J Pathol Transl Med.
2021 Sep;55(5):349-354. 10.4132/jptm.2020.05.17.
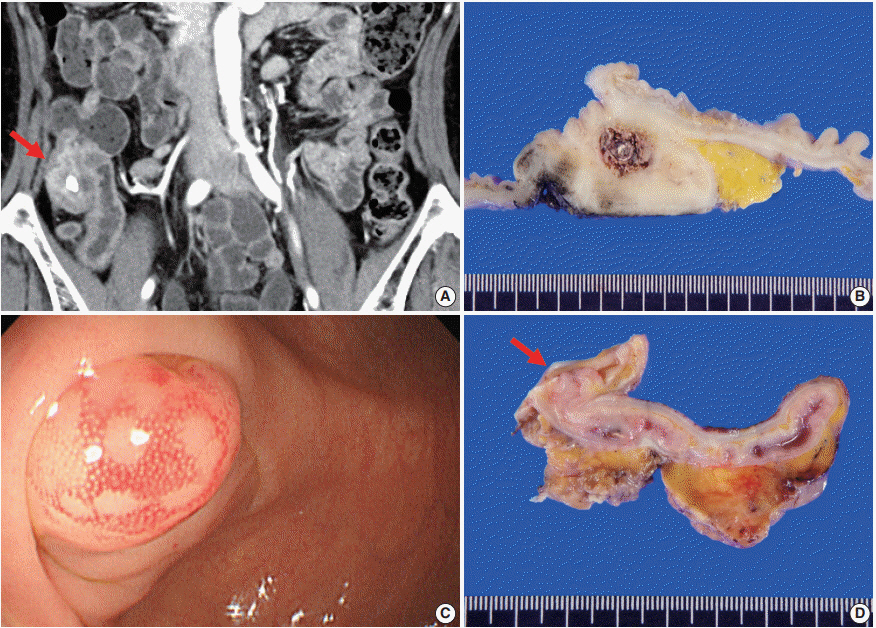
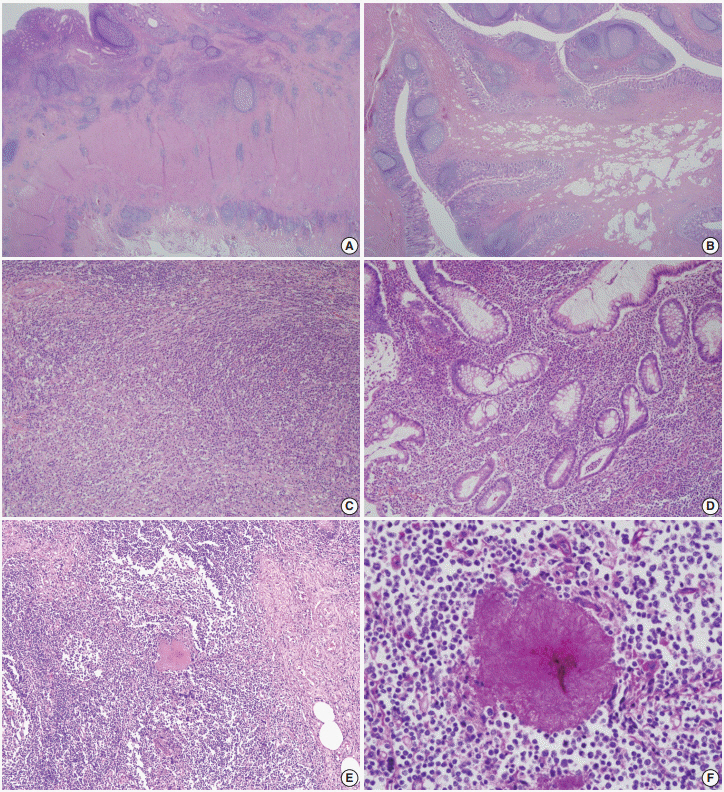
Appendiceal actinomycosis mimicking appendiceal tumor, appendicitis or inflammatory bowel disease
- Affiliations
-
- 1Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2520174
- DOI: http://doi.org/10.4132/jptm.2020.05.17
Abstract
- Appendiceal actinomycosis is very rare and its diagnosis is often difficult even in surgically resected specimens. Here we report two cases of appendiceal actinomycosis confirmed by pathologic examination of surgically resected specimens. Characteristic histologic features included transmural chronic inflammation with Crohn-like lymphoid aggregates and polypoid mucosal protrusion into cecal lumen through fibrous expansion of the submucosa. Chronic active inflammation involved the mucosa of the appendix and cecum around the appendiceal orifice. Crohn’s disease with predominant cecal involvement and inflammatory pseudotumor were considered as differential diagnoses. Careful examination revealed a few actinomycotic colonies in the mucosa, confirming the diagnosis. A high index of suspicion with awareness of the characteristic histologic features might prompt careful inspection for the actinomycotic colonies, leading to the appropriate diagnosis of this rare disease.
Keyword
Figure
Reference
-
References
1. Lee SY, Kwon HJ, Cho JH, et al. Actinomycosis of the appendix mimicking appendiceal tumor: a case report. World J Gastroenterol. 2010; 16:395–7.
Article2. Yeguez JF, Martinez SA, Sands LR, Hellinger MD. Pelvic actinomycosis presenting as malignant large bowel obstruction: a case report and a review of the literature. Am Surg. 2000; 66:85–90.3. Cintron JR, Del Pino A, Duarte B, Wood D. Abdominal actinomycosis. Dis Colon Rectum. 1996; 39:105–8.
Article4. Garner JP, Macdonald M, Kumar PK. Abdominal actinomycosis. Int J Surg. 2007; 5:441–8.
Article5. Gomez-Torres GA, Ortega-Garcia OS, Gutierrez-Lopez EG, et al. A rare case of subacute appendicitis, actinomycosis as the final pathology reports: a case report and literature review. Int J Surg Case Rep. 2017; 36:46–9.6. Lee IJ, Ha HK, Park CM, et al. Abdominopelvic actinomycosis involving the gastrointestinal tract: CT features. Radiology. 2001; 220:76–80.
Article7. Liu K, Joseph D, Lai K, Kench J, Ngu MC. Abdominal actinomycosis presenting as appendicitis: two case reports and review. J Surg Case Rep. 2016; 2016:rjw068.
Article8. Atalaia-Martins C, Cotrim I, Alves P. Appendiceal tumor or something more? Gastroenterology. 2018; 154:e14–5.
Article9. Nissotakis C, Sakorafas GH, Koureta T, Revelos K, Kassaras G, Peros G. Actinomycosis of the appendix: diagnostic and therapeutic considerations. Int J Infect Dis. 2008; 12:562–4.
Article10. Karagulle E, Turan H, Turk E, Kiyici H, Yildirim E, Moray G. Abdominal actinomycosis mimicking acute appendicitis. Can J Surg. 2008; 51:E109–10.11. Koren R, Dekel Y, Ramadan E, Veltman V, Dreznik Z. Periappendiceal actinomycosis mimicking malignancy report of a case. Pathol Res Pract. 2002; 198:441–3.
Article12. Ng N, Ng G, Davis BR, Meier DE. Actinomyces appendicitis: diagnostic dilemma--malignancy or infection? Am Surg. 2014; 80:E33–5.
Article13. Karakus E, Mambet E, Azili MN, Gulhan B, Tiryaki T, Tezer H. Actinomycosis of the appendix in childhood- an unusual cause of appendicitis. APSP J Case Rep. 2014; 5:26.14. Lee KS, Tang LH, Shia J, et al. Goblet cell carcinoid neoplasm of the appendix: clinical and CT features. Eur J Radiol. 2013; 82:85–9.
Article15. Maternini M, Saucy F, Sandmeier D, Vuilleumier H. Simple appendicitis? Can J Surg. 2008; 51:E54–5.16. DeKoning EP. Simple appendicitis?. In : Tintinalli JE, Stapczynski JS, Ma OJ, editors. Tintinalli’s emergency medicine: a comprehensive study guide. 7th ed. New York: The McGraw-Hill Companies;2011. p. 574–8.17. Piper MH, Schaberg DR, Ross JM, Shartsis JM, Orzechowski RW. Endoscopic detection and therapy of colonic actinomycosis. Am J Gastroenterol. 1992; 87:1040–2.