Ann Surg Treat Res.
2021 Sep;101(3):131-139. 10.4174/astr.2021.101.3.13.
Comparison of clinicopathological characteristics and prognosis in breast cancer patients with different Breast Imaging Reporting and Data System categories
- Affiliations
-
- 1Department of Surgery, Daejeon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Daejeon, Korea
- 2Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Surgery, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea
- 4Department of Surgery, National Cancer Center, Goyang, Korea
- 5Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea
- 6Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 7Department of Surgery, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- KMID: 2519843
- DOI: http://doi.org/10.4174/astr.2021.101.3.13
Abstract
- Purpose
The Breast Imaging Reporting and Data System (BI-RADS) is a systematic and standardized scheme of the radiological findings of breast. However, there were different BI-RADS categories between breast cancers as the clinical characteristics in previous studies. We analyzed the association of BI-RADS categories with the clinicopathological characteristics and prognosis of breast cancer.
Methods
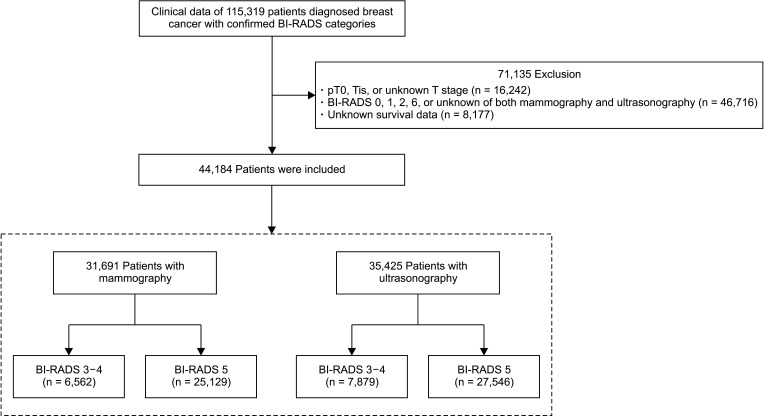
A total of 44,184 patients with invasive breast cancers assigned to BI-RADS category 3, 4, or 5 in preoperative mammography or ultrasonography were analyzed retrospectively using large-scale data from the Korean Breast Cancer Society registration system. The difference in the clinicopathological factors and prognoses according to the BI-RADS categories (BI-RADS 3–4 and BI-RADS 5) were compared between the mammography and ultrasonography groups. Comparisons of the clinicopathological factors in both groups were made using logistic regression analysis, while the prognoses were based on the breast cancer-specific survival using the Kaplan-Meier method and Cox proportional hazards model.
Results
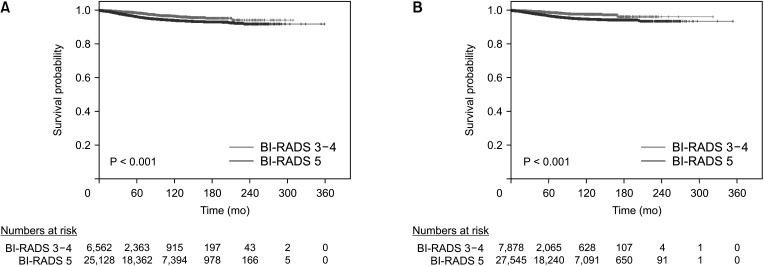
The factors associated with BI-RADS were T stage, N stage, palpability, histology grade, and lymphovascular invasion in the mammography group; and N stage, palpability, histology grade, and lymphovascular invasion in the ultrasonography group. In the survival analysis, there were significant differences in the breast cancer-specific survival of the BI-RADS category groups in both of the mammography (hazard ratio [HR], 3.366; P < 0.001) and ultrasonography (HR, 2.877; P < 0.001) groups.
Conclusion
In this study, the BI-RADS categories of preoperative mammography and ultrasonography of patients with invasive breast cancer were associated with prognosis and could be an important factor in making treatment decisions.
Figure
Reference
-
1. Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019; 144:1941–1953. PMID: 30350310.
Article2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424. PMID: 30207593.
Article3. Hong S, Won YJ, Park YR, Jung KW, Kong HJ, Lee ES, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat. 2020; 52:335–350. PMID: 32178489.
Article4. Kang SY, Kim YS, Kim Z, Kim HY, Kim HJ, Park S, et al. Breast cancer statistics in Korea in 2017: data from a breast cancer registry. J Breast Cancer. 2020; 23:115–128. PMID: 32395372.
Article5. Ko BS, Noh WC, Kang SS, Park BW, Kang EY, Paik NS, et al. Changing patterns in the clinical characteristics of Korean breast cancer from 1996-2010 using an online nationwide breast cancer database. J Breast Cancer. 2012; 15:393–400. PMID: 23346167.
Article6. Shin HR, Joubert C, Boniol M, Hery C, Ahn SH, Won YJ, et al. Recent trends and patterns in breast cancer incidence among Eastern and Southeastern Asian women. Cancer Causes Control. 2010; 21:1777–1785. PMID: 20559704.
Article7. Rao AA, Feneis J, Lalonde C, Ojeda-Fournier H. A pictorial review of changes in the BI-RADS fifth edition. Radiographics. 2016; 36:623–639. PMID: 27082663.
Article8. Lo JY, Markey MK, Baker JA, Floyd CE Jr. Cross-institutional evaluation of BI-RADS predictive model for mammographic diagnosis of breast cancer. AJR Am J Roentgenol. 2002; 178:457–463. PMID: 11804918.
Article9. D'Ors CJ. ACR BI-RADS atlas: breast imaging reporting and data system. Reston (VA): American College of Radiology;2013.10. Kim JY, Jung EJ, Park T, Jeong SH, Jeong CY, Ju YT, et al. Prognostic importance of ultrasound BI-RADS classification in breast cancer patients. Jpn J Clin Oncol. 2015; 45:411–415. PMID: 25670765.
Article11. Park EH, Min SY, Kim Z, Yoon CS, Jung KW, Nam SJ, et al. Basic facts of breast cancer in Korea in 2014: the 10-year overall survival progress. J Breast Cancer. 2017; 20:1–11. PMID: 28382089.
Article12. Min SY, Kim Z, Hur MH, Yoon CS, Park EH, Jung KW, et al. The basic facts of Korean breast cancer in 2013: results of a nationwide survey and breast cancer registry database. J Breast Cancer. 2016; 19:1–7. PMID: 27066090.
Article13. Tamaki K, Ishida T, Miyashita M, Amari M, Ohuchi N, Tamaki N, et al. Correlation between mammographic findings and corresponding histopathology: potential predictors for biological characteristics of breast diseases. Cancer Sci. 2011; 102:2179–2185. PMID: 21895869.
Article14. Xu J, Li F, Chang F. Correlation of the ultrasound imaging of breast cancer and the expression of molecular biological indexes. Pak J Pharm Sci. 2017; 30(4 Suppl):1425–1430. PMID: 29043992.15. Rashmi S, Kamala S, Murthy SS, Kotha S, Rao YS, Chaudhary KV. Predicting the molecular subtype of breast cancer based on mammography and ultrasound findings. Indian J Radiol Imaging. 2018; 28:354–361. PMID: 30319215.
Article16. Cen D, Xu L, Li N, Chen Z, Wang L, Zhou S, et al. BI-RADS 3-5 microcalcifications can preoperatively predict breast cancer HER2 and Luminal a molecular subtype. Oncotarget. 2017; 8:13855–13862. PMID: 28099938.
Article17. Ye DM, Li Q, Yu T, Wang HT, Luo YH, Li WQ. Clinical and epidemiologic factors associated with breast cancer and its subtypes among Northeast Chinese women. Cancer Med. 2019; 8:7431–7445. PMID: 31642614.
Article18. Blaichman J, Marcus JC, Alsaadi T, El-Khoury M, Meterissian S, Mesurolle B. Sonographic appearance of invasive ductal carcinoma of the breast according to histologic grade. AJR Am J Roentgenol. 2012; 199:W402–W408. PMID: 22915433.
Article19. Au FW, Ghai S, Lu FI, Moshonov H, Crystal P. Histological grade and immunohistochemical biomarkers of breast cancer: correlation to ultrasound features. J Ultrasound Med. 2017; 36:1883–1894. PMID: 28556296.
Article20. Liu Z, Li R, Liang K, Chen J, Chen X, Li X, et al. Value of digital mammography in predicting lymphovascular invasion of breast cancer. BMC Cancer. 2020; 20:274. PMID: 32245448.
Article21. Li JW, Tong YY, Zhou J, Shi ZT, Sun PX, Chang C. Tumor proliferation and invasiveness derived from ultrasound appearances of invasive breast cancers: moving beyond the routine differential diagnosis. J Ultrasound Med. 2020; 39:1589–1599. PMID: 32118315.22. Mahoney L, Csima A. Efficiency of palpation in clinical detection of breast cancer. Can Med Assoc J. 1982; 127:729–730. PMID: 7139488.23. Warren SL, Bhutiani N, Agle SC, Martin RC 2nd, McMasters KM, Ajkay N. Differences between palpable and nonpalpable tumors in early-stage, hormone receptor-positive breast cancer. Am J Surg. 2018; 216:326–330. PMID: 29502856.
Article24. Skinner KA, Silberman H, Sposto R, Silverstein MJ. Palpable breast cancers are inherently different from nonpalpable breast cancers. Ann Surg Oncol. 2001; 8:705–710. PMID: 11597010.
Article25. Brouckaert O, Schoneveld A, Truyers C, Kellen E, Van Ongeval C, Vergote I, et al. Breast cancer phenotype, nodal status and palpability may be useful in the detection of overdiagnosed screening-detected breast cancers. Ann Oncol. 2013; 24:1847–1852. PMID: 23680691.
Article26. Rosenberg RD, Hunt WC, Williamson MR, Gilliland FD, Wiest PW, Kelsey CA, et al. Effects of age, breast density, ethnicity, and estrogen replacement therapy on screening mammographic sensitivity and cancer stage at diagnosis: review of 183,134 screening mammograms in Albuquerque, New Mexico. Radiology. 1998; 209:511–518. PMID: 9807581.
Article27. Mandelson MT, Oestreicher N, Porter PL, White D, Finder CA, Taplin SH, et al. Breast density as a predictor of mammographic detection: comparison of interval- and screen-detected cancers. J Natl Cancer Inst. 2000; 92:1081–1087. PMID: 10880551.
Article28. Stacey-Clear A, McCarthy KA, Hall DA, Pile-Spellman E, White G, Hulka CA, et al. Mammographically detected breast cancer: location in women under 50 years old. Radiology. 1993; 186:677–680. PMID: 8381550.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Breast Imaging Reporting and Data System (BI-RADS): Advantages and Limitations
- Validity of Breast Cancer Symptom Questionnaire and Its Relationship With Breast Ultrasonography in Young Female Night Workers
- Shear-wave elastography in breast ultrasonography: the state of the art
- Thyroid Imaging Reporting and Data System (TIRADS)
- Histological Analysis of Benign Breast Imaging Reporting and Data System Categories 4c and 5 Breast Lesions in Imaging Study