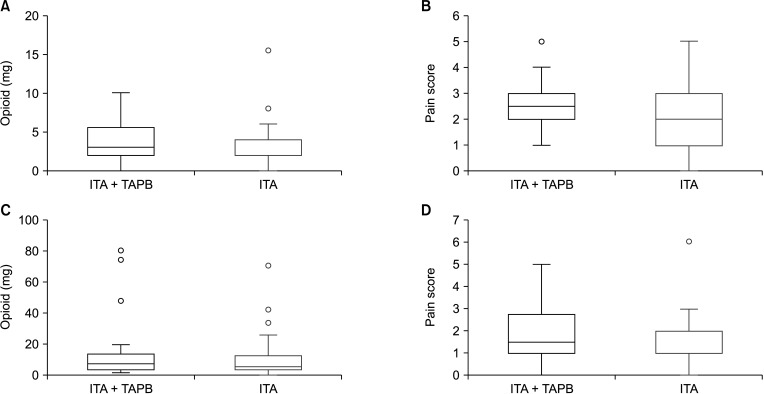
Methods
Patients undergoing elective colorectal surgery were randomized into an ITA with TAPB group or an ITA group. Patients were evaluated for pain 0, 8, 16, 24, and 48 hours after surgery. The primary outcome was the total morphine milligram equivalents administered 24 hours after surgery. The secondary outcomes were pain scores, ambulatory variables, inflammation markers, hospital stay duration, and complications within 48 hours after surgery.
Results
A total of 64 patients were recruited, and 55 were compared. There was no significant difference in morphine use over the 24 hours after surgery in the 2 groups (ITA with TAPB, 15.3 mg vs. ITA, 10.2 mg; P = 0.270). Also, there was no significant difference in pain scores. In both groups, the average pain score at 24 and 48 hours was 2 points or less, showing effective pain control.
Conclusion
ITA for pain control in patients with colorectal surgery is an effective pain method, and additional TAPB was not effective.
Keyword
Figure
Reference
-
1. Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, et al. Guidelines for perioperative care in elective colorectal surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations: 2018. World J Surg. 2019; 43:659–695. PMID: 30426190.
Article2. Levy BF, Scott MJ, Fawcett W, Fry C, Rockall TA. Randomized clinical trial of epidural, spinal or patient-controlled analgesia for patients undergoing laparoscopic colorectal surgery. Br J Surg. 2011; 98:1068–1078. PMID: 21590762.
Article3. Kim WJ, Mun JY, Kim HJ, Yoon SH, Han SR, Bae JH, et al. Surgical rectus sheath block combined with multimodal pain management reduces postoperative pain and analgesic requirement after single-incision laparoscopic appendectomy: a retrospective study. Int J Colorectal Dis. 2021; 36:75–82. PMID: 32875376.
Article4. Colibaseanu DT, Osagiede O, Merchea A, Ball CT, Bojaxhi E, Panchamia JK, et al. Randomized clinical trial of liposomal bupivacaine transverse abdominis plane block versus intrathecal analgesia in colorectal surgery. Br J Surg. 2019; 106:692–699. PMID: 30919948.
Article5. Dewinter G, Coppens S, Van de Velde M, D’Hoore A, Wolthuis A, Cuypers E, et al. Quadratus lumborum block versus perioperative intravenous lidocaine for postoperative pain control in patients undergoing laparoscopic colorectal surgery: a prospective, randomized, double-blind controlled clinical trial. Ann Surg. 2018; 268:769–775. PMID: 30004914.6. Felling DR, Jackson MW, Ferraro J, Battaglia MA, Albright JJ, Wu J, et al. Liposomal bupivacaine transversus abdominis plane block versus epidural analgesia in a colon and rectal surgery enhanced recovery pathway: a randomized clinical trial. Dis Colon Rectum. 2018; 61:1196–1204. PMID: 30192328.
Article7. Park JS, Choi GS, Kwak KH, Jung H, Jeon Y, Park S, et al. Effect of local wound infiltration and transversus abdominis plane block on morphine use after laparoscopic colectomy: a nonrandomized, single-blind prospective study. J Surg Res. 2015; 195:61–66. PMID: 25604485.
Article8. Xu YJ, Sun X, Jiang H, Yin YH, Weng ML, Sun ZR, et al. Randomized clinical trial of continuous transversus abdominis plane block, epidural or patient-controlled analgesia for patients undergoing laparoscopic colorectal cancer surgery. Br J Surg. 2020; 107:e133–e141. PMID: 31903600.
Article9. Lee CS, Park SJ, Hong SH, Shim JW, Chae MS, Han SR, et al. Clinical effect of multimodal perioperative pain management protocol for minimally invasive colorectal cancer surgery: propensity score matching study. Asian J Surg. 2021; 44:471–475. PMID: 33223452.
Article10. Wu RC, Jensen CC, Douaiher J, Madoff RD, Kwaan MR. Transversus abdominis plane block in laparoscopic colorectal surgery: a systematic review. Dis Colon Rectum. 2019; 62:1248–1255. PMID: 31490834.
Article11. Koning MV, Teunissen AJ, van der Harst E, Ruijgrok EJ, Stolker RJ. Intrathecal morphine for laparoscopic segmental colonic resection as part of an enhanced recovery protocol: a randomized controlled trial. Reg Anesth Pain Med. 2018; 43:166–173. PMID: 29219935.12. Koning MV, Klimek M, Rijs K, Stolker RJ, Heesen MA. Intrathecal hydrophilic opioids for abdominal surgery: a meta-analysis, meta-regression, and trial sequent ial analysis. Br J Anaesth. 2020; 125:358–372. PMID: 32660719.13. Kim AJ, Yong RJ, Urman RD. The role of transversus abdominis plane blocks in enhanced recovery after surgery pathways for open and laparoscopic colorectal surgery. J Laparoendosc Adv Surg Tech A. 2017; 27:909–914. PMID: 28742435.
Article14. Young J, Macpherson A, Thakerar A, Alexander M. Intrathecal morphine in postoperative analgesia for colorectal cancer surgery: a retrospective study. Pain Med. 2021; 22:402–406. PMID: 33164104.
Article15. Kong SK, Onsiong SM, Chiu WK, Li MK. Use of intrathecal morphine for postoperative pain relief after elective laparoscopic colorectal surgery. Anaesthesia. 2002; 57:1168–1173. PMID: 12437707.
Article16. Gehling M, Tryba M. Risks and side-effects of intrathecal morphine combined with spinal anaesthesia: a meta-analysis. Anaesthesia. 2009; 64:643–651. PMID: 19462494.
Article17. Sultan P, Halpern SH, Pushpanathan E, Patel S, Carvalho B. The effect of intrathecal morphine dose on outcomes after elective cesarean delivery: a meta-analysis. Anesth Analg. 2016; 123:154–164. PMID: 27089000.18. DeSousa KA, Chandran R. Intrathecal morphine for postoperative analgesia: current trends. World J Anesthesiol. 2014; 3:191–202.
Article19. Fares KM, Mohamed SA, Abdel-Ghaffar HS. High dose intrathecal morphine for major abdominal cancer surgery: a prospective double-blind, dose-finding clinical study. Pain Physician. 2014; 17:255–264. PMID: 24850107.20. Hutchins JL, Renfro L, Orza F, Honl C, Navare S, Berg AA. The addition of intrathecal morphine to a transversus abdominis plane block with liposome bupivacaine provides more effective analgesia than transversus abdominis plane block with liposome bupivacaine alone: a retrospective study. Local Reg Anesth. 2019; 12:7–13. PMID: 30863147.21. Kunopart M, Chanthong P, Thongpolswat N, Intiyanaravut T, Pethuahong C. Effects of single shot femoral nerve block combined with intrathecal morphine for postoperative analgesia: a randomized, controlled, dose-ranging study after total knee arthroplasty. J Med Assoc Thai. 2014; 97:195–202. PMID: 24765899.22. Huang YM, Lee YW, Huang YJ, Wei PL. Comparison of clinical outcomes between laparoscopic and open surgery for left-sided colon cancer: a nationwide populat ion-based study. Sci Rep. 2020; 10:75. PMID: 31919417.
Article23. Wongyingsinn M, Baldini G, Stein B, Charlebois P, Liberman S, Carli F. Spinal analgesia for laparoscopic colonic resection using an enhanced recovery after surgery programme: better analgesia, but no benefits on postoperative recovery: a randomized controlled trial. Br J Anaesth. 2012; 108:850–856. PMID: 22408272.
Article24. Ummenhofer WC, Arends RH, Shen DD, Bernards CM. Comparative spinal distribution and clearance kinetics of intrathecally administered morphine, fentanyl, alfentanil, and sufentanil. Anesthesiology. 2000; 92:739–753. PMID: 10719953.
Article25. Rodanant O, Sirichotewithayakorn P, Sriprajittichai P, Charuluxananan S. An optimal dose study of intrathecal morphine in gynecological patients. J Med Assoc Thai. 2003; 86 Suppl 2:S331–S337. PMID: 12930007.26. Yu Y, Gao S, Yuen VM, Choi SW, Xu X. The analgesic efficacy of ultrasound-guided transversus abdominis plane (TAP) block combined with oral multimodal analgesia in comparison with oral multimodal analgesia after caesarean delivery: a randomized controlled trial. BMC Anesthesiol. 2021; 21:7. PMID: 33413104.
Article27. Tomaszewski D, Bałkota M, Truszczyński A, Machowicz A. Intrathecal morphine increases the incidence of urinary retention in orthopaedic patients under spinal anaesthesia. Anaesthesiol Intensive Ther. 2014; 46:29–33. PMID: 24643924.28. Kuipers PW, Kamphuis ET, van Venrooij GE, van Roy JP, Ionescu TI, Knape JT, et al. Intrathecal opioids and lower urinary tract function: a urodynamic evaluation. Anesthesiology. 2004; 100:1497–1503. PMID: 15166570.29. Wiener JG, Gunnells D, Wood L, Chu DI, Cannon J, Kennedy GD, et al. Early removal of catheters in an Enhanced Recovery Pathway (ERP) with intrathecal opioid inject ion does not a f fect postoperative urinary outcomes. Am J Surg. 2020; 219:983–987. PMID: 31590888.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analgesic Effects and Complications of Very Low Dose Intrathecal Morphine in Postoperative Patients
- Postoperative Analgesic Effect of Combined Low Dose Intrathecal Morphine and Continuous Epidural Opioid Local Anesthetic Mixture after Lumbar Laminectomy
- Study the Effects of Intrathecal Injection of Morphine on Post-operative Pain Relief and Segmental Block Effect
- Wound infiltration or transversus abdominis plane block after laparoscopic radical prostatectomy: a randomized clinical trial
- The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy